The patient is a 74-year-old male with a history of persistent atrial fibrillation (AF); s/p pulmonary vein isolation (PVI) and cavotricuspid isthmus (CTI) dependent atrial flutter (AFL) ablation 2 years ago; aortic stenosis; s/p mechanical aortic valve replacement (AVR); coronary artery disease; s/p coronary artery bypass graft (CABG); obstructive sleep apnea (OSA) on continuous positive airway pressure (CPAP); hypertension; and body mass index (BMI) at 27.4 kg/m2; who is seen at the antiarrhythmic clinic for his routine 3-month follow-up.
He has been feeling fair with frequent episodes of exertional shortness of breath, fatigue, malaise, and exercise intolerance, which has affected his regular moderate intensity exercise activity. He does not drink alcohol and eats a Mediterranean diet.
His rhythm control strategy of AF started 9 years ago, when he underwent an electrical cardioversion followed with an initiation of sotalol, which sustained sinus rhythm for 7 years. However, persistent AF breakthrough required another cardioversion and initiation of amiodarone, that caused the patient significant tremor necessitating lowering the dose. AF recurrence led to initiation of dofetilide and AF and AFL ablation 2 years ago. Post-ablation, he felt great, and his 30 days mobile cardiac telemetry showed sinus rhythm with 2% atrial tachyarrhythmia.
He is on warfarin, dofetilide, potassium chloride, magnesium oxide, metoprolol, and losartan.
His lab data showed serum potassium at 4.3, serum magnesium at 1.9, serum creatinine at 0.97, and glomerular filtration rate (GFR) at 76.
Recent 30 days mobile cardiac telemetry showed 63% atrial tachyarrhythmia.
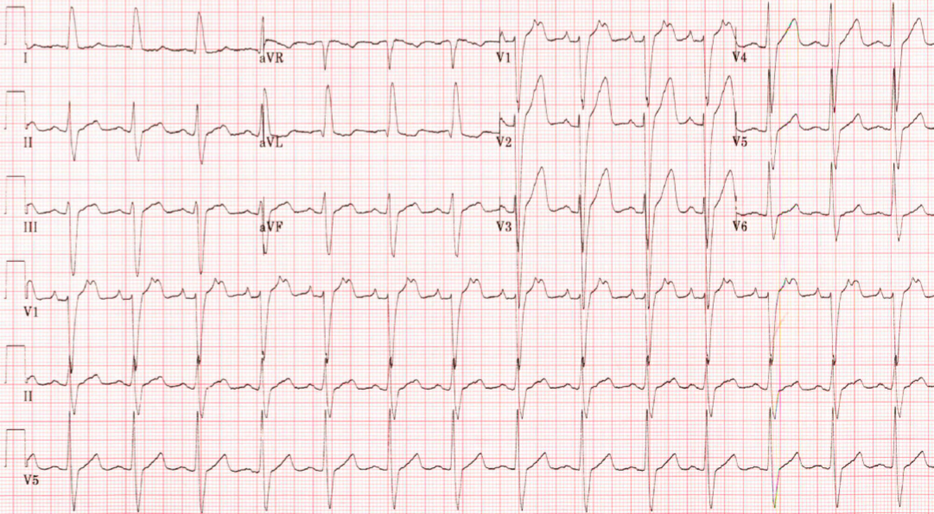
An electrocardiogram (ECG) (Figure 1) is performed and shows the following:
The correct answer is: C. Proceed with electrophysiology study and mapping ablation of left atrium.
ECG showed atrial tachycardia (AT) at a rate of 176 bpm and wide QRS complex rhythm with a heart rate of 89 bpm. There is left axis deviation and left bundle branch block with a QRS duration of 134 milliseconds (ms). QT/corrected QT (QTc) intervals are 404 and 491 ms, respectively.
Patient has intermittent atrial tachyarrhythmia on the mobile cardiac telemetry. Therefore,
cardioversion is not the appropriate next step due to likely relapse back to AT. Answer A is incorrect.
The atrial tachyarrhythmia could be focal, micro-reentrant or macro-reentrant AT. Therefore, CTI dependent AFL should be considered. However, the features of the P waves are not typical for CTI dependent AFL. The P waves in lead II, III and aVF are upright with an isoelectric line between the P waves.1 Therefore, answer B is incorrect.
Optimal risk factor modifications and lifestyle management are essential to optimize rhythm control strategy for AF. This regiment has not been shown to be helpful in AT.2 Therefore, answer D is incorrect.
The prevalence of AT post-AF ablation varies from <5% to 40% depending on the ablation strategy and duration of AF.3 The incidence of AT is higher in our patient since he had persistent AF, which results in an electrical and structural remodeling and atrial myopathy.1
PVI using radiofrequency ablation and atrial remodeling creates the substrate for AT including small gaps in the previous ablation line or around pulmonary veins requiring detailed high-density mapping and ablation of focal, micro-reentrant or macro-reentrant AT.4,5
References
- Hung Y, Chang SL, Lin WS, Lin WY, Chen SA. Atrial tachycardias after atrial fibrillation: how to manage? Arrhythm Electrophysiol Rev 2020;9:54–60.
- Chung MK, Eckhardt LL, Chen LY, et al. Lifestyle and risk factor modification for reduction of atrial fibrillation: a scientific statement from the American Heart Association. Circulation 2020;141:e750–e772.
- Chugh A, Oral H, Lemola K, et al. Prevalence, mechanisms, and clinical significance of macroreentrant atrial tachycardia during and following left atrial ablation for atrial fibrillation. Heart Rhythm 2005;2:464–71.
- Yamashita S, Takigawa M, Denis A, et al. Pulmonary vein-gap re-entrant atrial tachycardia following atrial fibrillation ablation: an electrophysiological insight with high-resolution mapping. Europace 2019;21:1039–47.
- Luther V, Sikkel M, Bennett N, et al. Visualizing localized reentry with ultra-high-density mapping in iatrogenic atrial tachycardia: beware pseudo-reentry. Circ Arrhythm Electrophysiol 2017;10:e004724.