A 59-year-old hypertensive male who had a repair of a type A aortic dissection 20 years ago is referred to you for an enlarging thoracic aorta. The patient is asymptomatic, but on routine follow-up with serial computed tomography (CT) imaging, his aortic root is now 5.6 cm, the chronically dissected arch is 5.8 cm, and he has an extent II thoracoabdominal aneurysm and dissection with a maximal diameter of 6.5 cm involving the entire descending and thoracoabdominal aorta. Transthoracic echocardiography reveals a dilated aortic root, moderate aortic insufficiency, left ventricular end-diastolic dimension 61 mm, and ejection fraction 55%. Coronary angiography shows non-obstructive coronary artery disease.
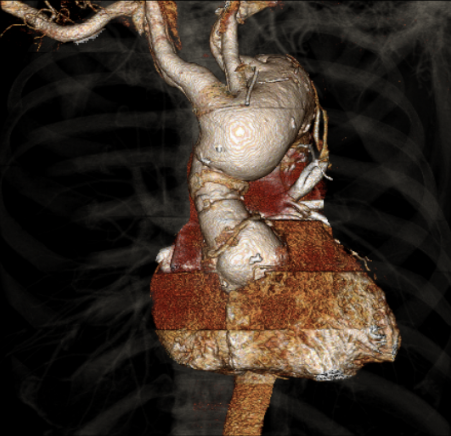
Figure 1
Preoperative CT scan showing an aortic root aneurysm, the previous ascending repair, and aortic arch aneurysm.
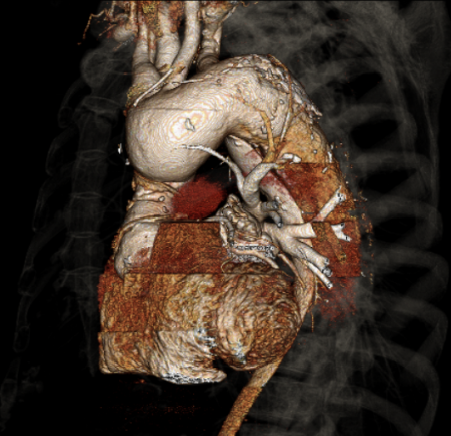
Figure 2
Aortic arch aneurysm extends into a descending thoracic and thoracoabdominal aneurysm.
The correct answer is: C. Repair the aortic root and arch under deep hypothermic circulatory arrest using an "elephant trunk" technique, followed by an open extent II thoracoabdominal aneurysm repair in a separate procedure.
This patient has aneurysmal growth of all segments of his aorta that have not already been replaced during the type A dissection repair. According to the Crawford classification of thoracoabdominal aneurysms, this patient has an extent II thoracoabdominal aneurysm, which is an aneurysm that involves the aorta from the left subclavian artery down to the aortic bifurcation. Extent I aneurysms extend from the left subclavian artery to the visceral segment above the renal arteries, extent III aneurysms from the mid descending thoracic aorta to below the renal arteries, and extent IV aneurysms involve the visceral segment from the celiac artery to below the renal arteries.
Continuing with medical management is inappropriate since the size of the aorta in all involved segments exceeds 5.5 cm, which is the limit for which repair is recommended to prevent another aortic catastrophe.1 He will require an extensive repair involving the aortic root, aortic arch, and the entire thoracoabdominal aorta, which can be done with low mortality in experienced centers.2
Although the largest segment of the aorta is the thoracoabdominal portion, the aneurysms in the more proximal aorta and the aortic insufficiency preclude the distal segment from being repaired first. The optimal sequence is to perform an aortic root reconstruction and a total arch replacement as an initial procedure. During the arch replacement, an "elephant trunk" should be left in place in the descending thoracic aorta so that obtaining proximal control during the thoracoabdominal aneurysm repair will be easier. Without an elephant trunk, obtaining proximal control of a prosthetic arch graft is quite hazardous due to extensive postoperative adhesions leading to significant risk for injury to surrounding structures, such as the pulmonary artery, recurrent laryngeal nerve, and esophagus. After the initial procedure, the patient should be allowed to fully recover from surgery and then be brought back for an open thoracoabdominal aneurysm repair. Although this two-stage strategy delays repair of a large thoracoabdominal aneurysm, the majority of patients survive to the second stage.3
In the "frozen elephant trunk" procedure, a long stent-graft is deployed antegrade into the descending thoracic aorta during the aortic arch replacement. With an extent II thoracoabdominal aneurysm, the trunk would likely have no distal seal, and it would not be possible to repair the visceral segment using this technique. Additionally, this technique is associated with a significant rate of spinal cord injury, which is not seen in traditional aortic arch surgery.4
A single-stage approach via a bilateral clamshell thoracotomy has been successfully used to repair extensive aneurysmal disease involving the entire ascending, arch, descending, and thoracoabdominal aorta.5 However, this experience is limited mainly to one center and additional experience in other centers is needed before the approach can be generally recommended.
Fenestrated/branched stent grafting for thoracoabdominal aortic aneurysms is in development. Results on the use of this technique for chronic dissections is limited. Although less invasive than open surgery, this technique is associated with morbidity and mortality rates similar to open surgery and a surprisingly high rate of spinal cord injury of as high as 16% even in experienced centers.6
Figure 3
Follow-up CT scan after first stage reconstruction with aortic root reconstruction and total arch repair with an elephant trunk procedure.
References
- Hiratzka LF, Bakris GL, Beckman JA, et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. Circulation 2010;121:e266-369.
- Coselli JS, Bozinovski J, LeMaire SA. Open surgical repair of 2286 thoracoabdominal aortic aneurysms. Ann Thorac Surg 2007;83:S862-4; discussion S890-2.
- Svensson LG, Rushing GD, Valenzuela ES, et al. Modifications, classification, and outcomes of elephant-trunk procedures. Ann Thorac Surg 2013;96:548-58.
- Di Eusanio M, Pantaleo A, Murana G, et al. Frozen elephant trunk surgery-the Bologna's experience. Ann Cardiothorac Surg 2013;2:597-605.
- Kouchoukos NT, Kulik A, Castner CF. Clinical outcomes and fate of the distal aorta following 1-stage repair of extensive chronic thoracic aortic dissection. J Thorac Cardiovasc Surg 2013;146:1086-91.
- Oikonomou K, Kopp R, Katsargyris A, Pfister K, Verhoeven EL, Kasprzak P. Outcomes of fenestrated/branched endografting in post-dissection thoracoabdominal aortic aneurysms. Eur J Vasc Endovasc Surg 2014;48:641-8.