Assessing the Symptomatic Patient With Hypertrophic Cardiomyopathy and Valve Disease
A 73-year-old woman with known hypertrophic cardiomyopathy (HCM) presents with progressive dyspnea on mild exertion over the prior few months.
She was originally diagnosed with HCM 9 years earlier and underwent alcohol septal ablation (ASA) due to medically refractory symptoms. A postoperative echocardiogram demonstrated left ventricular outflow tract (LVOT) gradient 9 mm Hg at rest, which did not change after a Valsalva maneuver. Over an interval of 3-4 years, she reported a marked improvement in her symptoms. She then, however, started to again report progressive worsening exercise intolerance manifest as dyspnea on exertion. At the time of this presentation, she is unable to walk more than a few feet without becoming markedly short of breath. She was previously able to walk around a large box store without symptoms but now needs to use a motorized cart. She has also started developing worsening lower extremity swelling and orthopnea.
Past medical history: Paroxysmal atrial fibrillation (AF), morbid obesity (body mass index 39 kg/m2), hypertension, hyperlipidemia, history of colon cancer treated with colonic resection.
Family history: Father with sudden cardiac death in his early fifties (unclear etiology), one sister with HCM who has undergone ASA, one brother died in infancy, second brother died due to respiratory issues related to chronic obstructive pulmonary disease. Two daughters: one screened for HCM with no evidence and the other chooses not to be screened.
Social history: Retired and widowed.
Cardiac medications: Furosemide 40 mg BID, metoprolol tartrate 150 mg BID, simvastatin 20 mg, apixaban 5 mg BID.
Height: 162.6 cm
Weight: 104 kg
Heart rate: 62 bpm
Blood pressure: 124/68 mm Hg
Physical examination: Pleasant woman in no acute distress, alert, comfortable, thought content appropriate. Regular rate and rhythm with soft early peaking systolic murmur at the left sternal border, which does not accentuate with Valsalva. Jugular venous pressure difficult to appreciate due to body habitus, 2+ pitting edema to knee, equal and 2+ radial and femoral pulses.
