A 29-year-old black male presents to the emergency department with chest pain. The symptoms were described as an acute onset of moderate substernal tightness radiating to the upper back. There was associated dyspnea, but no nausea, vomiting, or diarrhea. His symptoms were considered atypical in that they were exacerbated by stretching, deep breathing, and movement. The symptoms were different from his prior sickle cell pain crises. As there was no relief with self-administered Percocet at home, he came to the emergency department.
|
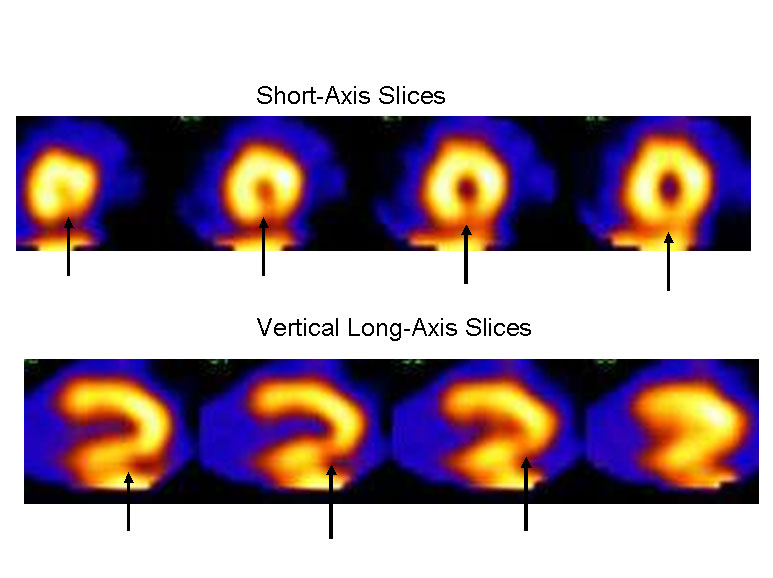
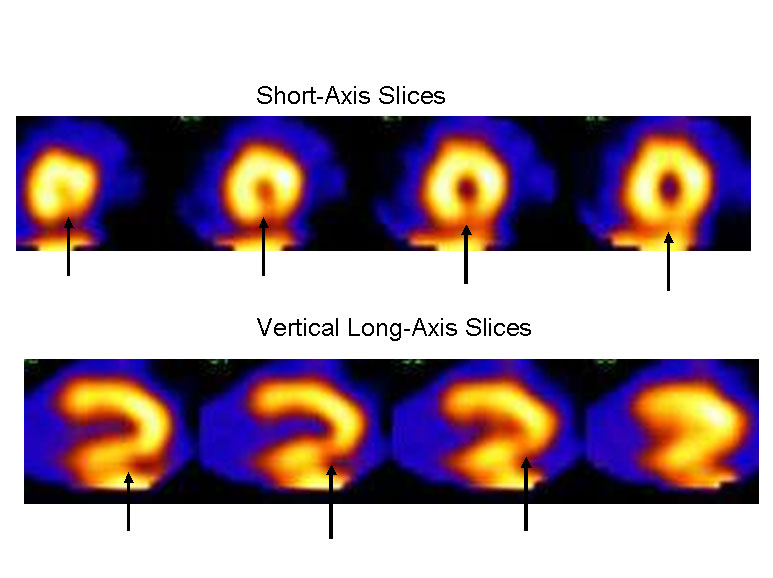
Figure 1
|
|
|
Past medical history: No cardiac history; sickle cell anemia with frequent sickle cell crises, most recently 1 month prior to admission
Social: Smokes one pack per day; no illicit drug use
Family history: Negative for premature coronary disease
Physical exam: Blood pressure 126/60 mm Hg, pulse 87 bpm, respirations 16, afebrile; oxygen saturation 99% on 2 L supplemental oxygen
Head, ears, eyes, nose, throat (HEENT): Mild scleral icterus
Lungs: Clear
Heart: Regular rate and rhythm, 1/6 systolic ejection murmur at left upper sternal border; no rub or gallop
Extremities: No edema
ECG: Normal sinus rhythm, without ischemic changes
Laboratory values: Hemoglobin 8.0, white blood cell count 20.2K, platelets normal, blood urea nitrogen/creatinine 6/0.8
| Cardiac markers: |
| |
2:30 |
5:30 |
11:30 |
21:30 |
| Troponin I, ng/ml |
4.6 |
5.3 |
2.5 |
0.7 |
| Myocardial band (MB), ng/ml |
6.6 |
6.0 |
4.2 |
1.1 |
| Creatine kinase (CK), U/L |
