A 31-year-old male with cystic fibrosis (CF) presented with 5 days of worsening respiratory status as well as increasing abdominal girth, bilateral lower extremity swelling, and 20-pound weight gain. Physical examination revealed fever, scattered pulmonary rales, and a new pericardial friction rub. He was admitted for CF exacerbation secondary to bacterial pneumonia with respiratory sputum cultures eventually growing methicillin-resistant staphylococcus aureus and multidrug resistant pseudomonas. However, despite usual therapies for CF exacerbation, he developed squeezing chest pain and worsening dyspnea. Re-examination revealed jugular venous distention, pulsus paradoxus of 16 mmHg, and more pronounced pericardial friction rub.
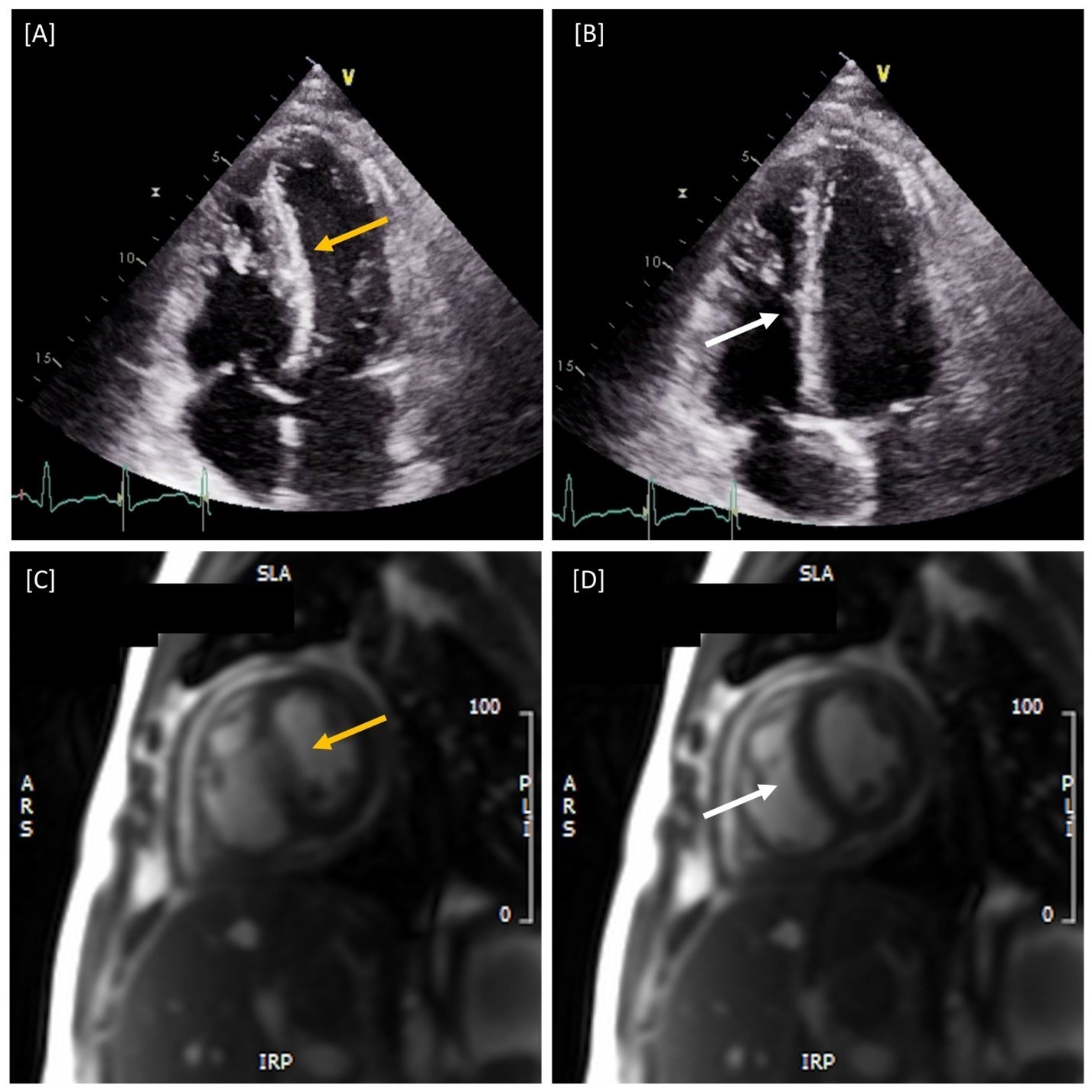
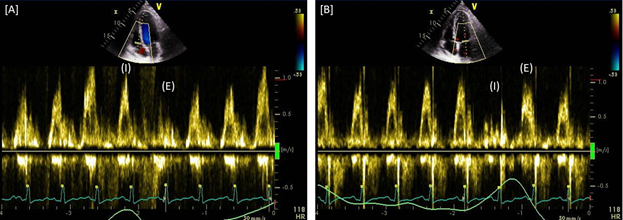
Electrocardiogram revealed sinus tachycardia without ST changes. Chest computed tomography showed ground glass and tree-in-bud opacities in the bilateral peri-cardiac regions of the lungs. Urgent transthoracic echocardiogram revealed multiple features concerning for pericardial constriction including thickened pericardium, respiratory variation of the mitral and tricuspid Doppler inflow velocities, ventricular septal shift, and increased diastolic flow reversal on hepatic vein Doppler during expiration (Figure 1A-B). A trivial, circumferential pericardial effusion without evidence of tamponade was also present. Constrictive findings were further confirmed with cardiac magnetic resonance imaging (CMR) revealing thickened pericardium at 7 mm and ventricular interdependence without fibrosis (Figure 1C-D).
