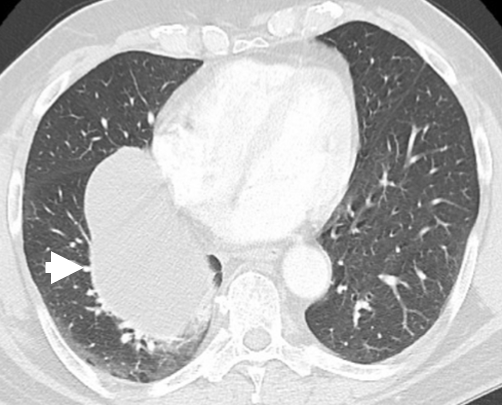
A 64-year-old gentleman with a 47 pack per year history presents to an outpatient cardiology clinic after a computed tomography (CT) scan of the chest (Figure 1) demonstrates a large mass in the mediastinum. The CT scan was performed by his family medicine physician for lung cancer screening given his age and smoking history. He has not had any symptoms to date. Specifically, he denies any dyspnea, cough, chest discomfort, fevers, weight loss, palpitations, or fatigue. He works full time as a building inspector and has not traveled outside of the country in the past 10 years. There is no history of prior surgeries. An exercise electrocardiography treadmill stress test taken a month prior was negative for ischemia.
Figure 1: Chest CT demonstrating a discrete, low-attenuation mediastinal lesion (white arrowhead) close to the right atrium and right paravertebral region measuring 12.2 x 8.0 cm in the maximum anterior-posterior and transverse dimensions, respectively.
On physical exam, his pulse is 77 beats per minute, blood pressure is 115/75 mmHg, and oxygen saturation is 98% on room air. Lungs are clear to auscultation bilaterally. Heart sounds are regular without any friction rub or murmur. Jugular venous pressure is within normal limits.
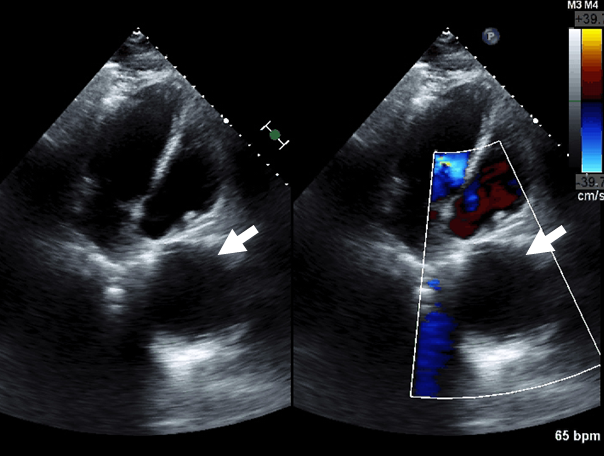
His transthoracic echocardiogram (Figure 2) shows an echolucent pericardial structure with normal biventricular size and function. T1- and T2-weighted cardiac magnetic resonance imaging (MRI) (Figure 3) confirms a large 12.1 cm x 8 cm pericardial mass located at the right cardiophrenic angle. There is no mass effect to the adjacent right atrium or inferior vena cava. No pericardial effusion and no evidence of hemodynamic compromise were found.
Figure 2: Transthoracic echocardiogram with echolucent space (white arrow) evident adjacent to the right atrium in the apical four chamber view corresponding to a pericardial mass.
Figure 3: Cardiac MRI with 12.1 x 8 cm, thin-walled, pericardial mass (white arrowhead) of the posterior right pericardium with the medial border abutting the inferior vena cava and right atrium.
The correct answer is: B. Obtain a cardiac MRI in 1 year.
The patient has a simple, large pericardial cyst. Pericardial cysts are benign intrathoracic lesions that occur in one person per 100,000 and constitute 7% of all mediastinal tumors.1 They are commonly located at the right cardiophrenic angle (51-70%) as in this patient, but also observed at the left cardiophrenic angle (28-38%), and, rarely, in other locations not adjacent to the diaphragm (8-11%).2,3 They typically range in size from 2 to 5 cm, but giant cysts up to 28 cm have been reported in the literature.4 While most cysts are congenital in origin, they can also be acquired as a sequelae of prior cardiothoracic surgery.
