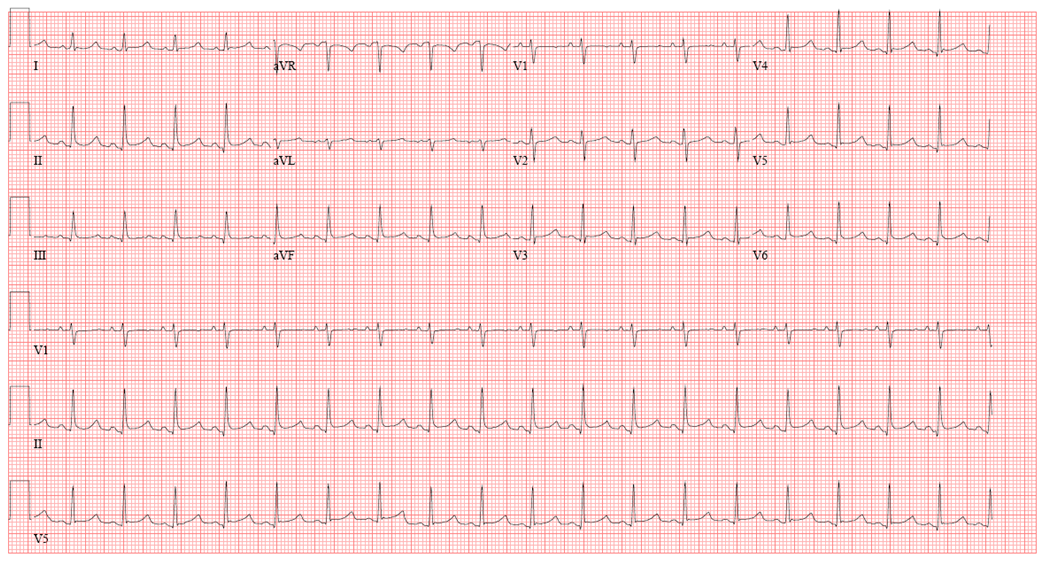
| Figure 1: 12 Lead ECG |
|
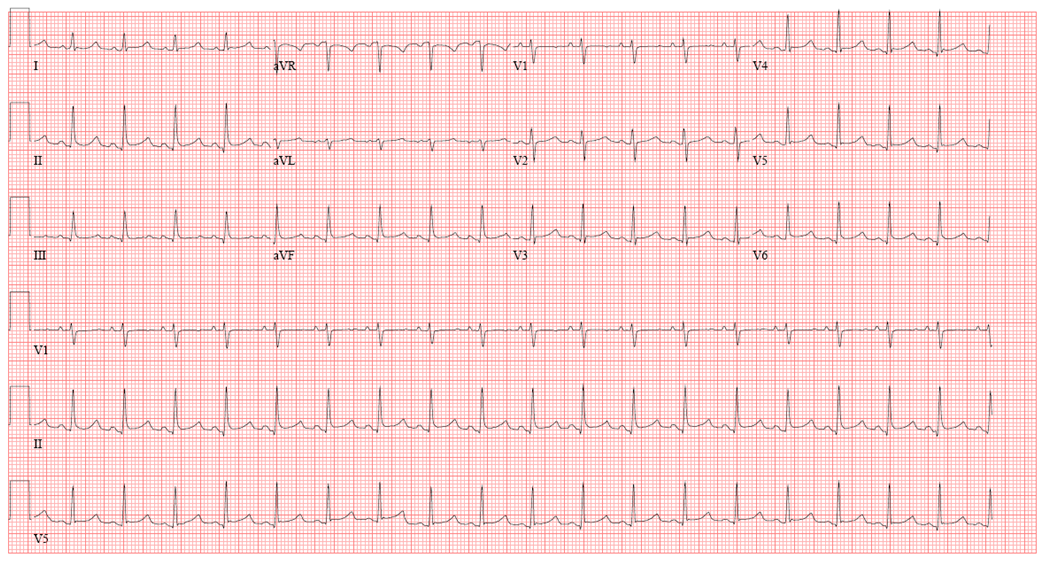
12 Lead ECG shows diffuse ST elevations (most prominent in leads V4-V6, II, aVF) with diffuse PR depressions (most notable in V5-V6) and PR elevation in lead aVR.
