Effusive Constrictive Pericarditis
A 52-year-old woman with a medical history of HIV diagnosed in 1995 and subarachnoid hemorrhage from an anterior communicating artery aneurysm that required clipping in 2010 presents to the emergency department with left wrist swelling for 4 days that is accompanied by intermittent fever. She is admitted to the hospital for further evaluation and is started on broad-spectrum antibiotic therapy.
Physical examination is notable for mild acute distress, elevated jugular venous pressure (JVP; up to 13 cm H2O), distant heart sounds, mild symmetric lower extremity edema, and a left wrist that demonstrates erythema, warmth, and tenderness. Initial laboratory workup shows leukocytosis (white blood cell count 13.7 k/mcL), normochromic normocytic anemia, elevated inflammatory markers with erythrocyte sedimentation rate 99 mm/hour and C-reactive protein level 23.9 mg/dL, CD4 count 370 cells/mcL, and HIV viral load 332 copies/mL. A diagnostic arthrocentesis is performed, and results are positive for Streptococcus pneumoniae bacteria.
Based on sensitivity analysis, antibiotics are de-escalated to ceftriaxone. During hospitalization, she reports sudden onset tearing chest pain that radiates to the back. A computed tomography (CT) angiogram of the chest/abdomen/pelvis reveals evidence of an eccentric focal aneurysm on the undersurface of the distal aortic arch. Additionally, a large pericardial effusion is visualized, measuring up to 17 mm with subtle enhancement of the parietal pericardium (Figure 1).
Figure 1
Subsequently, a transthoracic echocardiogram (TTE) shows early diastolic collapse of the right ventricular (RV) free wall with plethoric inferior vena cava (Figure 2).
Figure 2
As her blood pressure starts to decline with evidence of pulsus alternans, an urgent pericardiocentesis is performed with aspiration of 450 mL of nonpurulent serous fluid. Analysis of aspirated fluid includes: protein level 4.2 g/dL (serum protein level 8.3 g/dL); pH 7.6; glucose level 121 mg/dL; adenosine deaminase (ADA), gram stain, and culture negative; no acid fast bacilli by fluorochrome stain; and no anaerobic or fungal growth. Additional blood tests include thyroid-stimulating hormone level 2.71 mcU/mL, negative antinuclear antibody screening panel, and negative blood tuberculosis test. Given a concern for a systemic infectious process that could explain these findings (i.e., the aortic aneurysm and pericardial effusion), a whole-body fluorine-18 fluorodeoxyglucose positron emission tomography/CT imaging is performed, which shows a rim of hypermetabolism surrounding the aortic aneurysm suggestive of a mycotic nature of the structure (Figure 3).
Figure 3
Clinical manifestations of volume overload (elevated JVP, peripheral edema) persist despite volume optimization and decongestion. A repeat echocardiogram shows no recurrent tamponade features or re-accumulation of pericardial effusion; however, there is a significant respiratory variation of the mitral inflow velocity on pulsed-wave Doppler analysis (Figure 4).
Figure 4
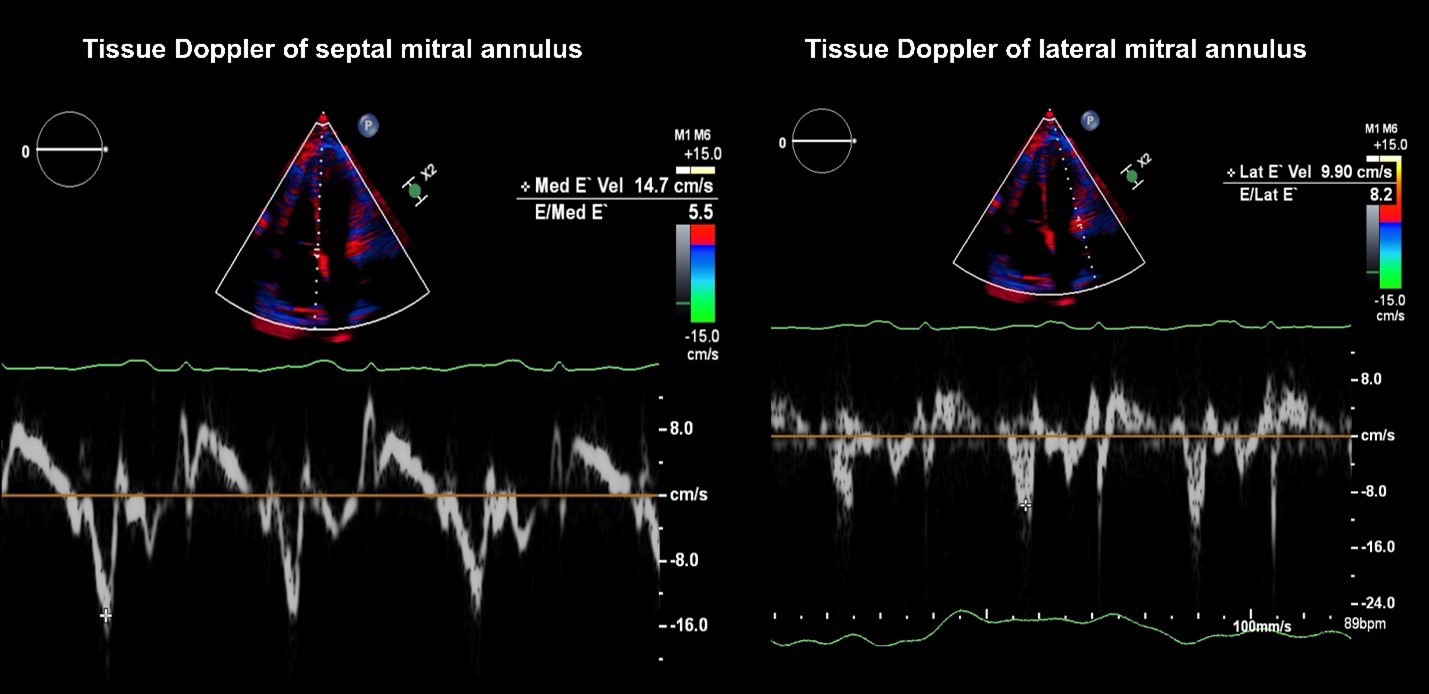
Additionally, tissue Doppler velocities of the septal and lateral mitral annulus are 14.7 cm/sec and 9.9 cm/sec, respectively (Figure 5).