She was unable to tolerate higher doses of metoprolol due to presyncope. As a result of her progressive symptoms, she undergoes repeat transthoracic echocardiography (Figure 1).
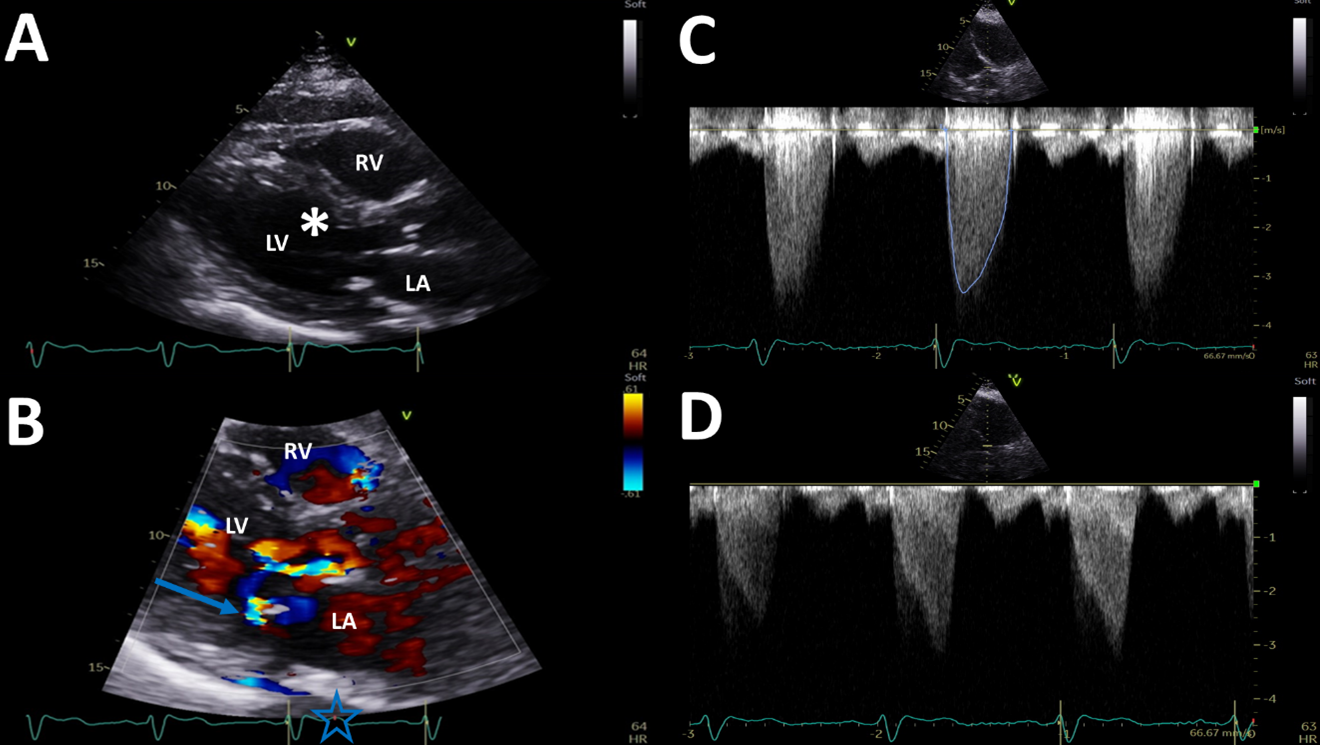
Figure 1
There is a crescent-shaped left ventricle (LV) with asymmetric LV hypertrophy (septum 17 mm) and hyperdynamic LV function (Figure 1, panel A). The anteroseptum exhibits a shaved-off appearance consistent with prior septal ablation (denoted by "*"). There is systolic anterior motion (SAM) of the mitral valve (MV) and at least moderate mitral regurgitation (MR) (Figure 1, panel B; arrow). The aortic valve (AoV) is moderately calcified with restricted opening; there is an early peaking gradient through the AoV with mean gradient 27 mm Hg (Figure 1, panel C). There is also a late-peaking gradient consistent with LVOT obstruction (peak gradient 34 mm Hg) at rest (Figure 1, panel D) that increases to 55 mm Hg after Valsalva maneuver and 46 mm Hg after a premature ventricular contraction (PVC).
With these echocardiographic findings of dynamic LVOT obstruction, SAM with at least moderate MR, and a restricted AoV with moderate aortic stenosis (AS), she is presented and discussed at your institution's HCM Center of Excellence multidisciplinary meeting. This monthly conference includes general cardiologists, imaging specialists, interventional cardiology, and cardiac surgery. As there is recurrent LVOT obstruction on maximally tolerated medical therapy, septal reduction therapy is discussed. There are two key questions addressed:
- With a history of a prior ASA, what are the important factors to consider when recommending repeat septal reduction therapy?
- Are there other coexisting pathologies that need to be addressed?
With evidence of LVOT obstruction, AS, and MR on her transthoracic echocardiogram as well as numerous risk factors for atherosclerotic cardiovascular disease, she undergoes left heart catheterization and transesophageal echocardiography to better evaluate these potential contributions to her presenting symptoms (Figure 2).
