The infant had generalized arterial calcification of infancy (GACI), which can usually be confirmed with genetic testing. Video 1 is a four-chamber view from a fetal echocardiogram showing right atrial dilation, mildly depressed right ventricular systolic function, and a small circumferential pericardial effusion. Video 2 is a sweep from the fetal echocardiogram through the main and branch pulmonary arteries showing thickened, echobright vessel walls. Videos 3 and 4 are transthoracic echocardiogram clips showing echobright walls of the ascending aorta and right pulmonary artery (Figure 1). The echobright appearance of the aorta and pulmonary arteries is strongly suggestive of arterial calcification and typical of GACI. Among the answer choices, genetic testing is most likely to confirm the diagnosis. Thus, answer choice A is the correct choice.
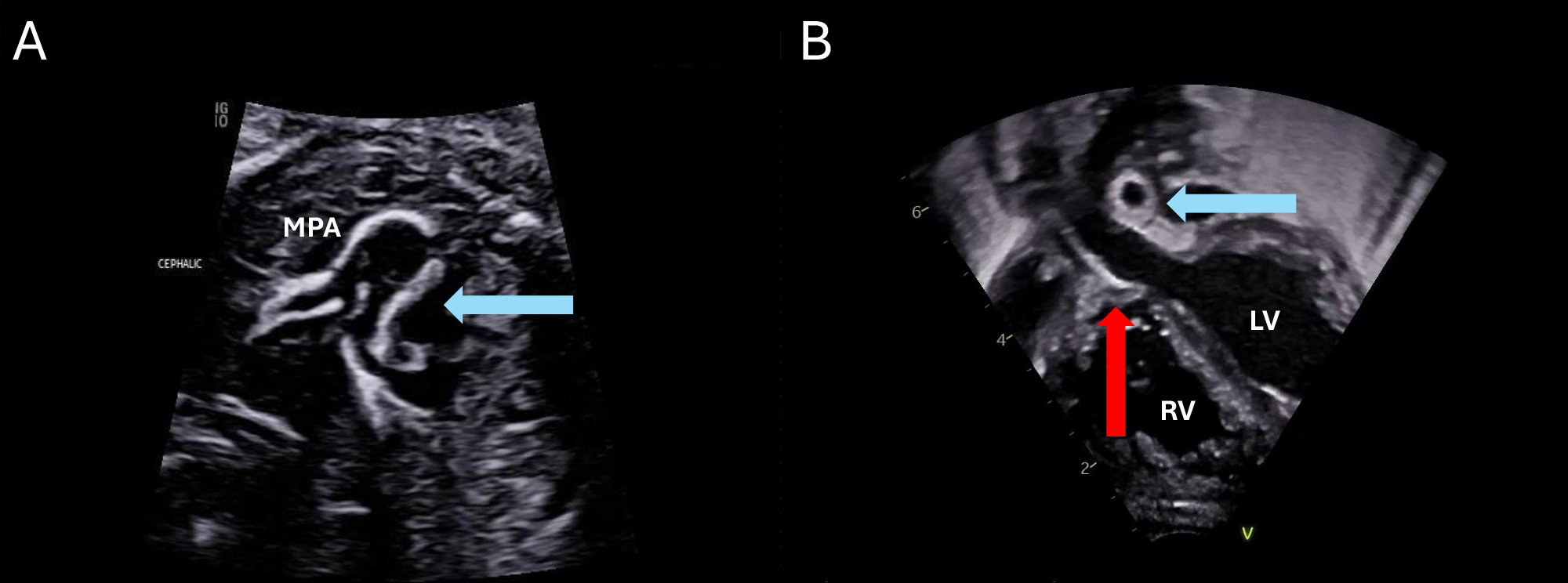
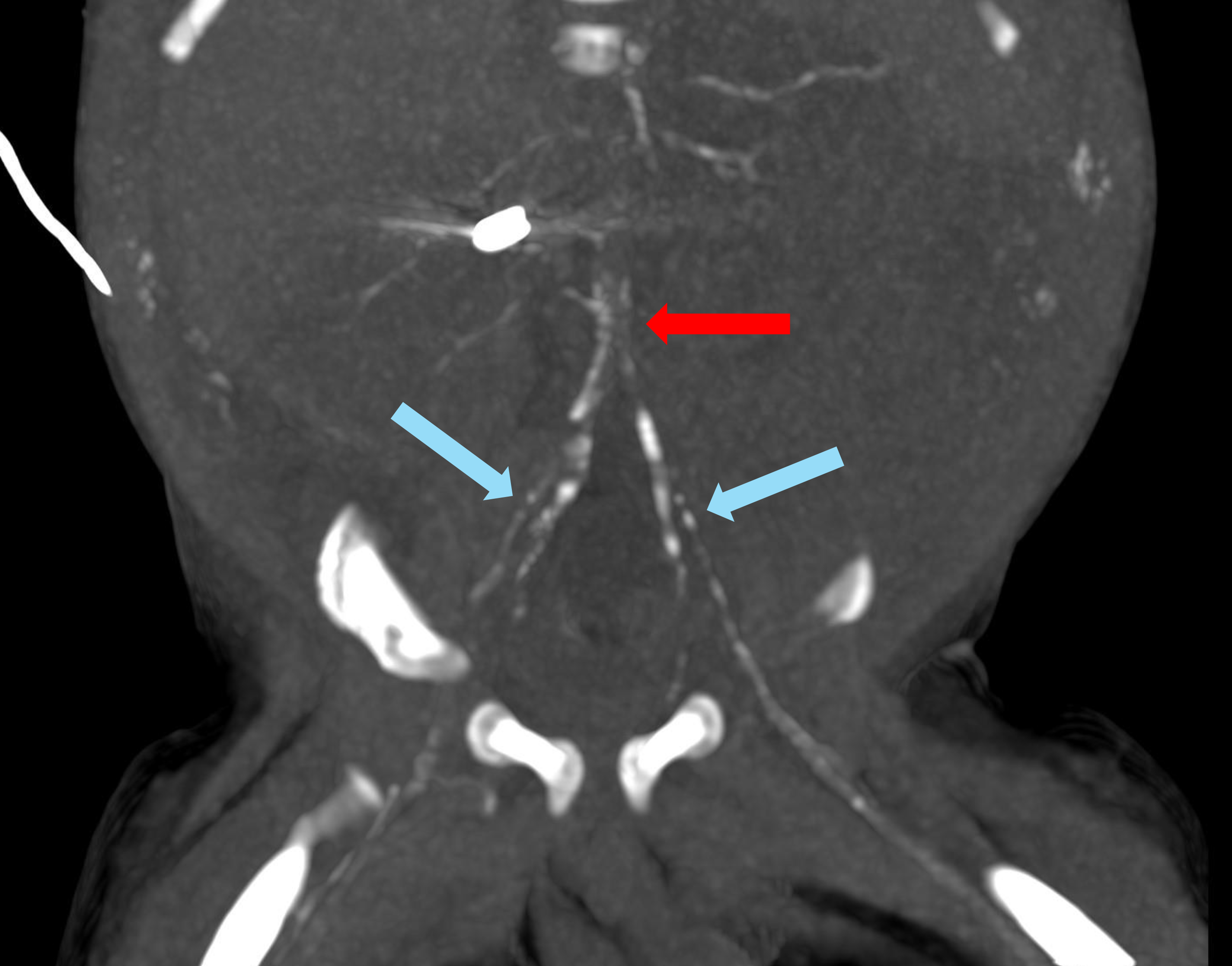
Figure 1: Transthoracic Echocardiogram Clips Showing Echobright Walls of the AAo and RPA
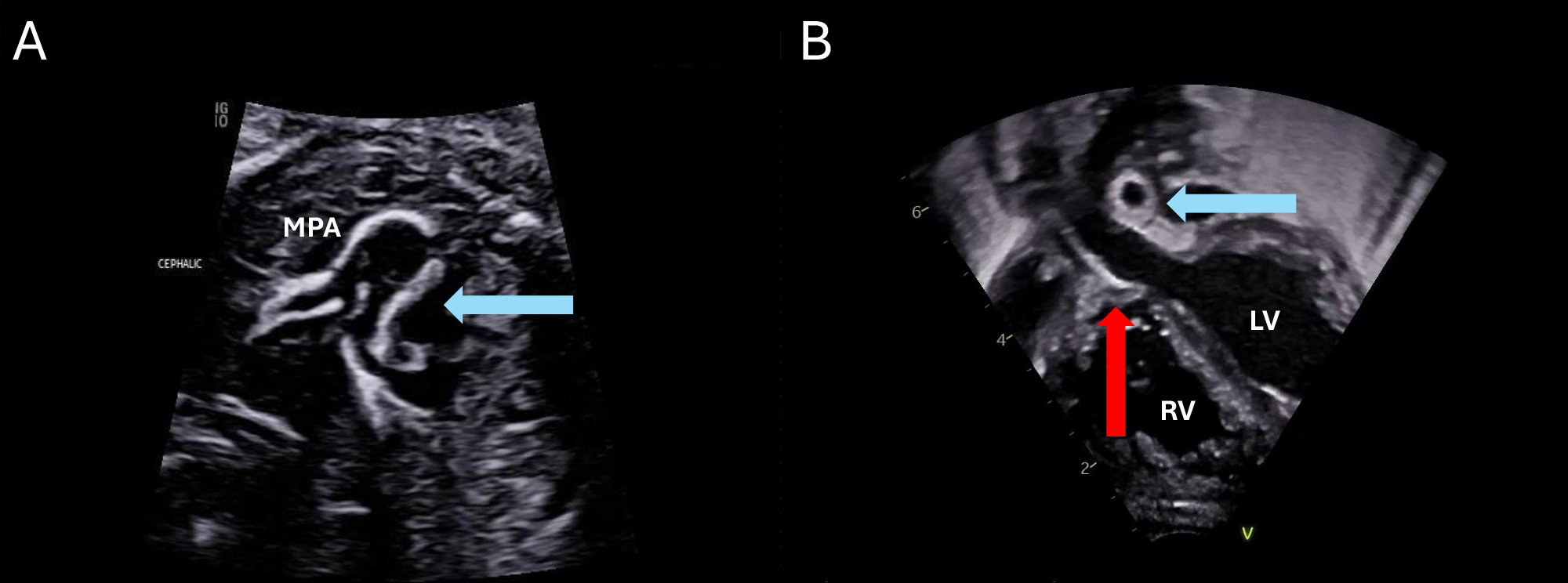
(Panel A) Fetal echocardiogram short-axis view of the MPA (blue arrow) and branch PAs showing echobright vessel walls consistent with arterial calcification. (Panel B) Transthoracic echocardiogram subcostal transverse view showing the AAo (red arrow) and proximal RPA (blue arrow) with echobright walls.