|
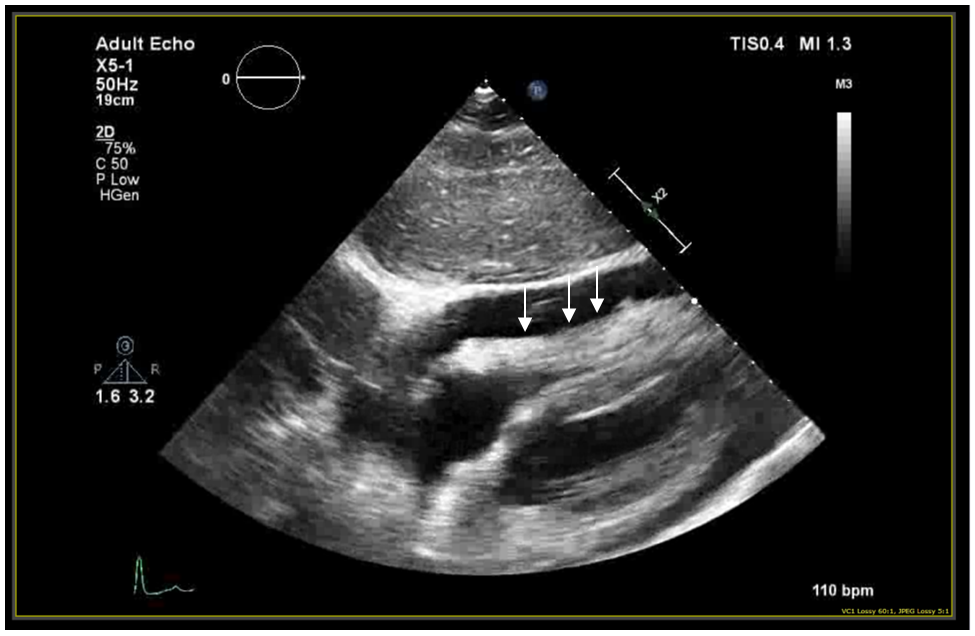
| Figure 2: Echocardiogram |
|
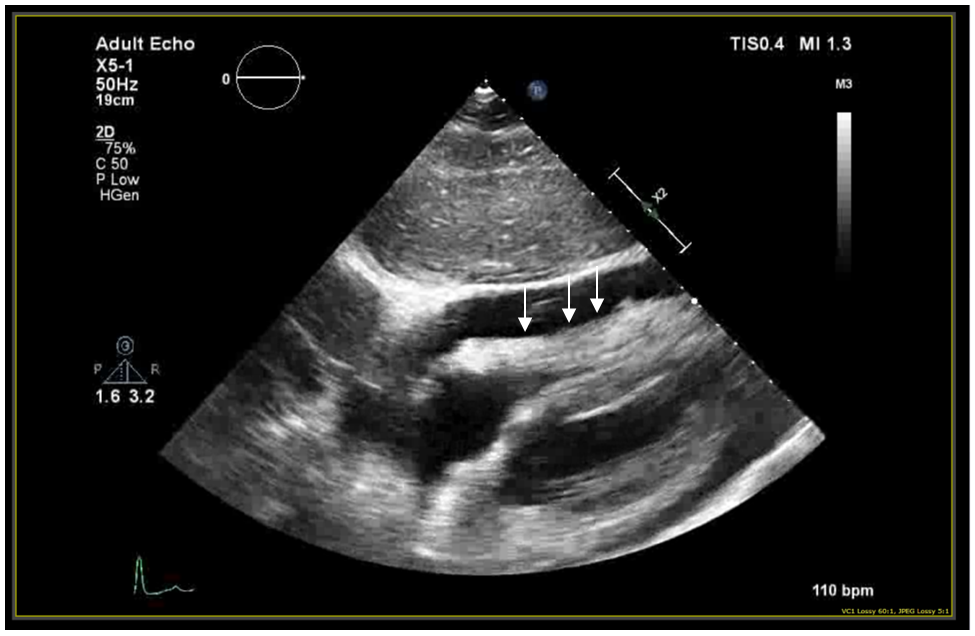
Transthoracic echocardiogram with subcostal window showing right ventricular diastolic collapse (arrows).
