A 65-year-old male has symptomatic episodes of paroxysmal AF despite treatment with sotalol 80 mg twice daily or flecainide 150 mg twice daily. When he elected to discontinue antiarrhythmic medication, atrial fibrillation episodes were persistent.
His past medical history was significant for orthopedic injuries and corrective surgery, in addition to AF for the last 15 years, typically initiated after big meals and during sleep. Cardiac imaging revealed a structurally normal heart. His brother and father both had AF.
CHADS-Vasc score is 1 based on age.
Medications: Flecainide 150 mg PO BID, Verapamil 180 mg PO daily, Aspirin 81 mg PO daily and Simvastatin 20 mg at PO qHS.
ECG: Sinus rhythm with a right bundle-branch block and left anterior fascicular block, PR interval is 200 milliseconds.
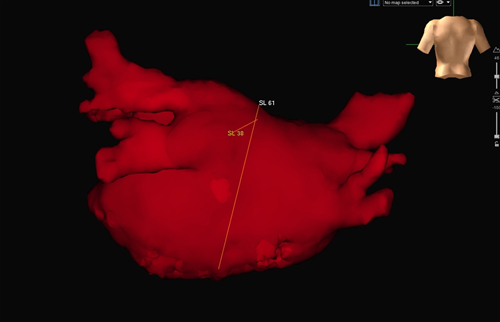
Cardiac MRI: Four pulmonary vein ostia were normal sized (range 18 - 27 mm). LVEF 58% with normal LV size and function. The late enhancement images showed no evidence of prior infarct, inflammation or infiltration of the LV myocardium. The LA antero-posterior dimension was 38 mm.
The correct answer is: E. There is no convincing data to suggest any of the above approaches is best in this case
Individual operators have developed techniques based on their own success rates and experience. The pathophysiology of progression from paroxysmal AF (self terminating episodes of less than 7 days duration) to persistent AF (episodes lasting more than 7 days requiring either electrical or pharmacological conversion) involves electrical remodeling, interstitial fibrosis and dilation of the atria.1 The AF ablation consensus document suggests that treatment of long-standing persistent AF (duration more than 1 year) should include additional substrate modification.2,3 We also employ substrate modification in addition to PVI when patients with persistent AF have significant underlying structural heart disease resulting in atrial dilation and fibrosis.
AF is initiated by 'triggers' that reside within the myocardial sleeves of pulmonary veins in a majority of patients with paroxysmal AF (94%).4 Pulmonary vein isolation remains the cornerstone of invasive therapy for both paroxysmal and persistent AF,2,3 but the results are limited by a high rate of reconnection of PV's to the LA.5 In paroxysmal AF, PVI is considered sufficient to prevent AF recurrences and additional linear LA lesions are not beneficial.3 Additionally, linear LA and CFAE ablations may increase short-term complications and atrial tachycardia. Extensive LA ablations can also give rise to LA chamber stiffening and potentially pulmonary hypertension.6 Until there is a reliable means of creating durable PVI, it will be difficult to ascertain its relative contribution to AF prevention in patients with persistent or long-standing persistent AF.
Most experienced operators distinguish between persistent AF that is less than a year's duration and long-standing persistent AF as an important factor in deciding ablation targets. Our patient has persistent AF when he avoids taking antiarrhythmic medication, but has an apparently structurally normal heart and no significant co-morbidity. Obviously, there is a poorly understood factor that leads to persistence of AF in this patient, perhaps genetically predisposed based on his family history. Therefore an initial strategy of pulmonary vein isolation alone is reasonable given the potential problems with additional substrate modification and lack of clear benefit. This decision was supported by AF initiated from the left PV's during the procedure and terminating during PVI.
References
- Schoonderwoerd BA, Van Gelder IC, Van Veldhuisen DJ, Van den Berg MP, Crijns HJ. Electrical and structural remodeling: role in the genesis and maintenance of atrial fibrillation. Prog Cardiovasc Dis 2005; 48:153-168.
- Calkins H, et al. HRS/EHRA/ECAS Expert Consensus Statement on catheter and surgical ablation of atrial fibrillation: recommendations for personnel, policy, procedures and follow-up. A report of the Heart Rhythm Society (HRS) Task Force on catheter and surgical ablation of atrial fibrillation. Heart Rhythm 2007; 4:816-861.
- Parkash R, Tang AS, Sapp JL, Wells G. Approach to the catheter ablation technique of paroxysmal and persistent atrial fibrillation: a meta-analysis of the randomized controlled trials. J Cardiovasc Electrophysiol 2011; 22:729-738.
- Haissaguerre M, et al. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N Engl J Med 1998; 339:659-666.
- McGarry, T.J. & Narayan, S.M. The anatomical basis of pulmonary vein reconnection after ablation for atrial fibrillation: wounds that never felt a scar? J Am Coll Cardiol 2012; 59:939-941.
- Shoemaker, M.B., et al. Left atrial hypertension after repeated catheter ablations for atrial fibrillation. J Am Coll Cardiol 2011; 57: 1918-1919.