Between a Rock and a Hard Place | Patient Case Quiz
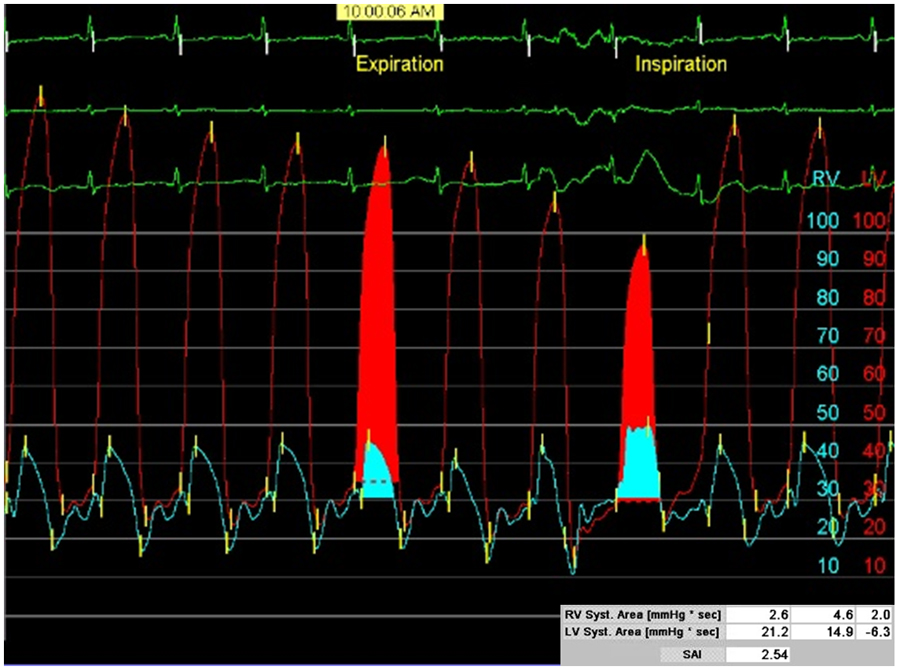
A 70-year-old man presents to your clinic for evaluation of increasing lower extremity edema and diuretic refractory ascites, worsening dyspnea on exertion, and fatigue. His volume status was previously controlled with diuretics, but it is now requiring increasing frequency of large volume paracenteses. He has a history of coronary artery disease status post 4 vessel coronary artery bypass grafting in 1994, chronic kidney disease stage III, hypertension, obesity, and diabetes. His medications include furosemide 40mg daily, aspirin 81mg daily, losartan 50mg daily, and insulin. His blood pressure is 162/72, heart rate is 72 beat per minute, and BMI is 39 kg/m2. His exam is notable for an elevated jugular venous pressure at his earlobe sitting upright with rapid Y descent, pericardial knock without a rub, clear lung sounds bilaterally, ascites (Figure 1), and symmetric 3+ pitting edema to his thighs with chronic venous stasis changes (Figure 2). His electrocardiogram (Figure 3) showed normal sinus rhythm with a heart rate of 72, complete right bundle branch block, left anterior fascicular block, diffuse T wave inversions, and low voltage in his limb leads. His laboratory values are significant for a brain natriuretic peptide 89pg/ml, hemoglobin 9.0 g/dL, sodium 138 mmol/L, potassium 5.4 mmol/L, creatinine 1.69 mg/dL, TSH 4.25 uU/ml, sedimentation rate 59 mm/hr, ultrasensitive C reactive protein of 16.5 mg/L, and hemoglobin A1c of 7.3%. A transthoracic echocardiogram is obtained revealing a left ventricular ejection fraction of 59%, tethering of the left ventricle, septal bounce, pericardial thickening, early diastolic notching on short axis M mode, annulus reversus (septal E` > lateral E` through the mitral annulus), and a plethoric IVC with < 50% collapse during inspiration. Given the concern about pericardial constriction, a constriction study is performed.
The patient was confirmed to have pericardial constriction and underwent a successful pericardiectomy. Additonal images (Figure 4 and 5) show evidence of extensive pericardial calcification on his pre-operative chest CT and gross specimen, respectively. Calcification is also evident on fluroscopy during his pre-operative left heart catheterization and constriction study (Video 1).
Figure 1
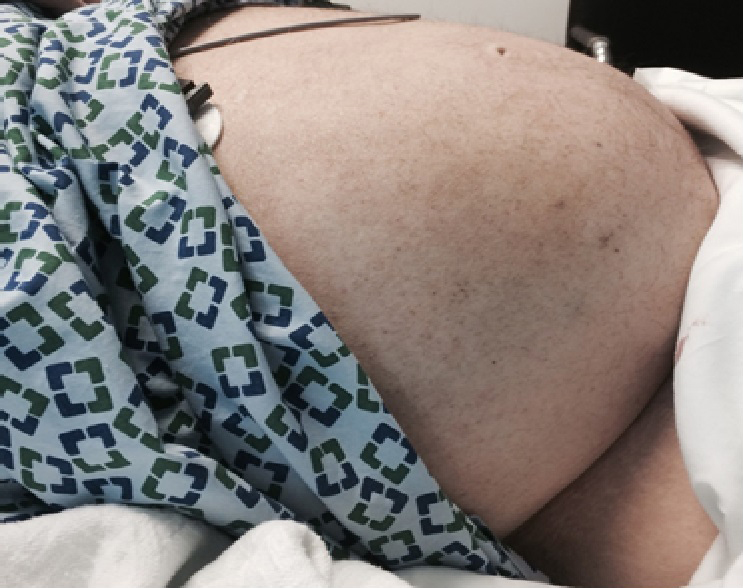
Physical examination showing abdominal distention and ascites.
Figure 2