Imaging can be very useful in distinguishing a pericardial cyst from other etiologies in the same location. The differential diagnosis for a pericardial cyst includes a pericardial diverticulum, prominent fat pad, ventricular or coronary aneurysm, tumor or a loculated pericardial effusion.5 Cysts do not communicate with the pericardial space, whereas diverticula do.6 As a result, diverticula can change in size (often decreasing) over a short period of time. A prominent epicardial or paracardiac fat pad can easily be distinguished by CT or MRI since fat has a lower density than the water density of the fluid contained within pericardial cysts.7 Color and spectral Doppler can help in differentiating a pericardial cyst from other vascular structures such as a coronary aneurysm.5 Pericardial tumors are rare with lipomas being the most common benign lesion.8 In contrast to a simple cyst, lipomas are echogenic on transthoracic echocardiography (TTE). Mesothelioma is the most common primary malignant pericardial neoplasm.9 On CT/MRI, it appears as a heterogeneously enhancing mass. Typically, pericardial cysts appear on CT images as well-defined, nonenhancing, fluid-attenuation lesions.10 Simple cysts are homogenous and contain no internal septa as opposed to loculated effusions. In some cases, a pericardial cyst can be differentiated from a loculated pericardial effusion by the presence of a thin wall separating the cyst from the main pericardial space.11 On cardiac MRI, cysts demonstrate intermediate to low signal intensity on T1-weighted images and high signal intensity on T2-weighted images.10 While TTE is an excellent initial test to confirm clinical diagnosis, CT or cardiac MRI provides better tissue characterization and is recommended for routine follow-up of asymptomatic cysts.4 Of the two options, MRI may be the best choice as it does not expose the patient to unnecessary radiation over time.
The natural history of a pericardial cyst has not been adequately studied. Preliminary results from a single-center, retrospective study showed that majority of pericardial cysts do not change over a mean follow-up period of 2 years, while one-third of the cysts decreased in size.12 Thus, interval enlargement of cysts in 2 years or less is rare and frequent imaging is likely not beneficial.
The correct answer from the clinical vignette is to obtain a cardiac MRI in 1 year given that the patient has an asymptomatic pericardial cyst. The diagnosis is clear at this point and a TTE with contrast will not provide further incremental value. Echinococcal hydatid cysts usually occur in the lungs or liver, but can also be observed in the pericardium in 0.5-3% of cases.13,14 The treatment of choice for echinococcal cysts is percutaneous aspiration and instillation of ethanol or silver nitrate after pre-treatment with albendazole (800 mg/day for 4 weeks).15 Surgical resection is not indicated in this situation. NSAIDS would be considered first line for pericarditis, but are not indicated for simple pericardial cysts.
Follow-up:
The patient returned to clinic 2 months later with a subacute, dry cough that has been present since his last visit. During this time period, he also reports chest pain that is exacerbated by lying down. He has pulmonary function testing performed that show mild restriction, but otherwise unremarkable. He has a repeat chest CT that shows stable appearance of the pericardial cyst, unchanged in size or location.
Now that the patient is symptomatic, surgery is the best course of action. When symptoms occur in pericardial cysts, they are due to the pressure of the cysts on adjacent organs. Compression of the heart or impedance of venous return can cause dyspnea, palpitations, chest pain, or a dry cough.11 The presence of symptoms, enlarging size, and potential for complications are all indications for surgical resection. The rare but serious complications of a large, pericardial cyst include rupture,16 erosion of the cyst into adjacent structures, such as the right ventricular wall or the superior vena cava,17,18 focal cardiac tamponade,19 mitral valve prolapse,20 bronchial obstruction,3,21 atrial fibrillation,22 pericarditis, and even sudden death.23 Minimally invasive thoracoscopic resection of a pericardial cyst with robotic or video-assisted technology is the favored alternative to open surgical resection because it minimizes surgical trauma and postoperative pain, has a shorter recovery period, and a better cosmetic outcome.24,25 If a patient is not a surgical candidate, cyst aspiration is a reasonable option.
