Our patient is a 61-year-old female with past medical history notable for atrial flutter and paroxysmal atrial fibrillation s/p cavotricuspid and pulmonary vein isolation with radiofrequency ablation (5 years prior to presentation), recurrent atrial fibrillation s/p redo pulmonary vein isolation with radiofrequency ablation at outside facility complicated by left atrial perforation with hemopericardium and tamponade. She underwent pericardial drain placement for this (3 months prior to presentation) which was complicated by pericarditis (2 months prior to presentation) s/p medical treatment, now presenting for admission with worsening chest pain, shortness of breath and fever for 1–2-week duration.
Prior to discharge from her recent ablation, she was started on indomethacin 50mg three times a day (TID) x7 days and discharged on apixaban 2.5mg twice a day (BID) (dose reduced given hemopericardium) with resolution of pericardial effusion s/p pericardiocentesis. Two months prior to presentation, she presented to an outside emergency department with pleuritic chest pain and was found to have a trace effusion with pericardial thickening on computed tomography (CT), and started on colchicine 0.6mg BID, ibuprofen 600mg TID, pantoprazole and sucralafate with concern for pericarditis. She completed a 2-week course of ibuprofen and continued her colchicine for a total of 7 weeks (with intermittent use of NSAIDs for chest pain) with improvement, but not resolution of chest discomfort prior to discontinuing both medications for gastrointestinal (GI) side effects (abdominal pain). She continued to have minimal, but tolerable chest discomfort for 1 additional week, prior to developing clinical fever, fatigue and worsening pleuritic chest pain. She presented to an outside clinic for further evaluation and was found to have a moderate sized pericardial effusion without tamponade physiology and was referred to our facility for further evaluation and management. Upon arrival to our outpatient clinic, she had been off colchicine and NSAIDs for about 2 weeks, was found to have a large pericardial effusion on echocardiogram. She reported continued chest pain with positional and pleuritic features, fever, and progressive fatigue. She was then admitted to our hospital for expedited evaluation and management of her symptoms and imaging findings.