AAo = ascending aorta; LV = left ventricle; MPA = main pulmonary artery; PAs = pulmonary arteries; RPA = right pulmonary artery; RV = right ventricle.
Rapid plasma reagin testing (answer choice B) can be used to evaluate for congenital syphilis. Although calcifications in the brain and liver can occur in the setting of congenital syphilis, this patient's presentation of arterial calcification is more consistent with GACI. Free carnitine level (answer choice C) can evaluate for primary carnitine deficiency but has no role in diagnosis of GACI. Cerebral vascular insufficiency has been described in GACI1; brain MRI (answer choice D) may evaluate for associated neurologic injury but is not the best test to confirm the underlying diagnosis. Thus, answer choices B-D are incorrect choices.
GACI is a rare autosomal recessive disorder of calcium metabolism that is typically caused by a mutation in the ENPP1 gene (GACI Type 1) or ABCC6 gene (GACI Type 2).1,2 Pathogenic mutations in these genes are identified in most phenotypic cases. Consequently, diagnosis can generally be confirmed by multigene panels or comprehensive genomic testing including exome sequencing.3 Disruption in cellular mineral resorption activities results in deposition of calcium and intimal proliferation in the internal elastic lamina of large and medium-sized arteries and other soft tissue.
GACI can present in utero with polyhydramnios, nonimmune hydrops, and echobright atrioventricular valves, aorta, and pulmonary arteries due to fibrous intimal thickening and calcification.2,4 Postnatally, it can result in respiratory failure, pulmonary hypertension, myocardial ischemia, hepatic and kidney ischemic injury, and ischemic neurologic injury. Typical features on postnatal echocardiography include echobright walls of the aorta and pulmonary arteries. The presence of calcifications can be confirmed with a noncontrast computed tomography (Figure 2).
Figure 2: Noncontrast Computed Tomogram Confirming Presence of Calcifications
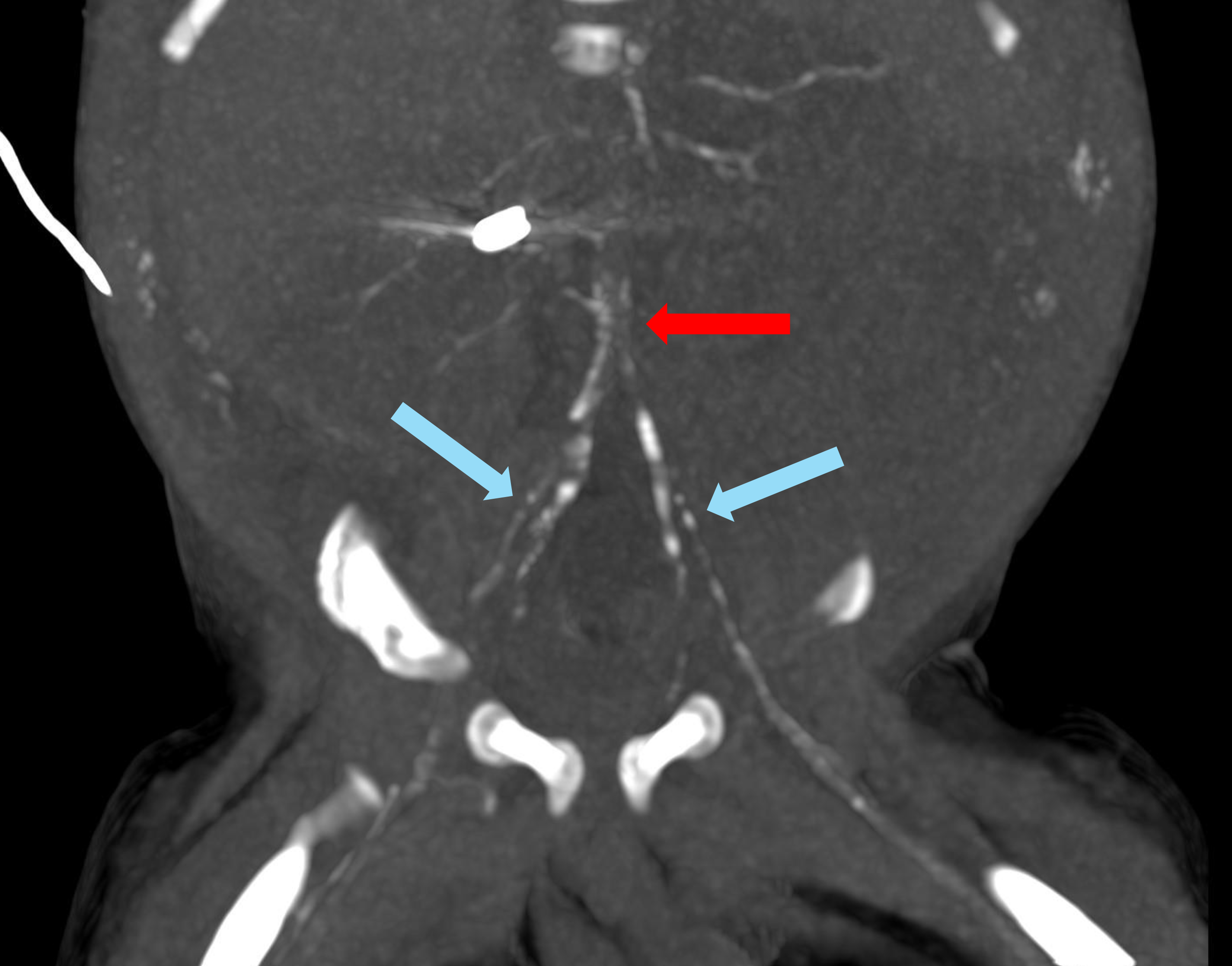
Coronal oblique image from noncontrast computed tomography of the abdomen and pelvis showing calcification of the abdominal descending aorta (red arrow) and common iliac arteries (blue arrows).