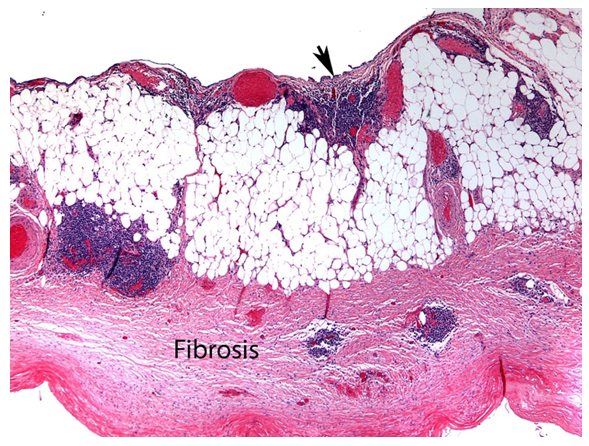
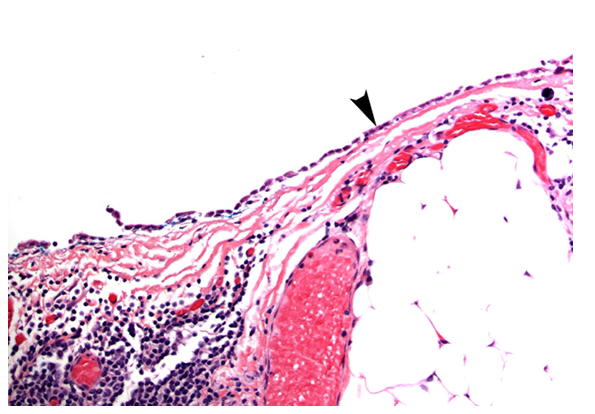
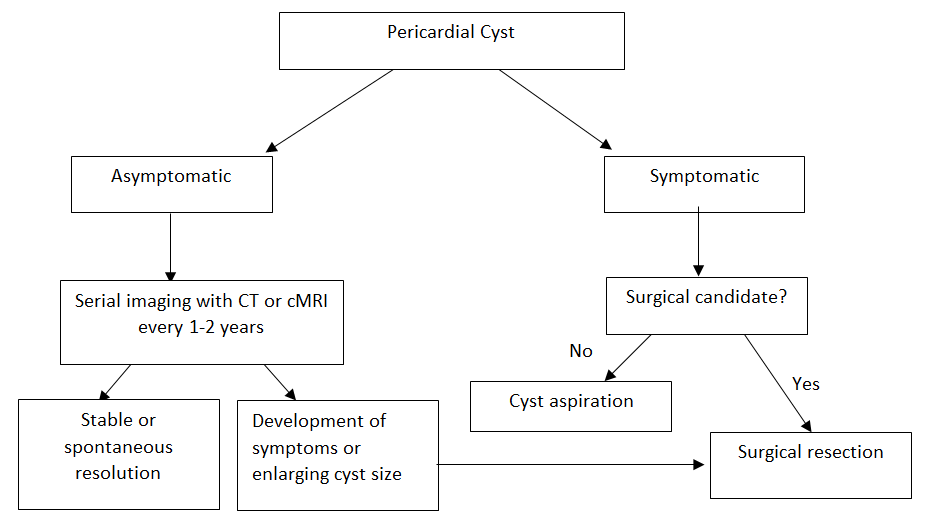
The patient underwent robotic-assisted thoracoscopic resection of his cyst without complications. Pathology is shown below (Figures 4a and 4b). Histologically, simple pericardial cysts are fluid-filled sacs lined with a single layer of mesothelial cells with the remainder of the wall composed of collagen and elastic fibers. Chronic inflammatory cells can also be observed within the cyst wall. The algorithm for the diagnostic and therapeutic workup for a pericardial cyst is shown in the diagram below. The patient recovered from surgery without incident and his chest pain and cough subsequently resolved.
Figure 4a: Cross section of cyst wall with fibromuscular tissue with collagen and elastic fibers (Fibrosis), chronic inflammation and mesothelial lining (black arrowhead). (Hematoxylin and eosin; 40x)
Figure 4b: Cyst wall with cuboidal epithelial lining (black arrowhead). (Hematoxylin and eosin; 100x)
Figure 5: Algorithm for diagnostic and therapeutic workup of a pericardial cyst.
References
- Hynes JK, Tajik AJ, Osborne MJ, Orszulak TA, Seward JB. Two-dimensional echocardiographic diagnosis of pericardial cyst. Mayo Clin Proc 1983;58:60-3.
