Patient is a 47-year-old male with a past medical history significant for hypertension and obesity who presents to clinic with shortness of breath, swelling of both lower extremities and abdomen as well as intermittent low-grade fevers. Prior to clinic presentation (8 months prior), he was seen at an outside health care facility where he underwent an extensive work-up including computed tomography (CT) of his chest/abdomen/pelvis as well as echocardiogram. He was found to have a small pericardial effusion at that time. He was also found to have an elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). He was ultimately diagnosed with viral pericarditis and treated with colchicine, ibuprofen, and oral Lasix. He was monitored locally and was found to have improving inflammatory markers but unfortunately had worsening volume overload and was admitted to his local hospital with decompensated heart and renal failure. He underwent a right heart catheterization during this admission revealing elevated right and left sided intra-cardiac filling pressures with a preserved cardiac index. His pericardial effusion was found to be enlarging for which he underwent a pericardial window with 400 cc of fluid drained. Tissue biopsy from the pericardium revealed chronic fibrous constrictive pericarditis and chronic lymphocytic pericarditis. At that time he was diuresed to euvolemia and discharged home with a 6-month prednisone taper. Colchicine and ibuprofen were discontinued due to renal failure. His symptoms significantly improved while taking prednisone. Unfortunately, his symptoms recurred after finishing the prednisone for which he presented to Cleveland Clinic for a second opinion.
