A 57-Year-Old Caucasian Male Smoker Presents With Chest Discomfort and Throat Pressure | Patient Case Quiz
A 57-year-old Caucasian male smoker with no significant medical history presents with three days of chest discomfort and throat pressure. The symptoms started while he was biking and initially resolved with rest. However, they recurred later that day and continued intermittently up to the presentation.
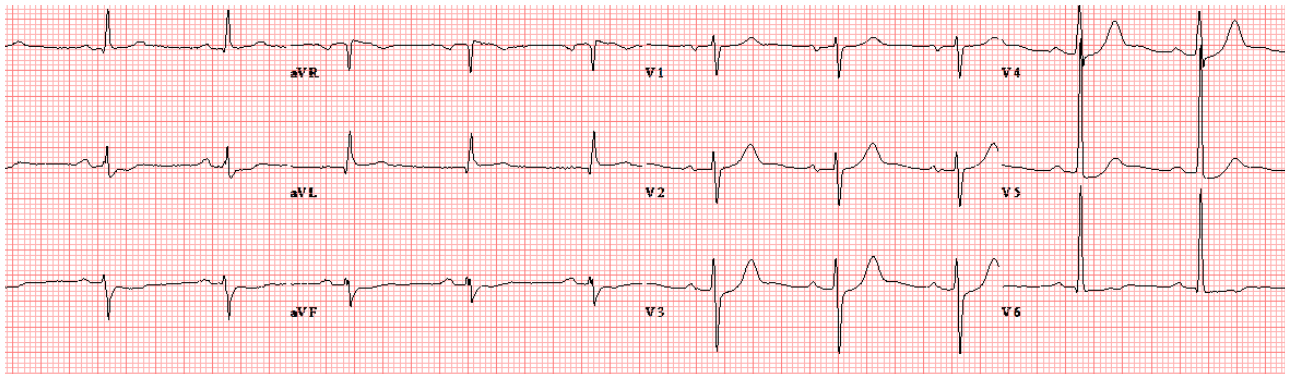
Upon arrival, he is free of chest pain. His electrocardiogram (ECG) shows mild ST-segment depressions and T wave changes in the inferior leads and lateral precordial leads (Figure 1). His initial troponin I is elevated at 17.3 ng/mL (normal value <0.05). A two-dimensional transthoracic echocardiogram shows inferior and lateral wall hypokinesis with a left ventricular ejection fraction of 40-45%.
|
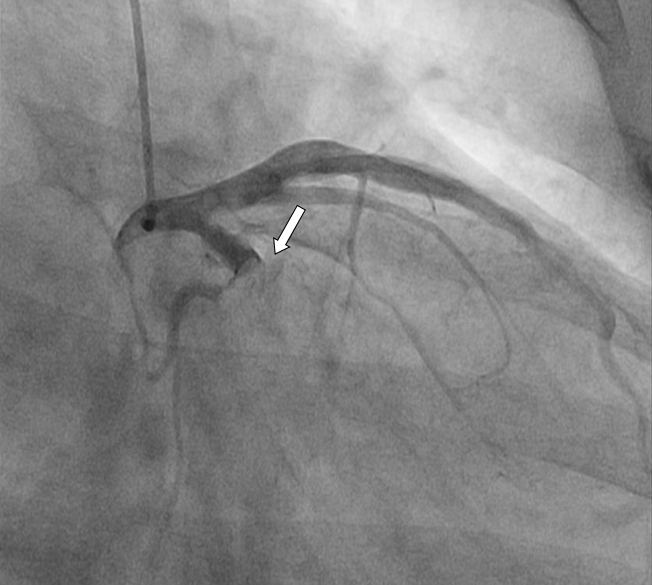
He is taken to the cardiac catheterization laboratory, and a selective coronary angiogram (Figure 2, Video 1) and left ventriculogram (Video 2) are performed.
|
|
|
Based on the clinical presentation and findings on the coronary angiogram, which of the following would be the best treatment strategy?
Show Answer
The correct answer is: C. Intravenous heparin and systemic glycoprotein IIB-IIIA infusion overnight and deferred percutaneous coronary intervention (PCI) in 48-72 hours.