166 |
155 |
161 |
139 |
|
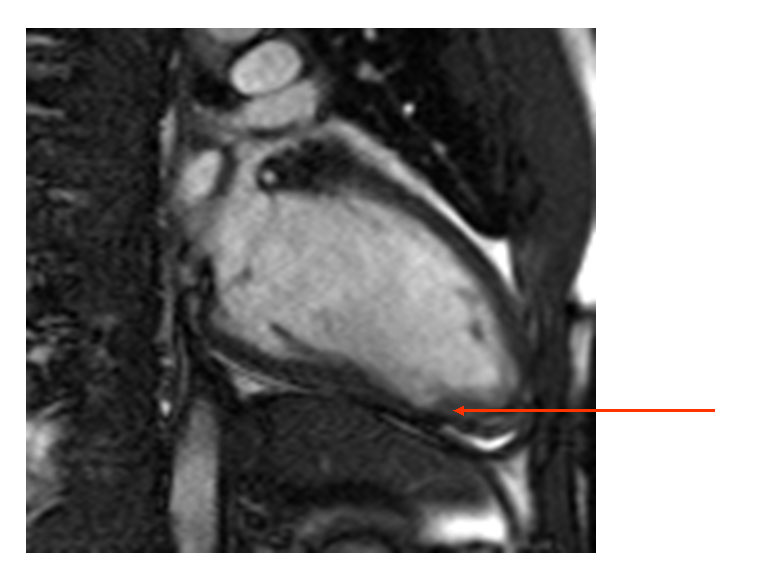
Emergency department course: The patient was initially considered low risk based on age and absence of ECG changes, and underwent acute rest myocardial perfusion imaging (MPI) for further risk stratification. This demonstrated a small sized, low-moderate grade inferior apical defect (Figure 1). Gated images demonstrated abnormal wall motion, and the study was interpreted as consistent with an acute coronary syndrome. The patient was admitted to the coronary intensive care unit. Serial markers were performed:
An echocardiogram demonstrated a mid and distal inferior wall motion abnormality with mild hypokinesia with preserved systolic function. No significant valvular abnormalities were observed, and right ventricular (RV) function was normal.
Based on the initial presentation and elevated cardiac markers, the patient was treated for acute coronary syndrome. Enoxaparin, aspirin, intravenous nitroglycerin, and metoprolol were initiated, with subsequent symptom resolution. The next day, a coronary angiography was performed, which showed normal coronary arteries. A left ventriculogram showed distal inferior hypokinesis.
The correct answer is: D. Acute thrombosis with subsequent thrombotic resolution with antiplatelet and antithrombotic treatment related to sickle cell anemia.
We presumed the patient had acute thrombosis related to his sickle cell disease. Because there was a serial rise and fall in troponin values as well as CK-MB, the most likely etiology is an acute cardiac event.
