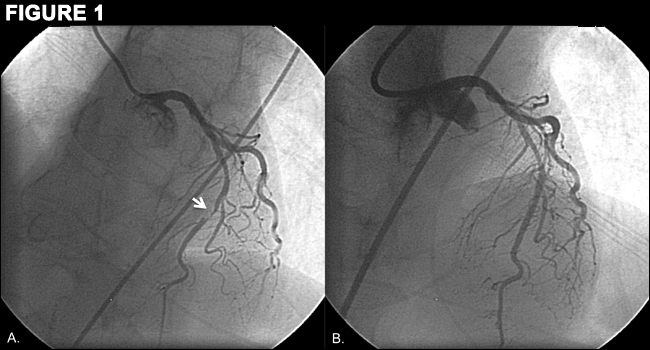
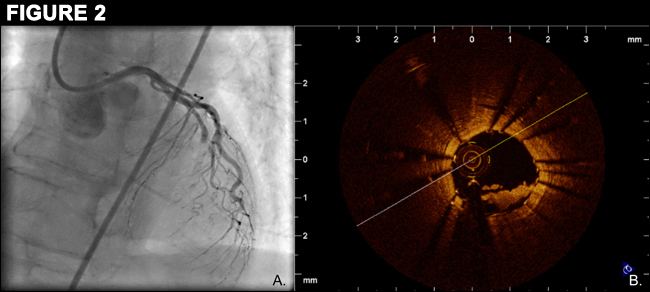
A 68-year-old woman had been admitted to the hospital with non-STEMI and was found to have a 95% mid left anterior descending (LAD) artery stenosis (Figure 1A). The lesion was treated with a 2.50x18 mm Everolimus-eluting stent during bivalirudin infusion (Figure 1B). The patient was loaded with clopidogrel 600 mg as bivalirudin was discontinued. The patient experienced chest pain with anterior ST-segment elevations 70-minutes later. Emergent angiography demonstrated acute stent thrombosis (AST, Figure 2A). On heparin and eptifibatide, low-pressure angioplasty was performed. Optical coherence tomography (OCT) imaging revealed an area of minimal malapposition and a low-attentuation intravascular mass consistent with platelet-rich thrombus within the stent (Figure 2B). The stent was post-dilated and intravenous heparin and eptifibatide infusions were continued for 12 hours.