- Stoller JK, Shaw C, Matthay RA. Enlarging, atypically located pericardial cyst. Recent experience and literature review. Chest 1986;89:402-6.
- Feigin DS, Fenoglio JJ, McAllister HA, Madewell JE. Pericardial cysts. A radiologic-pathologic correlation and review. Radiology 1977;125:15-20.
- Braude PD, Falk G, McCaughan BC, Rutland J. Giant pericardial cyst. Aust NZ J Surg 1990;60:640-1.
- Patel J, Park C, Michaels J, Rosen S, Kort S. Pericardial cyst: case reports and a literature review. Echocardiography 2004;21:269-72.
- Klein AL, Abbara S, Agler DA, et al. American Society of Echocardiography clinical recommendations for multimodality cardiovascular imaging of patients with pericardial disease. J Amer Soc Echocardiogr 2013;26:965-1012.
- Rogers CI, Seymour EQ, Brock JG. Atypical pericardial cyst location: the value of computed tomography. J Comput Assist Tomogr 1980;4:683-4.
- Restrepo CS, Vargas D, Ocazionez D, Martinez-Jimenez S, Betancourt Cuellar SL, Gutierrez FR. Primary pericardial tumors. RadioGraphics 2013;33:1613-30.
- Kaul TK, Fields BL, Kahn DR. Primary malignant pericardial mesothelioma: a case report and review. J Cardiovasc Surg 1994;35:261-7.
- Yared K, Baggish AL, Picard MH, Hoffmann U, Hung J. Multimodality imaging of pericardial diseases. JACC Cardiovasc Imaging 2010;3:650-60.
- Najib MQ, Chaliki HP, Raizada A, Ganji JL, Panse PM, Click RL. Symptomatic pericardial cyst: a case series. Eur J Echocardiogr 2011;12:E43.
- Alkharabsheh S, Ayache A, Al Halabi S, et al. Pericardial cysts: do they grow over time? J Am Coll Cardiol. 2016;67:1752.
- Rena, O, Garavoglia M, Francini M, Bellora P, Oliaro A, Casadio C. Solitary pericardial hydatid cyst. J Cardiovasc Surg 2004;45:77-80.
- Hidron A, Vogenthaler N, Santos-Preciado JI, Rodriguez-Morales AJ, Franco-Paredes C, Rassi A. Cardiac involvement with parasitic infections. Clin Microbiol Rev 2010;23:324-49.
- Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for diagnosis and management of pericardial diseases: the Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC) endorsed by the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2015;36:2921-64.
- Pradder FA, Conrad AR, Manzar KJ, Thayapran N, Jonas EE, Freeman I. Echocardiographic diagnosis of pericardial cyst. Am J Med Sci 1997;313:191-2.
- Chopra PS, Duke DJ, Pellet JR, Rahko PS. Pericardial cyst with partial erosion of the right ventricular wall. Ann Thorac Surg 1991;51:840-1.
- Mastroroberto P, Chello M, Bevacqua E, Marchese AR. Pericardial cyst with partial erosion of the superior vena cava: an unusual case. J Cardiovas Surg 1996;37:323-4.
- Bandeira FC, de Sá VP, Moriguti JC, et al. Cardiac tamponade: an unusual complication of pericardial cyst. J Am Soc Echocardiogr 1996;9:108-12.
- Kruger SR, Michaud J, Cannom DS. Spontaneous resolution of a pericardial cyst. Am Heart J 1985;109:1390-1.
- Davis WC, German JD, Johnson NJ. Pericardial diverticulum causing pulmonary obstruction. Arch Surg 1961;82:285-9.
- Vlay SC, Hartman AR. Mechanical treatment of atrial fibrillation: removal of pericardial cyst by thorascopy. Am Heart J 1995;129:616-8.
- Fredman CS, Parsons SR, Aquino TI, Hamilton WP. Sudden death after a stress test in a patient with a large pericardial cyst. Am Heart J 1994;127:946-50.
- Szinicz G, Taxer F, Riedlinger J, Erhart K. Thoracosocopic resection of a pericardial cyst. Thorac Cardiovasc Surg 1992;40:190-1.
- Abad C, Rey A, Feijoo J, Gonzalez G, Martin-Suarez J. Pericardial cyst: surgical resection in two symptomatic cases. J Cardiovasc Surg 1996;37:199-202.