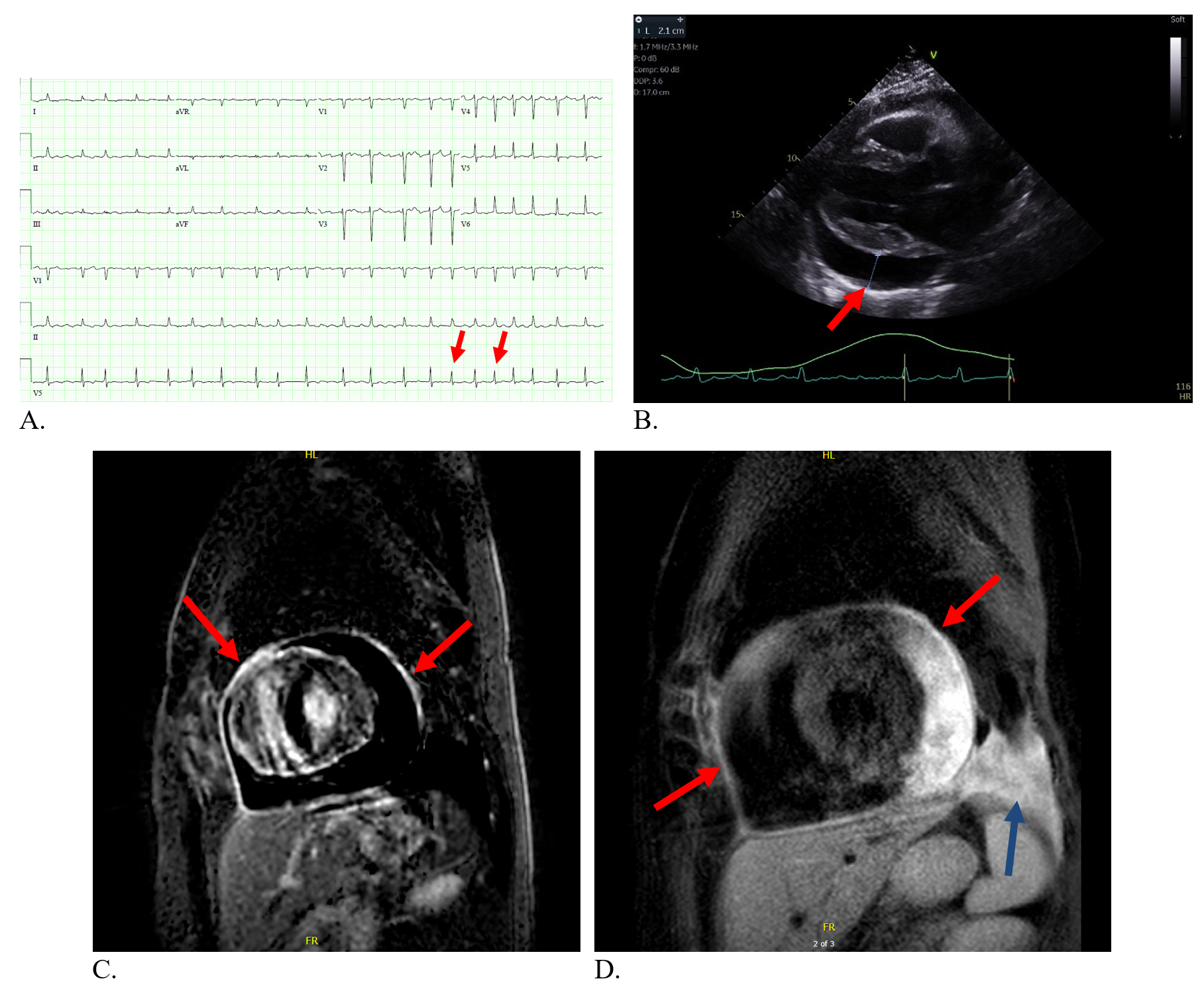
Upon admission, vitals were notable for T 36.5C, heart rate (HR) 125bpm, blood pressure (BP) 119/61 mmHg, RR 16/min, SaO2 95% on room air and without pulsus parodoxus (< 10mmHg fall in SBP on inspiration). Physical exam was notable for a comfortable appearing female sitting upright in bed, with an irregularly irregular tachycardic rhythm without abnormal heart sounds, murmur, or rub. She was clear to auscultation bilaterally with warm, well perfused extremities. Labs on admission notable for elevated erythrocyte sedimentation rate (ESR) 46mm/hr (0-15mm/hr), and elevated ultra-sensitive CRP 17.8mg/L (< 3.1mg/L). An electrocardiogram (ECG) was obtained and notable for atrial fibrillation with rapid ventricular rate (RVR), low voltage and electrical alternans (Figure 1: A, red arrows). Her transthoracic echocardiogram demonstrated a large circumferential pericardial effusion measuring 2.1cm along the inferolateral left ventricle (Figure 1: B). A cardiac magnetic resonance imaging (MRI) was obtained and notable for a moderate to large circumferential pericardial effusion, mostly located lateral to the left ventricle, with no apparent pericardial thickening. There was no diastolic septal bounce, but subtle respirophasic septal shift. There was no diastolic restraint or conical deformity of the ventricles. This constellation of findings was not consistent with the presence of constrictive physiology. There was circumferential late gadolinium enhancement (LGE) of the pericardium seen on fat suppressed imaging, indicative of inflammation (Figure 1: C). Cardiac MRI also demonstrated circumferential pericardial enhancement on T2 short-tau inversion recovery (STIR) sequencing, which indicates pericardial edema consistent with acute inflammation (Figure 1: D).
