Aortitis With Ostial Right Coronary Artery Involvement | Patient Case Quiz
|
A 64 year-old woman with hypertension and inflammatory arthritis presents with two months of shortness of breath with exertion. She is unable to climb a flight of stairs or take out the trash without significant dyspnea. She has no fevers, cough, angina, claudication, paroxysmal nocturnal dyspnea, orthopnea, or leg swelling. Medications include verapamil, adalimumab, and aspirin. On physical examination vital signs are within normal limits with equal blood pressures in both arms. Jugular venous pressure is <5 cm H20; heart rhythm is regular; normal S1 and S2 without murmurs, gallops, or rubs; normal peripheral pulses; and a left subclavian bruit. Lungs are clear bilaterally, and abdominal exam is benign. Initial laboratory work-up is significant for erythrocyte sedimentation rate >100 mm/hr. She is prescribed prednisone 60 mg/day by her primary care physician with improvement in inflammatory markers but persistent symptoms. She is referred for further evaluation.
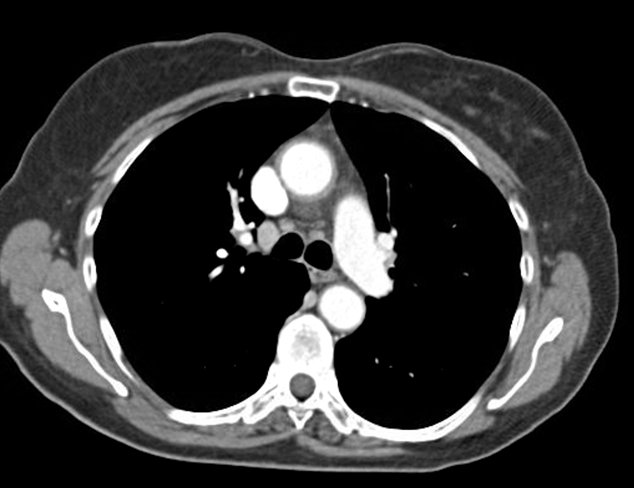
Computed tomography (CT) of the chest (Figure 1) demonstrates concentric wall thickening around the ascending aorta extending to the thoracic and abdominal aorta, consistent with aortitis. Exercise stress echocardiogram shows normal ventricular function but is non-diagnostic for ischemia as the test was terminated early due to dizziness and shortness of breath (7.0 metabolic equivalents, 62% maximal predicted heart rate). Coronary angiogram (Figure 2) demonstrates severe ostial narrowing of a dominant right coronary artery and otherwise angiographically normal coronary arteries including the left main coronary artery.
Which of the following statements describes the best management strategy for severe ostial right coronary artery stenosis associated with non-infectious aortitis?
Show Answer