Figure 5
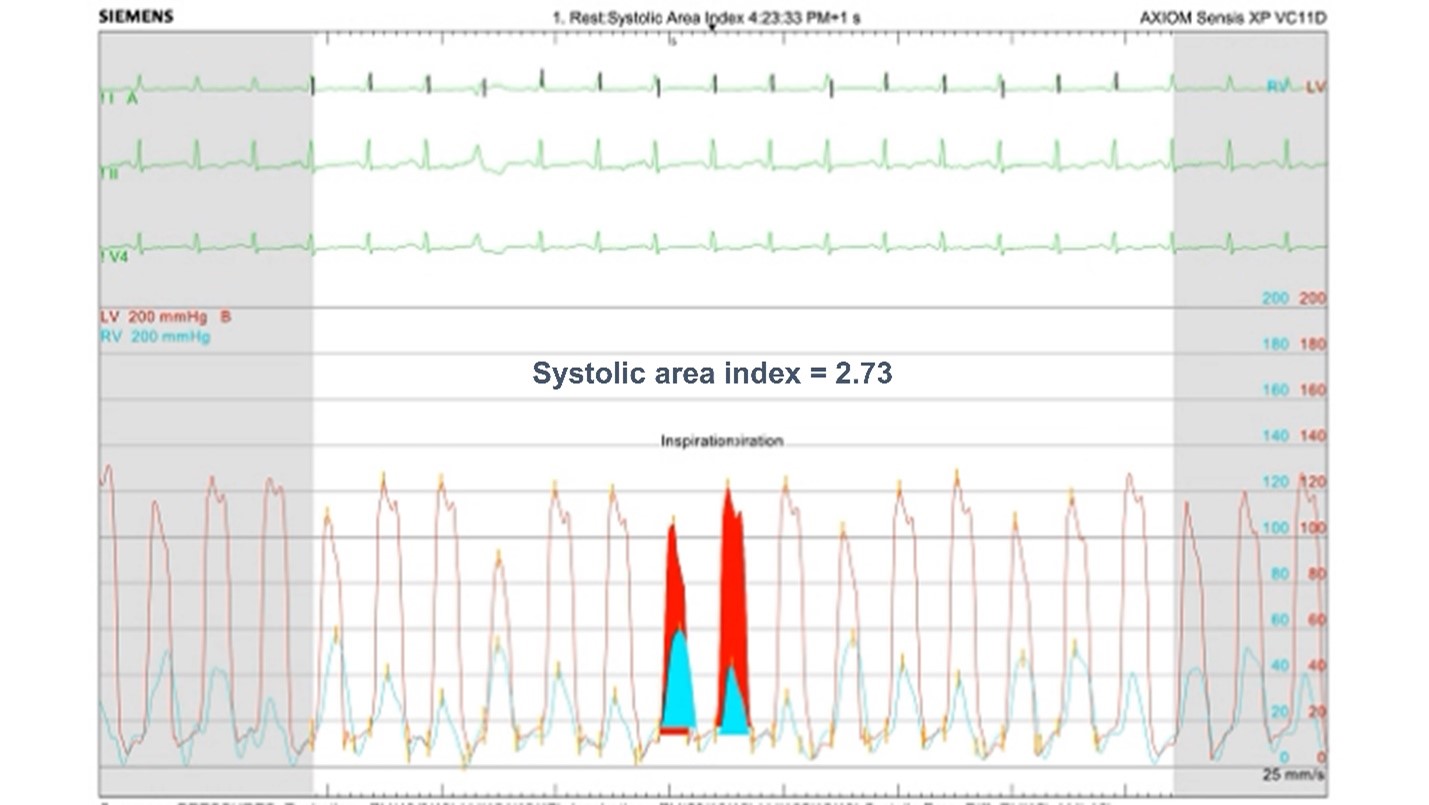
Preoperative evaluation with a simultaneous right and left heart catheterization is performed. Coronary angiography shows no evidence of coronary artery disease. Invasive hemodynamic assessment confirms the diagnosis suggested by TTE.
Which one of the following is the most specific hemodynamic parameter that confirms the echocardiographic diagnosis?
Show Answer