Pericardial and Pleural Effusions After STEMI
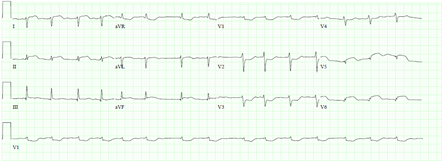
A 70-year-old hypertensive diabetic man presented to his local emergency department with 5 days of chest pressure and dyspnea. His past cardiac history was notable for atrial fibrillation for which he was treated with a percutaneous left atrial occluder, and sick sinus syndrome for which he had a permanent pacemaker. He denied infectious symptoms, palpitations, and syncope, but admitted to orthopnea and worsening leg edema. He was hemodynamically stable on presentation and required oxygen supplementation at 2L to maintain a peripheral saturation of 94%. Physical examination revealed evidence of heart failure. His electrocardiogram (ECG) revealed changes consistent with lateral ST-elevation myocardial infarction (STEMI) with Q-waves (Figure 1).
Figure 1
He was transferred emergently to our quaternary referral center for management. However, due to late presentation, he did not undergo emergent cardiac catheterization.
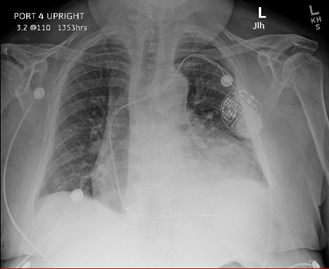
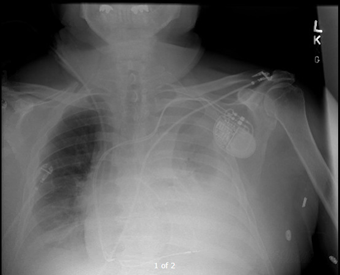
Chest radiography revealed cardiomegaly and increased vascular markings consistent with decompensated heart failure (Figure 2).
Figure 2
Echocardiography revealed severely diminished left ventricular systolic function with a focal wall motion abnormality in the left circumflex artery territory along with a moderate pericardial effusion (Video 1).
Video 1
The patient was managed conservatively with medical therapy for heart failure and STEMI including dual antiplatelet therapy with aspirin and clopidogrel, diuresis, afterload reduction, nitrates, and a heparin drip. His symptoms of congestion improved and he was transferred out of the intensive care unit to a telemetry stepdown unit. A pharmacologic positron emission tomography stress test using both rubidium-82 for perfusion and 18F-fluorodeoxyglucose (FDG) for viability testing revealed absent uptake of both radiotracers in the left circumflex territory consistent with scar. Cardiac catheterization revealed occluded mid-left anterior descending and mid-circumflex arteries. Percutaneous angioplasty was deferred.
He remained hospitalized and initially did well with diuresis; however, he developed worsening chest discomfort 1 week after presentation (approximately 2 weeks after the onset of symptoms). He was hemodynamically stable and afebrile. Repeat ECG did not show significant changes compared to ECG on admission. Repeat echocardiography revealed an enlarging pericardial effusion (Video 2); echocardiographic contrast, when injected intravenously, was not detected in the pericardial space, suggesting absence of myocardial free wall rupture. There were no echocardiographic features of tamponade.
Video 2
Simultaneously, a left sided pleural effusion was detected on chest radiography (Figure 3).
Figure 3
Pericardiocentesis and thoracentesis were done, yielding sterile but exudative serosanguineous effusion in both the pericardial (350cc) and pleural (900cc) spaces. Extensive laboratory examination of both pericardial and pleural fluid was negative for malignancy and infection. The pericardial drain was left in place but the pleural drain was removed after drainage. The patient's symptoms improved following drainage of effusions, and within 48 hours the pericardial drain was removed. Unfortunately, the patient suffered an episode of refractory ventricular tachycardia and expired despite resuscitative efforts approximately 3 weeks after presentation.
What diagnosis explains this patient's effusions?
Show Answer