Figure 1
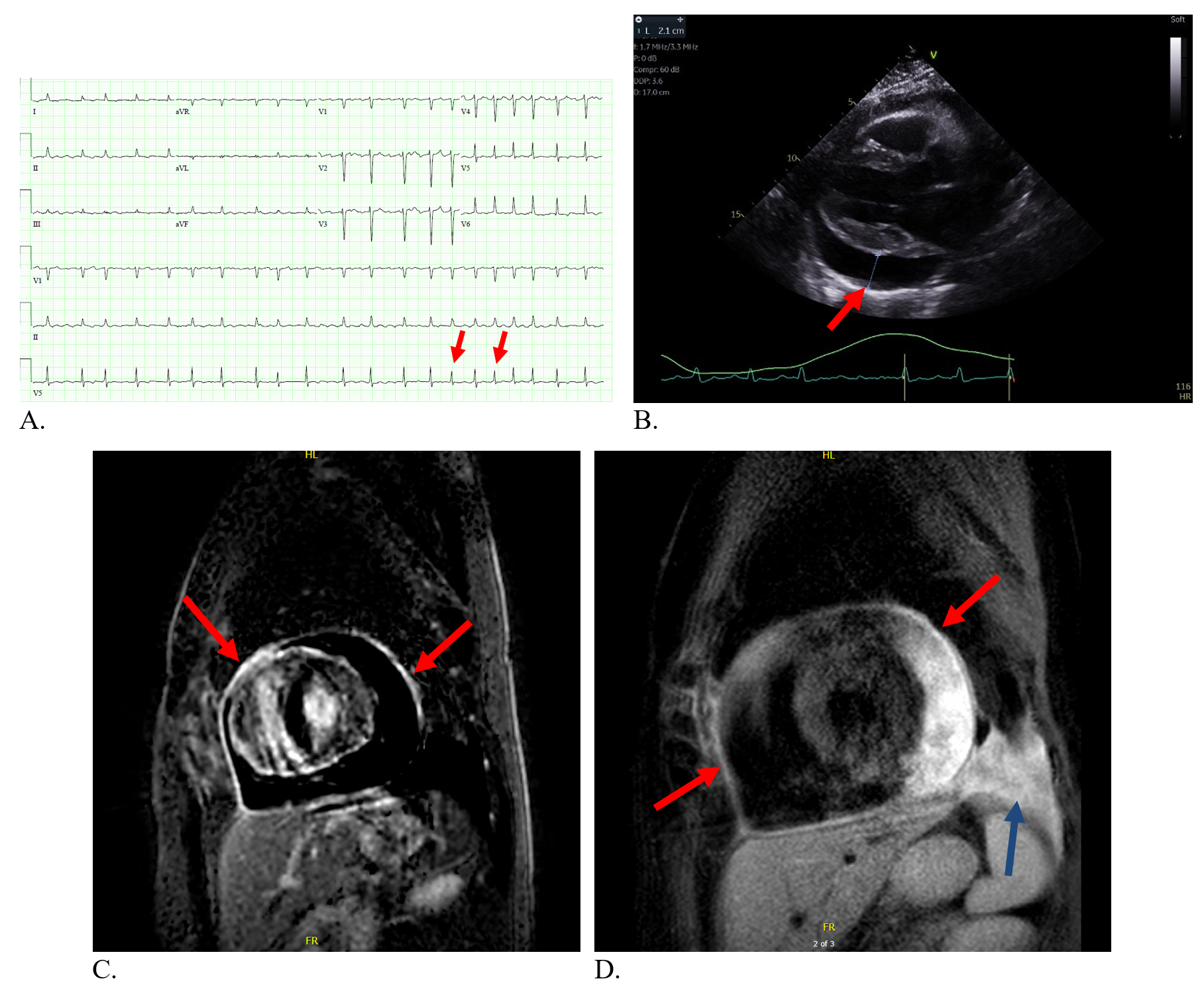 Figure 1: A: Electrocardiogram with findings consistent with pericardial effusion and atrial fibrillation with rapid ventricular rate B: Transthoracic echocardiogram with large pericardial effusion (red arrow) on parasternal long axis view. C: Cardiac MRI short axis with fat suppression and circumferential LGE (arrows). D: Cardiac MRI with T2 weighted STIR sequencing with circumferential enhancement, mostly lateral to pericardial effusion (red arrows). Also note pleural effusion (blue arrow).
Figure 1: A: Electrocardiogram with findings consistent with pericardial effusion and atrial fibrillation with rapid ventricular rate B: Transthoracic echocardiogram with large pericardial effusion (red arrow) on parasternal long axis view. C: Cardiac MRI short axis with fat suppression and circumferential LGE (arrows). D: Cardiac MRI with T2 weighted STIR sequencing with circumferential enhancement, mostly lateral to pericardial effusion (red arrows). Also note pleural effusion (blue arrow).
Key Findings:
- Continued symptoms of positional and pleuritic chest pain
- Elevated inflammatory markers present
- Echo with a large effusion without tamponade physiology
- Cardiac MRI with active pericardial inflammation (circumferential pericardial LGE; pericardial edema) without constrictive physiology
A management decision was made, her symptoms improved, and repeat echocardiogram 5 days later was notable for complete resolution of her pericardial effusion.