The current data and guidelines support routine invasive management following non–ST-segment elevation myocardial infarction (NSTEMI).1 Total occlusion of the infarct-related artery (IRA) is not uncommonly found in NSTEMI. It is seen in up to 30% of cases and commonly affects the left circumflex coronary artery.2,3 In these cases, there is usually a large thrombus burden associated with the culprit lesion in IRA.4 Intervention in these cases is associated with higher rates of periprocedural complications and lower rates of procedural success.5 On angiography, a thrombus is defined as a filling defect with either total or partial occlusion with convex, or irregular but usually hazy margins. In addition, there is contrast retention or staining associated with the filling defect.6
Thrombus obstructing a coronary artery can lead to distal embolization during any of the steps of PCI and result in periprocedual myocardial infarction. Impaired microvascular perfusion can result in "no-reflow" phenomenon. Overall, these events can lead to larger final infarct size and poor early and late outcomes.7,8
There are several treatment strategies that can be used with a large coronary thrombus burden. Aspiration of the thrombus or mechanical thrombectomy followed by balloon angioplasty and stenting can be used when there is significant thrombus burden.9,10,11 The goal of the procedure is to debulk the thrombus and thereby prevent distal embolization.12 Among patients with STEMI in the Thrombus Aspiration during Percutaneous Coronary Intervention in Acute Myocardial Infarction Study (TAPAS) study, aspiration thrombectomy with a manual thrombus aspiration catheter resulted in improved myocardial reperfusion compared with conventional PCI, and this translated to improved clinical outcomes.13 The catheter used was of low profile and could be maneuvered over routine coronary guide wires. The Thrombus Aspiration in ST-Elevation Myocardial Infarction in Scandinavia (TASTE) trial, on the other hand, concluded that routine thrombus aspiration before PCI when compared with PCI alone had no effect on 30-day outcomes in STEMI. Aspiration thrombectomy is currently endorsed by American College of Cardiology (ACC)/American Heart Association (AHA) Guidelines on STEMI as Class IIA recommendation.10 However, recent trials did not show any benefit of thrombus aspiration when compared with conventional PCI in NSTEMI population.14 Failed aspiration can, by itself, lead to embolization and the slow-flow phenomenon.15 Additionally, delay in presentation in NSTEMI, in contrast to STEMI, may result in organization of the thrombus and make it less amenable to aspiration.16 Current guidelines do not support thrombus aspiration in patients presenting with NSTEMI.1
The second option of simple balloon angioplasty without stent placement is currently not recommended as it would increase the risk of distal particulate matter embolization with an additional risk of early and/or late vessel re-occlusion and closure due to lack of stenting. Nevertheless, it may be of benefit in few cases with no significant vessel occlusion due to thrombus.17 In our patient, however, due to a large thrombus occluding a major vessel, this would not be an option.
Distal embolic protection devices have been used as an adjunct during vein graft PCI. In the Saphenous vein graft Angioplasty Free of Emboli Randomized (SAFER) trial, use of a distal occlusion balloon with an aspiration catheter showed reduction in major adverse cardiovascular events within 30 days. A bare-metal stent with an external mesh sleeve to reduce embolization is currently available outside the U.S. to limit distal embolization when there is high thrombus burden.18 Trials with these devices in native vessel PCI have so far yielded discouraging results.15,11 The reason for the lack of benefit of these devices may be due to incomplete vessel apposition and failure to capture all the debris formed during the procedure. In addition, these devices need vessel preparation with predilation, the process that by itself leads to embolic phenomena.
A strategy of passivation with 48-72 hours of adjunctive antiplatelet and antithrobotic therapy and deferred PCI is a reasonable option especially with late presentations in stable patients. Procedural success is less likely with late presentation, as in our case, and crossing the lesion may be challenging as the thrombus is more likely to have organized. Delaying definitive intervention with interim treatment with antithrombotics, such as intravenous unfractionated heparin and antiplatelet agents, including glycoprotein IIB/IIIA inhibitors as well as P2Y12 inhibitors, may help decrease the thrombus burden and ensure procedural success with deferred PCI and stent placement.20,21
Excimer laser coronary angioplasty (ELCA) is another modality that can be used when there is large thrombus burden and works by a lysis and debulking effect of excimer laser on the thrombus and the culprit plaque.22 However, its efficacy and safety has not been tested in trials.
The patient described in this Patient Case Quiz had a late presentation and was clinically stable on presentation. There was total occlusion of the IRA with high thrombus burden. A staged strategy of deferred PCI and stenting with interim antithrombotic/antiplatelet therapy proved to be a reasonable and safe strategy.
References
- Anderson JL, Adams CD, Antman EM, et al. 2012 ACCF/AHA focused update incorporated into the ACCF/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013;61:e179-347.
- Wang TY, Zhang M, Fu Y, et al. Incidence, distribution, and prognostic impact of occluded culprit arteries among patients with non–ST-elevation acute coronary syndromes undergoing diagnostic angiography. Am Heart J 2009;157:716-23.
- Bahrmann P, Rach J, Desch S, Schuler GC, Thiele H. Incidence and distribution of occluded culprit arteries and impact of coronary collaterals on outcome in patients with non-ST-segment elevation myocardial infarction and early invasive treatment strategy. Clin Res Cardiol 2011;100:457-67.