|
| Figure 3: Cardiac MRI |
|

Cardiac magnetic resonance image in the sagittal projection with delayed hyperenhancement of the pericardium after gadolinium administration. The markedly increased pericardial signal (arrows) suggests ongoing inflammation.
|
|
A 43-year-old woman with a past medical history notable only for tobacco use presented to the hospital with chest pain and dyspnea.
The chest pain was substernal, sharp, pleuritic, and radiated to both shoulders. It had been present for two days but became progressively worse and was associated with dyspnea which prompted her to present for medical attention. She also noted that she had an upper respiratory infection that started about a week before these symptoms began. She had a family history of sarcoidosis but no personal history of any autoimmune disorder.
Initial vital signs were notable for tachycardia at 120 beats per minute. Physical exam was normal and no friction rub was auscultated on exam.
Initial ECG (Fig 1) showed diffuse ST elevations with PR depression and an initial echocardiogram showed a large circumferential pericardial effusion with right ventricular collapse (Fig 2). An erythrocyte sedimentation rate was elevated at 60mm/h.
She underwent urgent pericardiocentesis with removal of 400cc of straw colored fluid. Cytopathology noted many inflammatory cells with no malignant cells. A viral respiratory panel was negative. Cardiac magnetic resonance imaging (Fig 3) after pericardiocentesis suggested ongoing pericardial inflammation.
The correct answer is: D. 3 Months
Initial therapy for acute idiopathic or viral pericarditis involves high dose anti-inflammatory medications. Typically this involves a high dose non-steroidal anti-inflammatory drug (NSAID) (ibuprofen 1600-3200mg/day or aspirin 2-4g/day) and colchicine at 0.6mg twice daily. (0.6mg daily for patients less than 70kg). The NSAID is usually tapered off after 2-3 weeks provided the patient has symptomatic improvement1-2. Often the tapering can be longer over several months if there is no symptom relief. For idiopathic pericarditis ibuprofen is typically preferred over other NSAIDs due to dose range and availability. In general, steroids should be avoided in the case of viral or idiopathic pericarditis however in advanced cases with constrictive physiology features and severe pericardial enhancement, triple therapy including steroids may be necessary (see below). High dose aspirin (2-4g/day) is used for pericarditis in the setting of recent acute coronary syndrome as NSAIDs should be avoided in this setting. Colchicine has been shown to prevent recurrence of pericarditis after an initial episode in the COPE trial3. In this study, patients were treated for 3 months before colchicine was discontinued. Recently a CMR guided approach to treating pericarditis has been suggested by staging the severity of the disease and modulating a slow tapering of the anti-inflammatories4.
References
- LeWinter ML. Clinical Practice. Acute Pericarditis N Engl J Med 2014; 371: 2410-2416
- Imazio M, Demichelis B, Parrini I, et al. Day-hospital treatment of acute pericarditis: a management program for outpatient therapy J Am Col Card 2004; 43: 1042-1046
- Imazio M, Bobbio M, Cecchi E, et. al. Colchicine in addition to conventional therapy for acute pericarditis: results of the COlchicine for acute PEricarditis (COPE) trial Circulation 2005; 112: 2012-2016
- Alraies MC, AlJaroudi W, Yarmohammadi H et al. Magnetic resonance-guided management in patients with recurrent pericarditis Am J Cardiol 2015: 115:542-547