Heterophile antibodies resulting in elevations seem unlikely, as they usually result in sustained elevations on serial testing.1
|
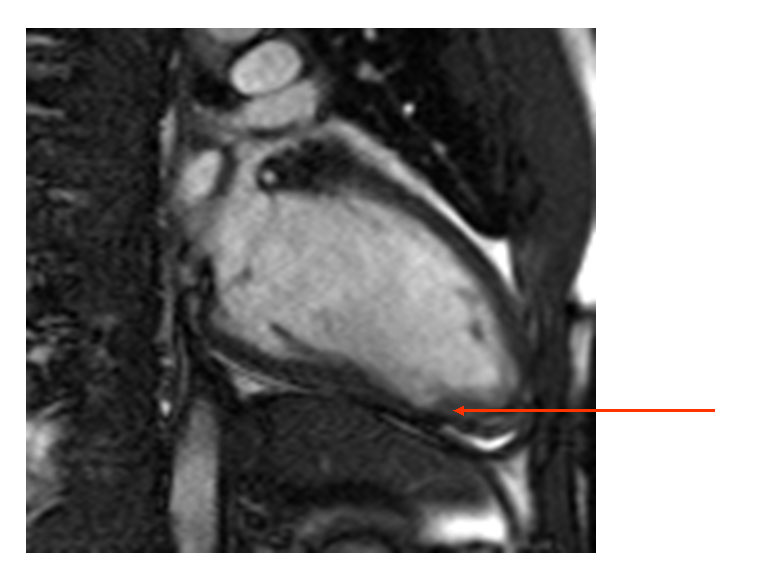
Figure 2A
|
|
|
Type II MI is a consideration; however, the patient was not significantly tachycardic, ejection fraction was normal, and there was no hypotension to result in an increased demand. In the absence of underlying cardiac abnormalities, a hemoglobin can decrease to as low as 5 g without resulting in significant effects on tissue oxygenation.
2
Pulmonary embolism is another consideration; however, oxygen saturations, RR , and RV function were all normal, making this unlikely. Troponin elevations in the setting of pulmonary embolism are typically associated with increased RV strain/dysfunction as a result of RV ischemia.3
The rise and fall in cardiac markers, and the acute MPI results in conjunction with an echocardiogram that showed a wall motion abnormality in a similar distribution, indicate that this was an acute event, with “false-negative” coronary angiography. In the TACTICS-TIMI 18 trial, 61% of patients had elevated troponins, but coronary angiography demonstrated nonsignificant disease.4 In this group of patients with nonsignificant coronary disease, the event rate in troponin (+) compared to troponin (-) patients was significantly higher.
|
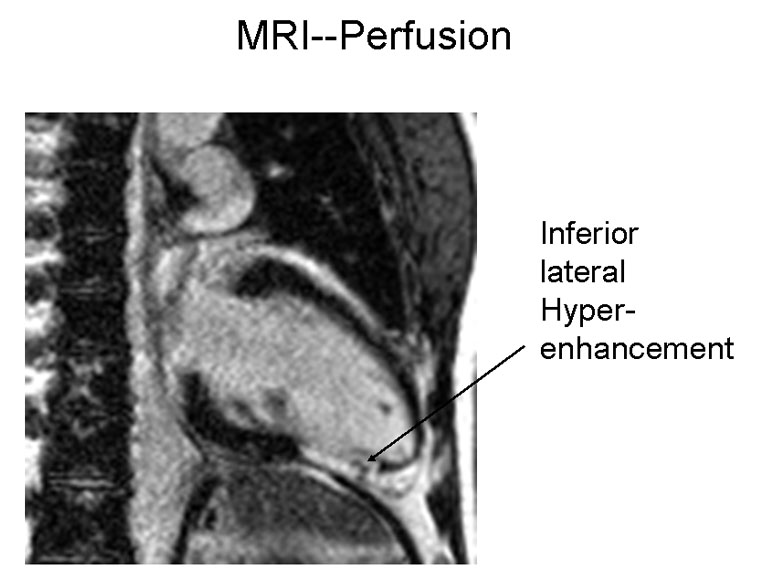
Figure 2B
|
|
|
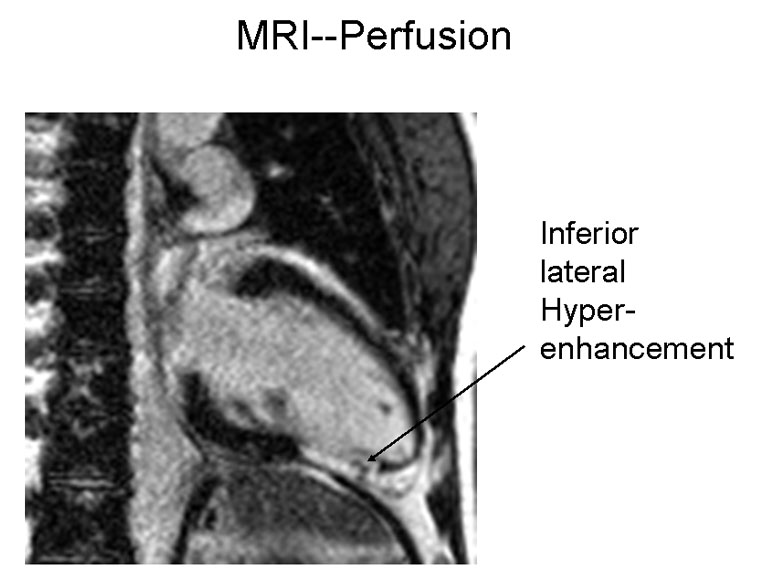
Subsequently, cardiac magnetic resonance imaging (MRI) was performed to determine whether there was an associated cardiomyopathy. This demonstrated a wall motion abnormality (Figure 2A) and a focal area of gadolinium uptake (Figure 2B) extending from the mid to distal inferior wall, consistent with transmural infarction, rather than myocarditis. The distribution was similar to the MPI and echocardiographic wall motion abnormalities. Given the lack of plaque on the angiogram and his young age, the presumptive diagnosis was acute thrombosis related to sickle cell crisis. Because of the delay in angiography, we have hypothesized that any visible thrombus resolved with antiplatelet and antithrombotic treatment.
