An 82-Year-Old Man With Worsening Exercise Tolerance
|
|
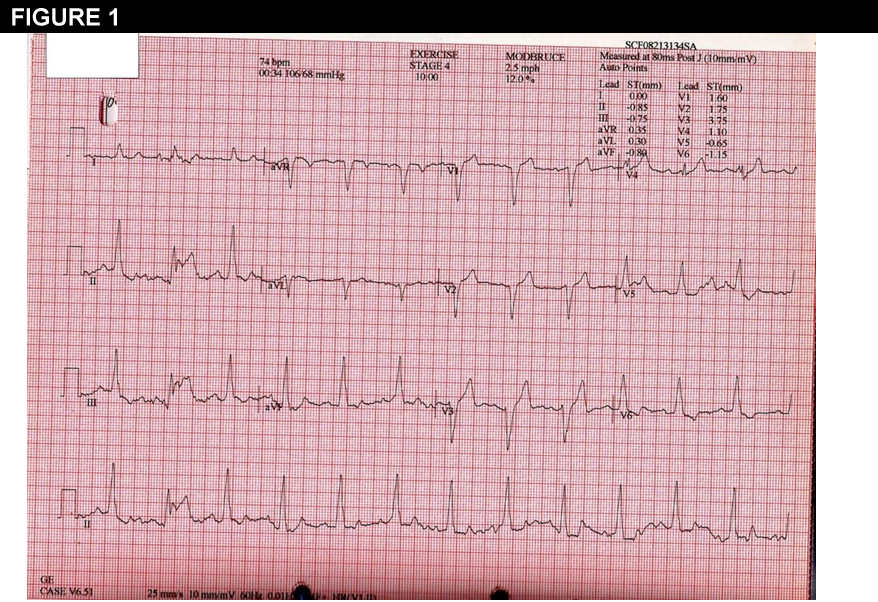
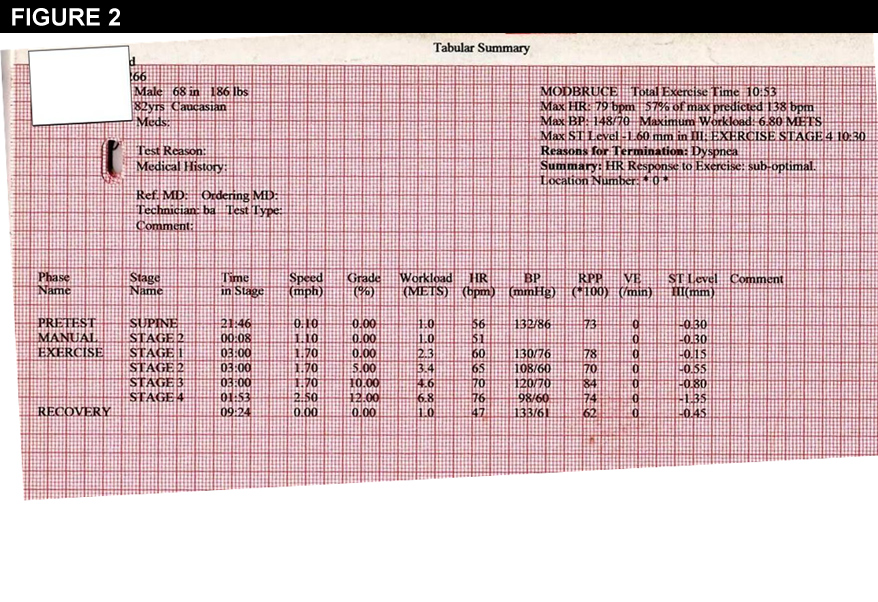
Stress test results are shown in the box.
You now refer the patient for
Show Answer

|
|
Stress test results are shown in the box.
Show Answer
The correct answer is: A. Cardiac catheterization
The stress test clearly demonstrates chronotropic incompetence. Exercise requires that the body increase oxygen uptake, by up to four times during maximal exercise. To achieve this, heart rate doubles, while stroke volume and arterio-venous oxygen difference increase to lesser degrees.1 An inability to increase heart rate during exercise will thus result in inability to meet the metabolic demands of exercise. While the best formula to describe age-predicted maximal heart rate is a matter of debate, it is well-known that heart rate response to exercise declines predictably with age, due to changes in intrinsic heart rate as well as response to catecholamines, which is the primary etiology of age-related declines in exercise tolerance.2 How best to diagnose chronotropic incompetence as the etiology of exercise intolerance is also a matter of debate. While a heart rate increase on a graded treadmill exercise test of less than 80% of the age-predicted maximum provides the simplest definition, this is highly effort-related. Thus, more sophisticated methods using expired gas exchange to confirm effort.3 In this case, the patient's continuation to stage 4 of the protocol despite increasing dyspnea left his effort in no doubt.
In this case, the correct answer for the next step is A, cardiac catheterization. In general, chronotropic incompetence is associated with perfusion defects, and also independently associated with increased cardiac mortality. Those with both chronotropic incompetence and a perfusion defect, as this patient had, are at highest risk, suggesting this group is deserving of aggressive investigation and treatment.4
Angiography revealed only a 40% stenosis of the right coronary with no other lesions, so decision was made to proceed with dual-chamber pacemaker implantation (choice C). The 2013 consensus statement from the Heart Rhythm Society and American College of Cardiology5 recommends dual-chamber pacing over single-chamber ventricular pacing for patients with sinus node dysfunction as supported by the highest level of evidence. Because of the high rate of development of AV block in patients with sinus node dysfunction (3-35),6 this statement also recommends dual-chamber over single-chamber atrial pacing for most patients, although randomized trials are lacking. While this patient has a left bundle branch block, data are lacking regarding use of cardiac resynchronization in patients with normal ejection fractions.
Following implantation of a rate-adaptive pacemaker, this highly active 82-year-old was able to resume his prior exercise regimen and continued to do well.
References
© 2026 American College of Cardiology Foundation. All rights reserved.