Several days of oral colchicine led to resolution of the friction rub and loop diuretics facilitated return to euvolemia. At 3-month follow-up, the patient's echocardiogram and CMR showed continued constriction without effusion.
Figure 1
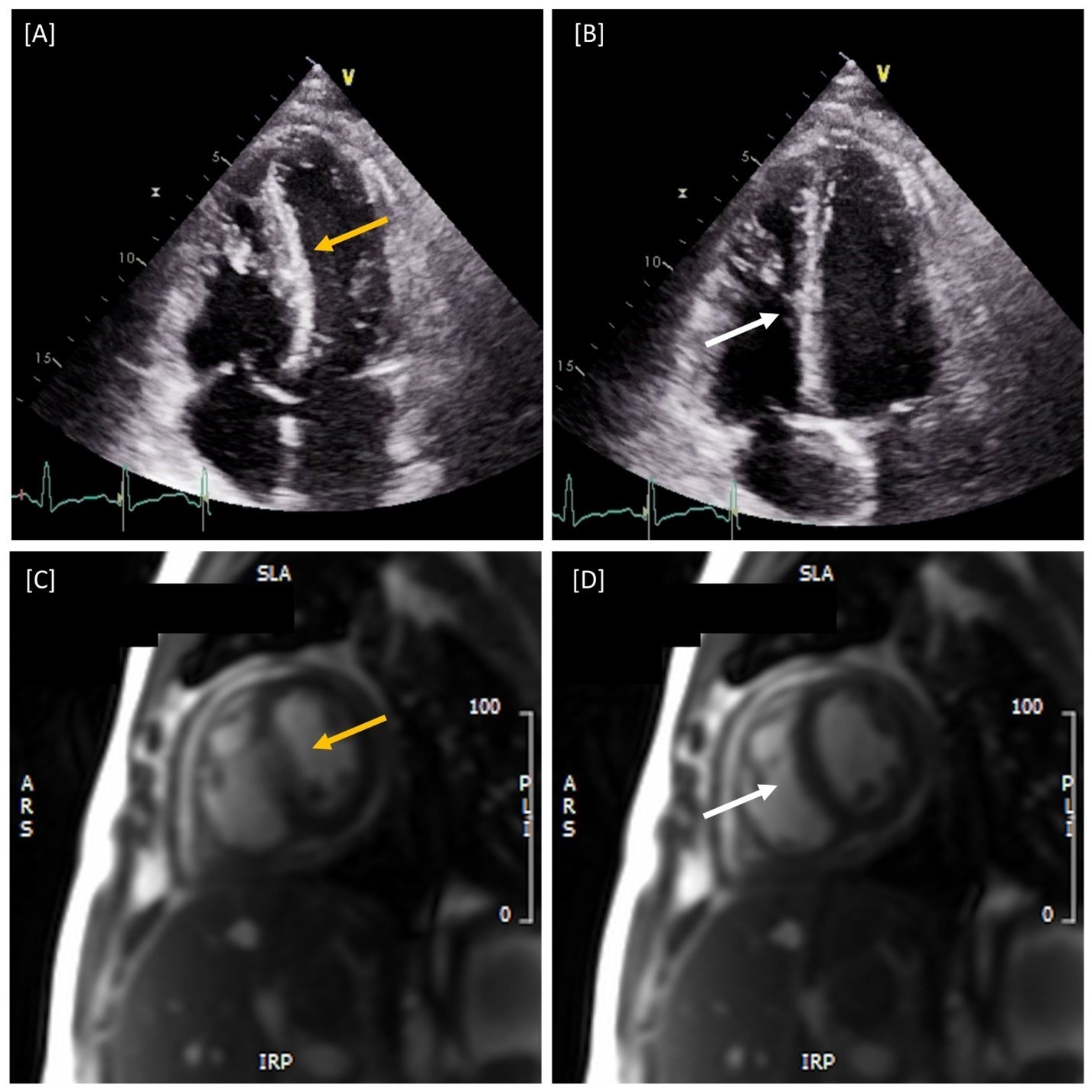 Figure 1: Paradoxical Septal Motion with Respiratory Variation. [A-B] Apical Four Chamber Transthoracic Echocardiography and [C-D] Short Axis CMR revealing accentuated septal movement towards the left ventricle (yellow arrows) during inspiration [A, C] with significant septal rebound back into the right ventricle (white arrows) during expiration [B,D] indicative of ventricular interdependence and consistent with constrictive pericarditis.
