In Utero Intruder: A Fetal Cardiac Mass
A routine obstetric ultrasonogram at 32 weeks' gestational age demonstrates a pericardial mass and pericardial effusion in the fetus. A fetal echocardiogram is performed (Video 1).
Video 1: 2D Image in the Axial Plane
2D = two-dimensional.
Based on the echocardiographic findings, which one of the following is the most likely diagnosis?
Show Answer
The correct answer is: B. Teratoma.
This fetus has a large, solitary, heterogeneous pericardial mass and a large pericardial effusion. Labeled frames from Video 1 are shown in Figures 1 and 2. These findings are characteristic of fetal teratomas.
Figure 1: 2D Imaging in an Axial Plane Demonstrating a Large Pericardial Effusion and Normal 4Ch Intracardiac Anatomy
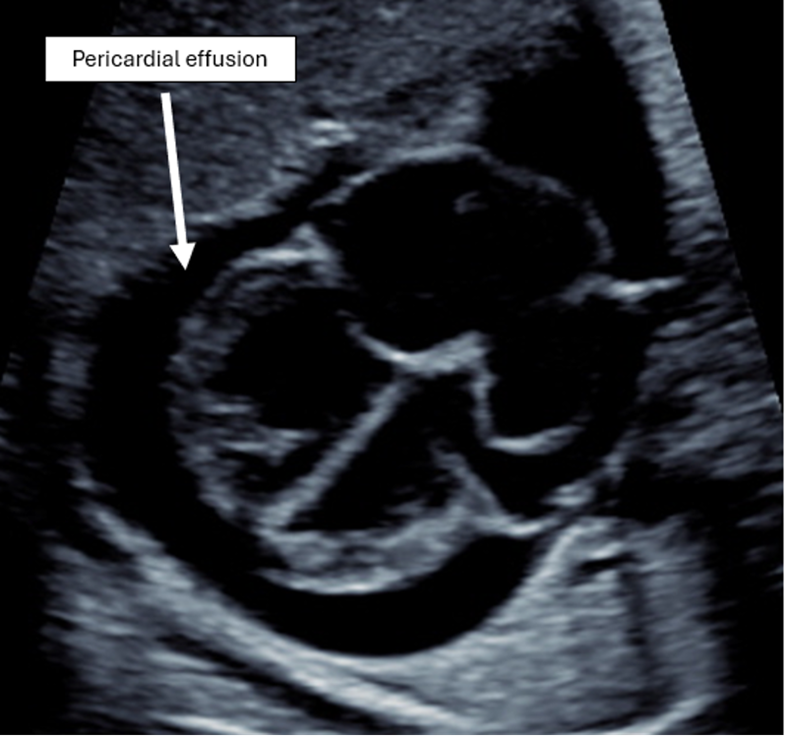
2D = two-dimensional; 4Ch = four-chamber.
Figure 2: 2D Imaging in an Axial Plane Demonstrating a Large, Right-Sided Pericardial Mass With Heterogeneous Echogenicity

The MPA and branch PAs are seen without impingement by the tumor.
2D = two-dimensional; MPA = main pulmonary artery; PAs = pulmonary arteries.
Intrapericardial teratomas compose 6-25% of all congenital cardiac tumors; consist of endodermal, mesodermal, and ectodermal germ cell layers; and are most often benign.1-3 When detected prenatally, they typically have a right-sided location, irregular shape, heterogeneous echotexture, encapsulated appearance, and accompanying pericardial effusion.4-5 Both the tumor and the pericardial effusion can cause compression of cardiac structures, cardiac tamponade, fetal hydrops, and death. Intrapericardial teratomas grow rapidly and studies have shown progressive reduction in combined fetal cardiac output due to evolving tamponade physiology as the tumor expands.5
The outcomes of fetuses with an intrapericardial teratoma are strongly related to the development of nonimmune hydrops.4 Most fetuses that do not develop hydrops and undergo postnatal resection have been shown to have a favorable outcome.4 However, fetuses that are diagnosed with intrapericardial teratomas early in gestation and those that develop hydrops are at increased risk for poor outcomes including intrauterine demise.4
Current management strategies include surveillance and early delivery, maternal steroid therapy,6 and prenatal intervention. The latter includes pericardiocentesis, thoracentesis, amnio-drainage of polyhydramnios, placement of a pericardio-amniotic shunt, laser ablation of the tumor, and resection of the tumor with open fetal surgery. Study results suggest that performing drainage of fluid to temporarily relieve cardiac compression can prolong the pregnancy and thereby improve neonatal outcomes after postnatal surgical resection.4 Case reports have also described successful open fetal surgery to resect the mass prior to the development of hydrops when gestation precludes early delivery.5 Further investigation is needed to understand the indications, best practices, and benefits of these strategies.