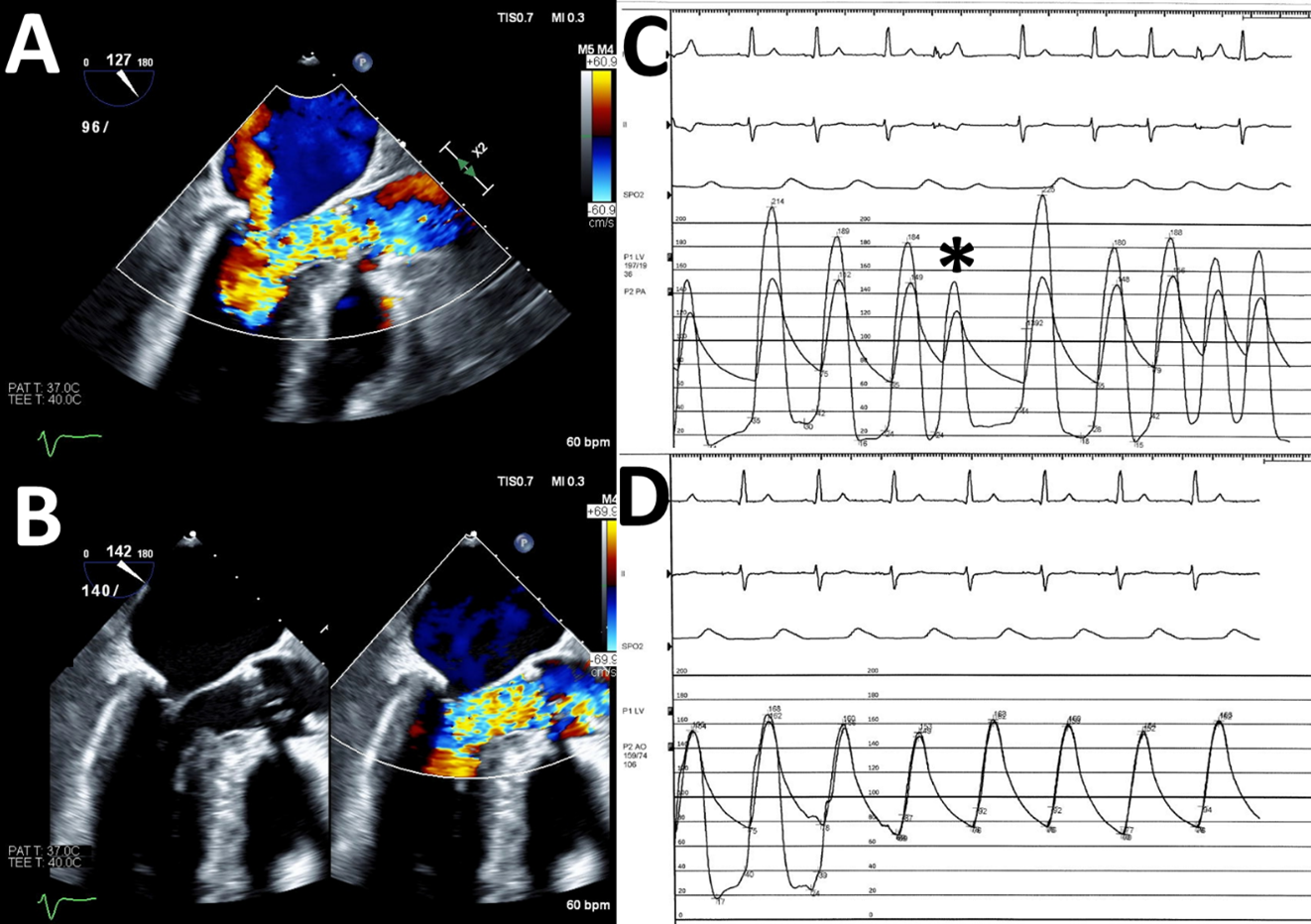
Figure 2
Transesophageal echocardiography with color Doppler is performed at systolic blood pressure 96 mm Hg (Figure 2, panel A) and 140 mm Hg (Figure 2, panel B). Invasive coronary angiography demonstrates diffuse mid left anterior descending artery (LAD) disease with a severe 70% lesion at the bifurcation of the second diagonal branch (images not shown). Hemodynamic tracings demonstrate mid-LV–to–LVOT gradient 30-35 mm Hg at rest that increases to 70 mm Hg following PVC and 135 mm Hg following PVC during nitroglycerin infusion (Figure 2, panel C; PVC denoted by "*"). The gradient across the AoV is 5-10 mm Hg (Figure 2, panel D).
Which one of the following is your recommendation regarding this patient's management plan?
Show Answer