Physical examination of lower extremities showing pitting edema and chronic venous stasis changes.
Figure 3
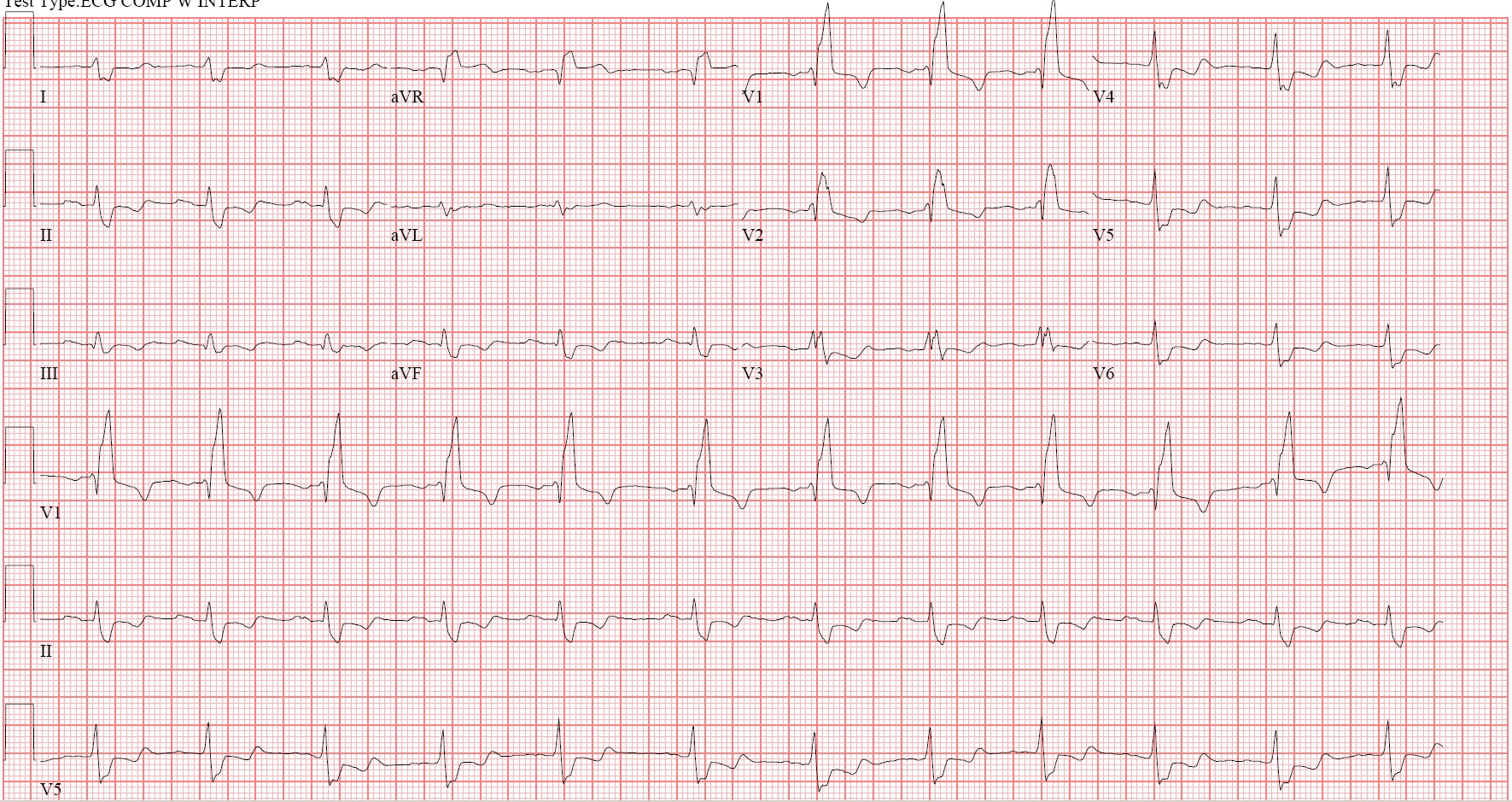
Electrocardiogram
Figure 4

Calcified Pericardial Constriction: Nongated unenhanced cardiac Chest CT - Coronal view showing extensive linear pericardial calcification (white arrows) over the base of the right ventricle and inferio-lateral left ventricle.
Figure 5

Gross specimen of the pericardium status post pericardiectomy showing thickened pericardium with a smooth, glistening parietal surface (A). Conversely, the visceral side (B) appears roughened and fibrous with a moderate amount of calcification. A movat stain (not pictured) was performed showing organized fibrosis with calcification.
Video 1
Fluoroscopy video showing heavy calcification of the inferior and posteriolateral pericardium.
When performing a constriction study to help differentiate between pericardial constriction and restrictive myocardial disease, which finding is associated with the highest specificity for the diagnosis of pericardial constriction?
Show Answer