In this case, at approximately 32 weeks' gestation, the fetus has a large (5 cm diameter) tumor and a large pericardial effusion. There is no evidence of hydrops. The fetus is monitored closely with serial ultrasonograms and fetal echocardiograms. At 35 weeks' gestation, ascites is diagnosed and there is evidence that both the tumor and pericardial effusion have grown. Given these signs of hemodynamic compromise, the fetus is delivered at 35 weeks' gestation. At 5 days of age, he undergoes a successful resection of the tumor and drainage of the pericardial effusion. At 2 months of age, he remains asymptomatic from a cardiac perspective and has unremarkable findings on echocardiogram.
Rhabdomyoma is an incorrect diagnosis due to the location and echocardiographic appearance of the tumor in this case. Rhabdomyomas typically have a homogeneous appearance on ultrasonogram, are located in the ventricular or atrial cavity, and are often multiple rather than solitary. Rhabdomyomas are the most common type of congenital cardiac tumor, comprise benign proliferations of myocardial tissue, and are frequently associated with tuberous sclerosis complex. They may grow during gestation, typically regress spontaneously after birth, and rarely cause hemodynamic compromise.7-8
Fibromas are tumors that are also often large, solitary, and hyperechoic. However, their location is typically intraventricular (arising from the ventricular septum or free wall) rather than pericardial, which makes this an incorrect diagnosis. Fetal cardiac fibromas are benign connective tissue tumors derived from fibroblasts and are the second-most common fetal cardiac tumor. Fibromas are more likely to be associated with hemodynamic abnormalities than rhabdomyomas and, because of their large size, can cause outflow tract obstruction. Fibromas are also associated with ventricular arrhythmia, a common indication for postnatal surgical resection.9 Fibromas are often diagnosed postnatally or in childhood because spontaneous regression is unusual. Presentation prenatally or in early infancy may indicate more severe disease.1-3
Cardiac myxomas are extremely rare in fetuses. They are solitary, pedunculated masses of endocardial tissue that typically are seen in the atria, making this an incorrect diagnosis.1-3,10
References
- Abuhamad A, Chaoui R. A Practical Guide to Fetal Echocardiography: Normal and Abnormal Hearts. 4th ed. Wolters Kluwer; 2022.
- Lai WW, Mertens LL, Cohen MS, Geva T, eds. Echocardiography in Pediatric and Congenital Heart Disease: From Fetus to Adult. 3rd ed. Wiley Blackwell; 2022.
- Walsh EP, Mayer JE Jr, Teele SA, Brown DW, eds. Nadas' Pediatric Cardiology. 3rd ed. Elsevier; 2024.
- Nassr AA, Shazly SA, Morris SA, et al. Prenatal management of fetal intrapericardial teratoma: a systematic review. Prenat Diagn. 2017;37(9):849-863. doi:10.1002/pd.5113
- Rychik J, Khalek N, Gaynor JW, et al. Fetal intrapericardial teratoma: natural history and management including successful in utero surgery. Am J Obstet Gynecol. 2016;215(6):780.e1-780.e7. doi:10.1016/j.ajog.2016.08.010
- Carosso M, Carosso AR, Bertschy G, et al. New findings in the multidisciplinary management of a fetal intrapericardial teratoma: a case report. Fetal Diagn Ther. 2024;51(1):92-100. doi:10.1159/000533132
- Bosi G, Lintermans JP, Pellegrino PA, Svaluto-Moreolo G, Vliers A. The natural history of cardiac rhabdomyoma with and without tuberous sclerosis. Acta Paediatr. 1996;85(8):928-931. doi:10.1111/j.1651-2227.1996.tb14188.x
- Tworetzky W, McElhinney DB, Margossian R, et al. Association between cardiac tumors and tuberous sclerosis in the fetus and neonate. Am J Cardiol. 2003;92(4):487-489. doi:10.1016/s0002-9149(03)00677-5
- Gikandi A, Chiu P, Secor J, et al. Surgical debulking of large ventricular fibromas in children. J Thorac Cardiovasc Surg. 2025;169(1):186-194. doi:10.1016/j.jtcvs.2024.05.013
- Yuan SM. Fetal primary cardiac tumors during perinatal period. Pediatr Neonatol. 2017;58(3):205-210. doi:10.1016/j.pedneo.2016.07.004