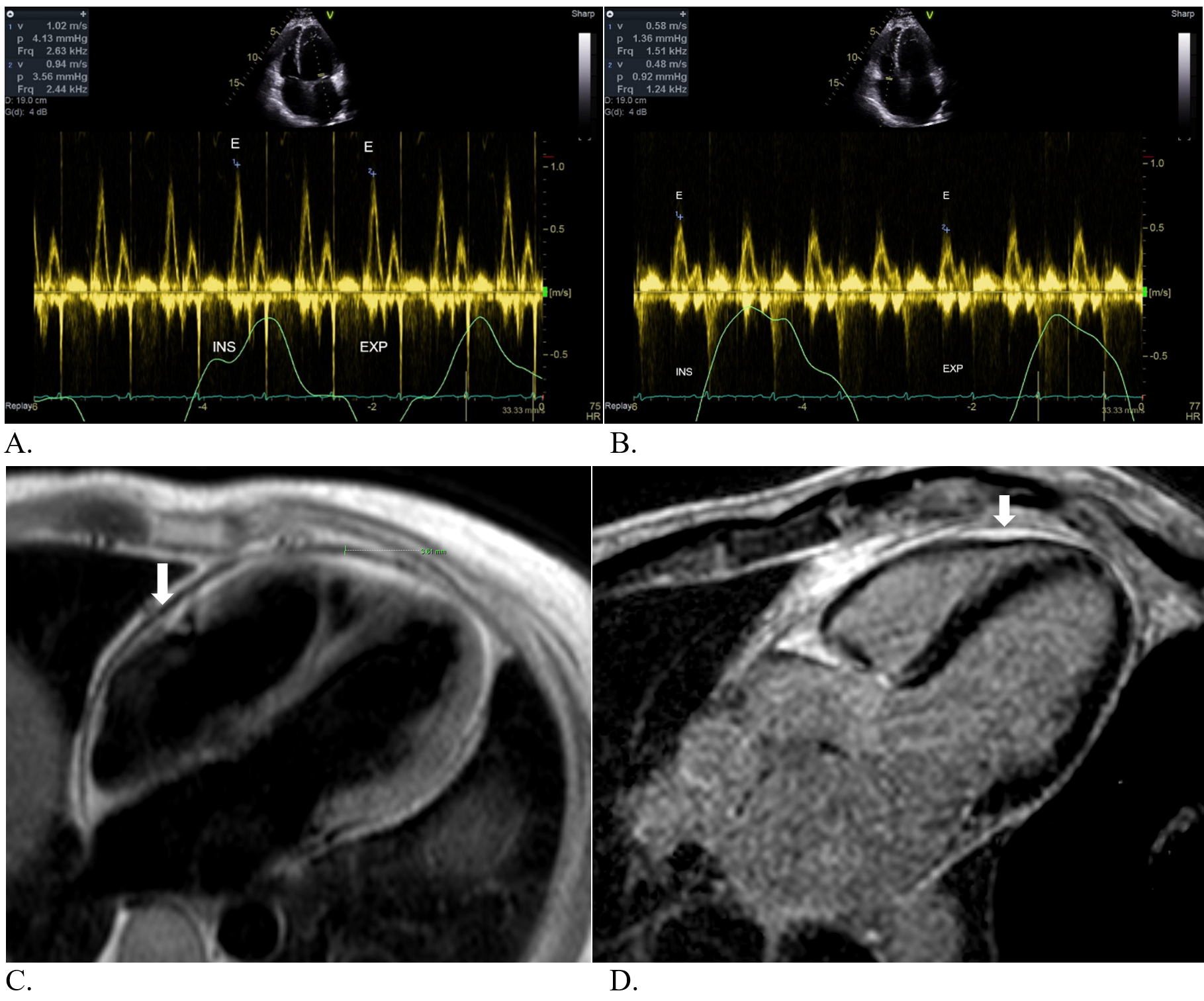
Laboratory work-up while in clinic revealed normal white blood cell, hemoglobin and platelet counts. His creatinine was found to be back to his baseline at 0.96 mg/dL. He had an NT-ProBNP that was obtained and was elevated at 653 pg/mL (<125 pg/mL). ESR and ultra-sensitive CRP were both elevated with values of 29 mm/hr (0-15 mm/hr) and 87.3 mg/L (<3.1 mg/L), respectively. Echocardiogram was obtained revealing preserved biventricular size and function with a dilated inferior vena cava (IVC), mild septal bounce and mild respiratory variation of mitral and tricuspid inflows, 8.0% and 17.0%, respectively (Figure 1: A and B). Lastly, he underwent cardiac magnetic resonance imaging (MRI) which revealed a moderate circumferential pericardial delayed enhancement and increased pericardial signal on T2 STIR imaging indicative of pericardial edema. There were findings also of a mild septal bounce, mild pericardial thickening and a dilated IVC (Figure 1: C and D).
Figure 1
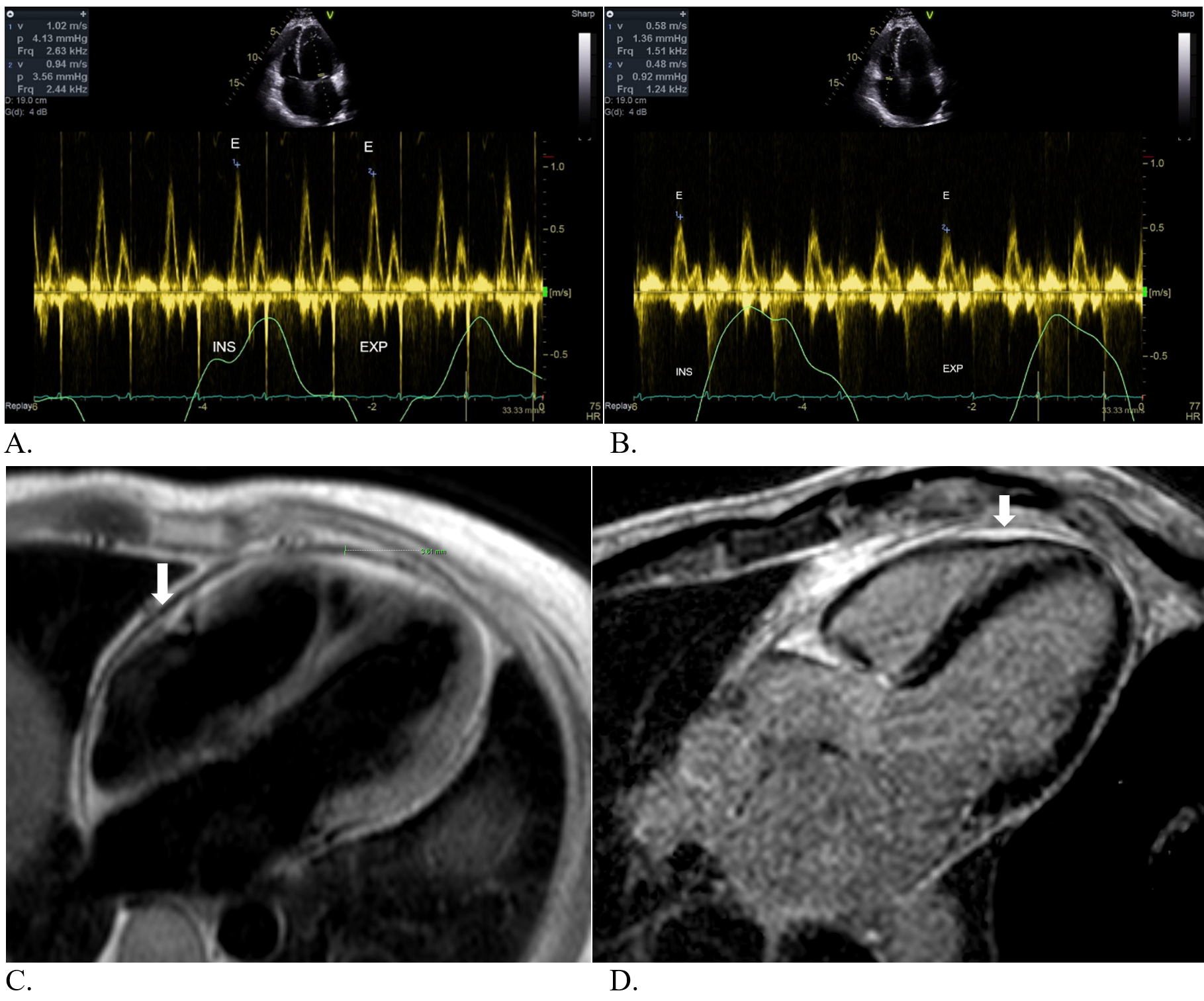 Figure 1: A: Mild variation of mitral inflow Doppler. B: Mild variation of tricuspid inflow Doppler. C: Mild pericardial thickening on axial black blood images. D: Delayed pericardial enhancement, particularly around the right ventricle (arrow).