Figure 1: Paradoxical Septal Motion with Respiratory Variation. [A-B] Apical Four Chamber Transthoracic Echocardiography and [C-D] Short Axis CMR revealing accentuated septal movement towards the left ventricle (yellow arrows) during inspiration [A, C] with significant septal rebound back into the right ventricle (white arrows) during expiration [B,D] indicative of ventricular interdependence and consistent with constrictive pericarditis.
The correct answer is: D. All the above
Though considerable overlap in signs and symptoms of constrictive pericarditis and cystic fibrosis exists, this is only the third reported case of concomitant disease.1 Recurrent pulmonary inflammation in this patient from bacterial pneumonia led to a subacute, effusive-constrictive pericarditis requiring targeted therapy other than typical cystic fibrosis management for resolution.
While the patient's pericardial friction rub raised initial concern for an additional process, echocardiography confirmed the presence of pericardial constriction with a variety of variables. The "sniff test," more commonly used for detecting the presence of diaphragmatic paralysis, consisting of a quick, sharp inspiratory effort through the nose can be performed during transthoracic echocardiography to exemplify the dissociation of intrathoracic and intracardiac pressures in constriction.2 With fixed intracardiac volume, sniffing increases right ventricular filling causing the interventricular septum to shift towards the left ventricle. As seen in Figure 2, tricuspid valve inflow velocity increases as blood fills the right ventricle while mitral valve inflow velocity decreases due to impaired left ventricular filling and output from interventricular septal shift. The opposite is expected during expiration consistent with ventricular interdependence. In fact, ventricular septal shift was found to have an odds ratio of 7.7 for constrictive pericarditis and diagnose it with 87% sensitivity and 91% specificity when combined with either medial mitral annulus e' velocity ≥9 cm/s or hepatic vein expiratory diastolic reversal ratio ≥0.79.3
Figure 2
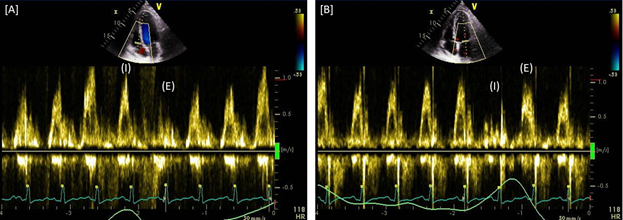 Figure 2: Respiratory Variation of Transvalvular Flow. [A] Tricuspid Doppler inflow velocity increases through peak inspiratory (I) efforts with a significant, sudden decrease upon expiration (E) while [B] Mitral Doppler inflow velocity is suddenly reduced upon inspiratory efforts as seen by the lime green respiratory tracing along the bottom of each graphic.
Figure 2: Respiratory Variation of Transvalvular Flow. [A] Tricuspid Doppler inflow velocity increases through peak inspiratory (I) efforts with a significant, sudden decrease upon expiration (E) while [B] Mitral Doppler inflow velocity is suddenly reduced upon inspiratory efforts as seen by the lime green respiratory tracing along the bottom of each graphic.
Figure 2: Respiratory Variation of Transvalvular Flow. [A] Tricuspid Doppler inflow velocity increases through peak inspiratory (I) efforts with a significant, sudden decrease upon expiration (E) while [B] Mitral Doppler inflow velocity is suddenly reduced upon inspiratory efforts as seen by the lime green respiratory tracing along the bottom of each graphic.
References
- McCartney C, Nayak R. Idiopathic constrictive pericardial disease in a patient with cystic fibrosis. Am J Med Case Rep 2016;4:118-21.
- McCool FD, Tzelepis GE. Dysfunction of the diaphragm. N Engl J Med 2012;366:932-42.
- Welch TD, Ling LH, Espinosa RE, et al. Echocardiographic diagnosis of constrictive pericarditis: Mayo Clinic criteria. Circ Cardiovasc Imaging 2014;7:526-34.