The correct answer is: B. Initiate steroids and restart twice daily colchicine
Taking her clinical history into account with her presentation, her diagnosis is most consistent with acute pericarditis given she met at least two out of four clinical criteria for the diagnosis (pericardial chest pain, new or worsening pericardial effusion, pericardial rub, ECG changes). Her acute pericarditis is secondary to a post-cardiac injury syndrome (PCIS) given injury to the pericardium with left atrial perforation during radiofrequency ablation and pericardiocentesis for resultant tamponade. More specifically, she was diagnosed with incessant post-traumatic pericarditis given her continuous pericarditis symptoms for more than 4-6 weeks and less than 3 months following pericardial injury during a cardiac procedure.1,2
Regarding management, echocardiography was utilized initially for hemodynamic evaluation of her effusion in assessment for tamponade physiology despite her clinical stability arguing against clinical tamponade. Cardiac MRI was utilized for detection of pericardial inflammation with LGE, evaluation for constrictive physiology, and T2 STIR weighting was utilized to stage the inflammation with evaluation for pericardial edema, which is indicative of more active or acute pericardial inflammation.1,3 Given findings of pericardial enhancement on T2 STIR imaging, her pericardial inflammation was characterized as an acute pericarditis, and she would benefit from escalation of her medical therapy.1,4
Regarding treatment, our patient was started on prednisone 40mg daily in addition to colchicine 0.6mg BID as second line therapy given her previous incomplete response to colchicine and NSAIDs.2,4 If steroid treatment is selected, it is recommended to use low to moderate dose steroids (e.g., prednisone 0.2-0.5mg/kg/day) with a planned taper of 5-10mg/day every 1-2wks.4 High dose steroids have been found to increase the chronicity and recurrence rate of pericarditis.5 Pericardiectomy is an incorrect response as the patient has active pericardial inflammation on cardiac MRI which has not demonstrated refractoriness to second or third line therapies, and there was no constrictive physiology on cardiac MRI to suggest constrictive pericarditis.2,4 Restarting twice daily colchicine and NSAIDs is also an incorrect response as she had an incomplete response previously (although incomplete treatment of 7 weeks) and she did not tolerate the combination given her abdominal pain despite proton pump inhibitor (PPI) and sucralafate. Although her pericardial effusion was large, she did not demonstrate tamponade physiology or clinical tamponade for that matter to warrant emergent pericardiocentesis, and a trial of medical therapies was preferred to alleviate chest discomfort and treat the underlying inflammation. With the chosen medical strategy, her symptoms improved, pericardial effusion resolved, and she was discharged with plans for a 3-month course of colchicine and tapering of her prednisone while following inflammatory markers (CRP, ESR) to help guide the steroid tapering process.2,4 If our patient is unable to taper off of her prednisone due to recurrent symptoms or increasing inflammation (elevated ESR, CRP) a biologic therapy could be initiated. Biologics such as anakinra and rilonacept, which both act to reduce inflammation through interleukin-1 antagonism, have been found to resolve recurrent pericarditis, steroid dependent pericarditis and reduce recurrences.6,7 If a patient is intolerant of steroids, or is unable to successfully wean off steroids, it may be reasonable to consider medical therapy with an interleukin-1 inhibitor given the results seen in these trials.6,7
References
- Verma BR, Chetrit M, Gentry JL 3rd, et al. Multimodality imaging in patients with post-cardiac injury syndrome. Heart 2020;106:639-46.
- Chiabrando JG, Bonaventura A, Vecchié A, et al. Management of acute and recurrent pericarditis: JACC State-of-the-Art Review. J Am Coll Cardiol 2020;75:76-92.
- Chetrit M, Xu B, Kwon DH, et al. Imaging-guided therapies for pericardial diseases. JACC Cardiovasc Imaging 2020;13:1422-37.
- Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases: the task force for the diagnosis and management of pericardial diseases of the European Society of Cardiology (ESC)Endorsed by: the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2015;36:2921-64.
- Imazio M, Brucato A, Cumetti D, et al. Corticosteroids for recurrent pericarditis: high versus low doses: a nonrandomized observation. Circulation 2008;118:667-71.
- Imazio M, Andreis A, De Ferrari GM, et al. Anakinra for corticosteroid-dependent and colchicine-resistant pericarditis: The IRAP (International Registry of Anakinra for Pericarditis) study. Eur J Prev Cardiol 2020;27:956-964.
- Klein AL, Imazio M, Cremer P, et al. Phase 3 trial of interleukin-1 trap rilonacept in recurrent pericarditis. N Engl J Med 2021;384:31-41.