- Escaned J, Echavarría-Pinto M, Gorgadze T, et al. Safety of lone thrombus aspiration without concomitant coronary stenting in selected patients with acute myocardial infarction. EuroIntervention 2013;8:1149-56.
- McEntegart MB, Kirtane AJ, Cristea E, et al. Intraprocedural thrombotic events during percutaneous coronary intervention in patients with non–ST-segment elevation acute coronary syndromes are associated with adverse outcomes: analysis from the ACUITY (Acute Catheterization and Urgent Intervention Triage Strategy) trial. J Am Coll Cardiol 2012;59:1745-51.
- Sherman CT, Litvack F, Grundfest W, et al. Coronary angioscopy in patients with unstable angina pectoris. N Engl J Med 1986;315:913-9.
- White CJ, Ramee SR, Collins TJ, et al. Coronary thrombi increase PTCA risk angioscopy as a clinical tool. Circulation 1996;93:253-8.
- Henriques JPS, Zijlstra F, Ottervanger JP, et al. Incidence and clinical significance of distal embolization during primary angioplasty for acute myocardial infarction. Eur Heart J. 2002;23:1112-7.
- Luca GD, Dudek D, Sardella G, Marino P, Chevalier B, Zijlstra F. Adjunctive manual thrombectomy improves myocardial perfusion and mortality in patients undergoing primary percutaneous coronary intervention for ST-elevation myocardial infarction: a meta-analysis of randomized trials. Eur Heart J 2008;29:3002-10.
- Vlaar PJ, Diercks GF, Svilaas T, et al. The feasibility and safety of routine thrombus aspiration in patients with non-ST-elevation myocardial infarction. Catheter Cardiovasc Interv 2008;72:937-42.
- Gick M, Jander N, Bestehorn H-P, et al. Randomized evaluation of the effects of filter-based distal protection on myocardial perfusion and infarct size after primary percutaneous catheter intervention in myocardial infarction with and without ST-segment elevation. Circulation 2005;112:1462-9.
- Herrmann J, Von Birgelen C, Haude M, et al. Prognostic implication of cardiac troponin T increase following stent implantation. Heart Br Card Soc 2002;87:549-53.
- Svilaas T, Vlaar PJ, van der Horst IC, et al. Thrombus aspiration during primary percutaneous coronary intervention. N Engl J Med 2008;358:557-67.
- Thiele H, de Waha S, Zeymer U, et al. Effect of aspiration thrombectomy on microvascular obstruction in NSTEMI patients: the TATORT-NSTEMI trial. J Am Coll Cardiol 2014;64:1117-24.
- Kaltoft A, Bøttcher M, Nielsen SS, et al. Routine thrombectomy in percutaneous coronary intervention for acute ST-segment–elevation myocardial infarction: a randomized, controlled trial. Circulation 2006;114:40-7.
- Waksman R, Lipinski MJ. The utility of thrombus aspiration for NSTEMI: déjà vu of aspiration for primary PCI. J Am Coll Cardiol 2014;64:1125-7.
- Escaned J, Echavarría-Pinto M, Gorgadze T, et al. Safety of lone thrombus aspiration without concomitant coronary stenting in selected patients with acute myocardial infarction. EuroIntervention 2013;8:1149-56.
- Kaluski E, Hauptmann KE, Müller R, Tsai S, Klapholz M, Grube E. Coronary stenting with MGuard: first-in-man trial. J Invasive Cardiol 2008;20:511-5.
- Haeck JDE, Koch KT, Bilodeau L, et al. Randomized comparison of primary percutaneous coronary intervention with combined proximal embolic protection and thrombus aspiration versus primary percutaneous coronary intervention alone in ST-segment elevation myocardial infarction: the PREPARE (PRoximal Embolic Protection in Acute myocardial infarction and Resolution of ST-Elevation) study. JACC Cardiovasc Interv. 2009;2:934-43.
- Kelbæk H, Engstrøm T, Ahtarovski KA, et al. Deferred stent implantation in patients with ST-segment elevation myocardial infarction: a pilot study. EuroIntervention 2013;8:1126-33.
- Tang L, Zhou S-H, Hu X-Q, Fang Z-F, Shen X. Effect of delayed vs immediate stent implantation on myocardial perfusion and cardiac function in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous intervention with thrombus aspiration. Can J Cardiol 2011;27:541-7.
- Topaz O, Ebersole D, Das T, et al. Excimer laser angioplasty in acute myocardial infarction (the CARMEL multicenter trial). Am J Cardiol 2004;93:694-701.