With the increasing use of more sensitive biomarkers, patients with transient elevations are increasingly being diagnosed. Cardiac MRI is useful for differentiating between patients who have myocarditis versus those who have acute MI with normal coronary angiography.5
Accurate identification of the etiology of the myocardial damage is important to assist in determining appropriate long-term treatment, particularly in identifying patients who are appropriate candidates for secondary treatment.6
References
- Panteghini M. A critical appraisal of experimental factors influencing the definition of the 99th percentile limit for cardiac troponins. Clin Chem Lab Med 2009;47:1179-82.
- Weiskopf RB, Viele MK, Feiner J, et al. Human cardiovascular and metabolic response to acute, severe isovolemic anemia. JAMA 1998;279:217-21.
- Becattini C, Vedovati MC, Agnelli G. Prognostic value of troponins in acute pulmonary embolism: a meta-analysis. Circulation 2007;116:427-33.
-
Dokainish H, Pillai M, Murphy SA, et al., on behalf of the TACTICS-TIMI-18 Investigators. Prognostic implications of elevated troponin in patients with suspected acute coronary syndrome but no critical epicardial coronary disease: a TACTICS-TIMI-18 substudy. J Am Coll Cardiol 2005;45:19-24.
- Assomull RG, Lyne JC, Keenan N, et al. The role of cardiovascular magnetic resonance in patients presenting with chest pain, raised troponin, and unobstructed coronary arteries. Eur Heart J 2007;28:1242-9.
- Maddox TM, Ho PM, Roe M, Dai D, Tsai TT, Rumsfeld JS. Utilization of secondary prevention therapies in patients with nonobstructive coronary artery disease identified during cardiac catheterization: insights from the National Cardiovascular Data Registry Cath-PCI Registry. Circ Cardiovasc Qual Outcomes 2010;3:632-41.