GACI has a high mortality rate during infancy (50-85% by 6 months of age), although milder phenotypes and spontaneous resolution have also been reported.1,2 Bisphosphonates such as etidronate can inhibit calcification and have been used for treatment of GACI postnatally. Sodium thiosulfate may exhibit chelating effects on calcium salts and has also been used in GACI. Nevertheless, the role of these medical therapies remains controversial. Prenatal administration of etidronate to pregnant patients with GACI fetuses has also been reported but requires further study.5
Echobright vascular walls on echocardiography should raise suspicion for GACI. The diagnosis of GACI is important given significant prognostic ramifications and to prompt consideration for medical therapy aimed at mitigating the underlying disorder of calcium regulation.
References
- Boyce AM, Gafni RI, Ferreira CR. Generalized arterial calcification of infancy: new insights, controversies, and approach to management. Curr Osteoporos Rep. 2020;18(3):232-241. doi:10.1007/s11914-020-00577-4
- Ramirez-Suarez KI, Cohen SA, Barrera CA, Levine MA, Goldberg DJ, Otero HJ. Longitudinal assessment of vascular calcification in generalized arterial calcification of infancy. Pediatr Radiol. 2022;52(12):2329-2341. doi:10.1007/s00247-022-05364-0
- Ziegler SG, Gahl WA, Ferreira CR. Generalized arterial calcification of infancy. 2014 Nov 13 [Updated 2020 Dec 30]. In: Adam MP, Feldman J, Mirzaa GM, et al., eds. GeneReviews® [Internet]. Seattle: University of Washington, Seattle; 1993-2025. Available at: https://www.ncbi.nlm.nih.gov/sites/books/NBK253403/. Accessed 04/24/2025.
- Pu L, Dai X, Liu H, Li L, Zhao F, Chen J. Prenatal diagnosis of generalized arterial calcification of infancy in the second trimester. Prenat Diagn. 2022;42(12):1538-1544. doi:10.1002/pd.6245
- Agarwal N, Agarwal U, Alfirevic Z, et al. Skeletal abnormalities secondary to antenatal etidronate treatment for suspected generalised arterial calcification of infancy. Bone Rep. 2020;12:100280. Published 2020 May 13. doi:10.1016/j.bonr.2020.100280