Figure 1: A: Mild variation of mitral inflow Doppler. B: Mild variation of tricuspid inflow Doppler. C: Mild pericardial thickening on axial black blood images. D: Delayed pericardial enhancement, particularly around the right ventricle (arrow).
Figure 1: A: Mild variation of mitral inflow Doppler. B: Mild variation of tricuspid inflow Doppler. C: Mild pericardial thickening on axial black blood images. D: Delayed pericardial enhancement, particularly around the right ventricle (arrow).
The correct answer is: B. Resume prednisone taper for 4 weeks with the addition of twice daily colchicine.
The patient has signs and symptoms concerning for constrictive pericarditis given his presentation of right sided volume overload in conjunction with findings seen on echocardiography and cardiac MRI. He was trialed on a long taper of prednisone with significant improvement in his symptoms but unfortunately his symptoms recurred after cessation of therapy. Taking all of this into consideration, transient constriction is very high on the differential given the spectrum of constrictive pericarditis. Transient constrictive pericarditis is a variant of constrictive pericarditis that is now recognized as a diagnosis. This clinical entity can be reversible and overall has a better prognosis when compared to those with chronic constrictive pericarditis. It is estimated that transient constriction represents 9-17% of all constrictive pericarditis cases.1,2 The pathophysiology behind transient constriction is felt to be a result of fluctuating pericardial edema and inflammation rather than fixed pericardial fibrosis or calcification.1,3 The important concept here is that patients that are suspected of having transient constriction based on the clinical picture should be trialed with anti-inflammatory drugs for at least 3-6 months prior to consideration for pericardiectomy.1-3 In our current patient's case, referring him for pericardiectomy prematurely may have led to a morbid surgery in someone whose disease process may be reversed with anti-inflammatories. Furthermore, although symptomatic management is an important part of this patient's treatment regimen, oral Lasix alone would not affect the clinical trajectory regarding the disease process. Lastly, NSAIDs would not maximize potential benefit without a corticosteroid. There is emerging use for biologics such as anakinra and rilonacept in this setting as well.4 Ultimately, our patient did not improve after another course of prednisone which led to pericardiectomy approximately 6 months later. Post-operative course was uncomplicated, and he is currently doing well.
References
- Jellis CL, Tariq MU. Transient Constrictive Pericarditis – Releasing the Grip. http://www.acc.org. Sep 14, 2015. Accessed 07/20/2021. https://www.acc.org/latest-in-cardiology/articles/2015/09/09/12/19/transient-constrictive-pericarditis.
- Feng D, Glockner J, Kim K, et al. Cardiac magnetic resonance imaging pericardial late gadolinium enhancement and elevated inflammatory markers can predict the reversibility of constrictive pericarditis after anti-inflammatory medical therapy: a pilot study. Circulation 2011;124:1830-37
- Ramchand J, Chahine J, Alnajjar H, et al. Long-term nature history of transient constrictive pericarditis. Eur Heart J 2020;2: ehaa946.2163.
- Andreis A, Imazio M, Giustetto C, Brucato A, Adler Y, De Ferrari GM. Anakinra for constrictive pericarditis associated with incessant or recurrent pericarditis. Heart 2020;106:1561-65.