Chief Complaint: Syncope
HPI: A 53-year-old man presents with an episode of syncope which occurred once while he was riding his bicycle. The patient was not injured in the incident. He has not experienced chest discomfort on exertion. Since that time the patient has avoided riding and has remained asymptomatic. Prior to this episode the patient denied any dyspnea. There have been no symptoms of orthopnea, lower extremity edema, nor palpitations.
Family History: There are no family members with a diagnosis of hypertrophic cardiomyopathy nor any family members with premature sudden cardiac death.
Social/Occupational History: He is a lifelong smoker and non-alcohol user. He takes frequent 5-mile bicycle rides in his neighborhood without any issues.
Pertinent Physical Exam:
BMI: 31 kg/m2
Blood pressure: 122/80 mm Hg
Pulse: 72/min
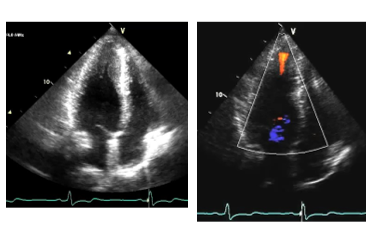
Cardiac exam: Discrete and nondisplaced point of maximal impulse, regular rate and rhythm, grade 2/6 late-peaking systolic ejection murmur heard best along the left sternal border without change during Valsalva.
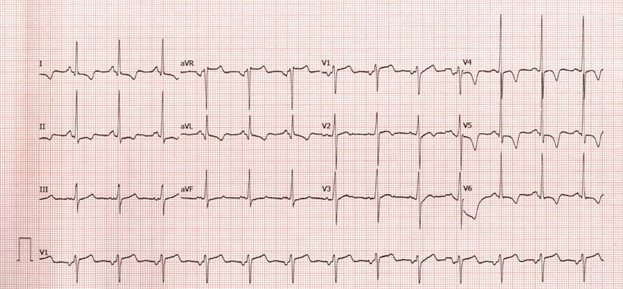
ECG: example provided normal sinus rhythm with T-wave inversions in the precordial leads.
Ambulatory ECG monitoring: 14 days of monitoring demonstrated sinus rhythm with no sustained arrhythmias.
Transthoracic echocardiography:
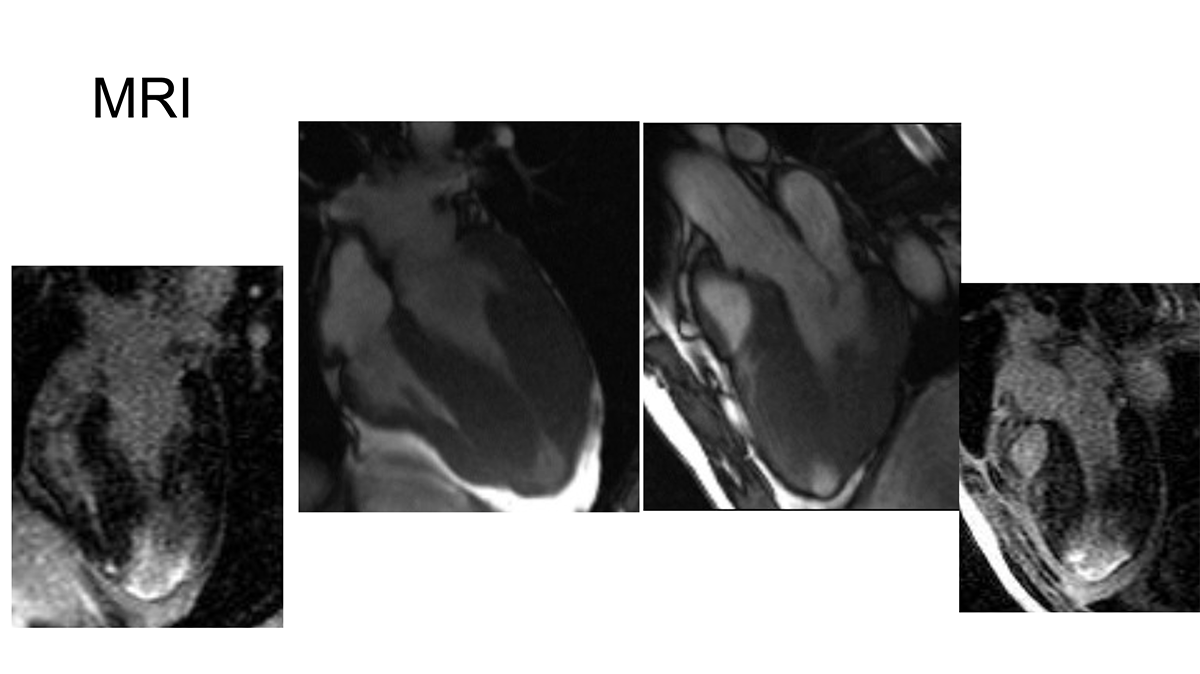
Cardiac MR:
The correct answer is: C. Engage in a shared decision-making discussion regarding the role of a primary prevention ICD
Answer A is incorrect as the patient does not have evidence of LVOT obstruction nor arrhythmia warranting treatment with a beta blocker. A beta blocker would be useful in patients with LVOT obstruction to reduce contractility and heart rate to improve forward flow.
Answer B is incorrect as exercise stress echocardiography is indicated to evaluate for worsening of dynamic LVOT obstruction during exercise in symptomatic patients. This patient did not have symptoms and does not have dynamic LVOT obstruction.
Answer C is correct since an apical aneurysm (independent of size) is associated with an increased risk for sudden cardiac death, ventricular arrhythmia, and heart failure. For adult patients with 1 or more major risk factors for sudden cardiac death, it is a 2a recommendation to offer an ICD for primary prevention. This should be thoroughly discussed with the patient factoring patient preferences along with the risks and benefits in a balanced approach.
Answer D is incorrect since an evaluation should be conducted of the individual patient's risk factors for sudden cardiac death. A comprehensive shared decision-making approach is recommended.
Educational grant support provided by: Bristol Myers Squib
To visit the course page for the Hypertrophic Cardiomyopathy: Accelerating Guideline-Driven Care grant, click here.
References
- Ommen SR et al. 2020 ACCF/AHA Guideline for the diagnosis and treatment of hypertrophic cardiomyopathy. Circulation. 2020
- Rowin E.J., Maron B.J., Haas T.S., et al. "Hypertrophic cardiomyopathy with left ventricular apical aneurysm: implications for risk stratification and management". J Am Coll Cardiol 2017;69:761-773.