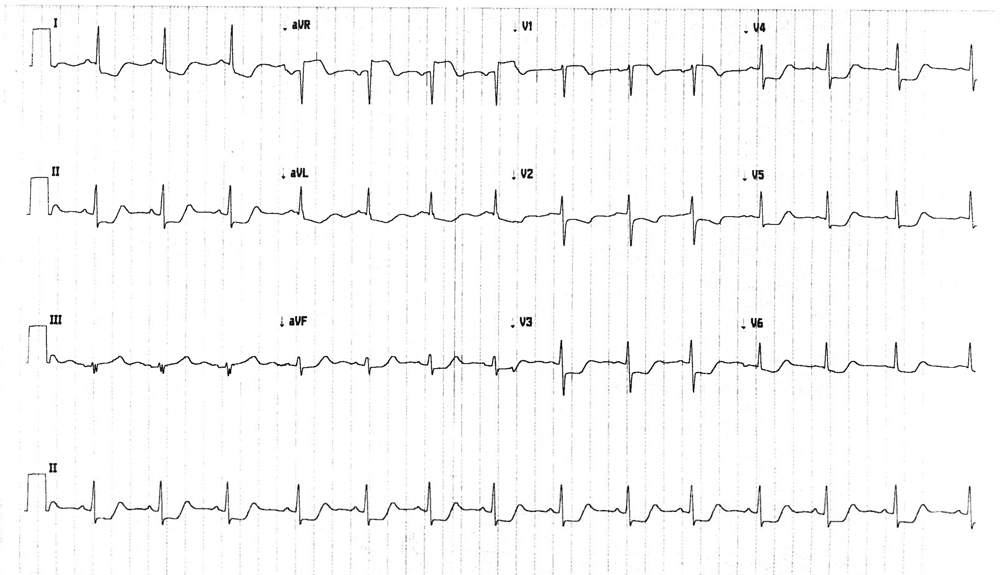
A 26-year-old woman, who is one-month post-partum presents to the Emergency Department (ED) with three days of stuttering chest pain. Her past medical history is notable for Hodgkin's disease treated with mantle field radiation therapy 8 years prior. Her family history is negative for heart disease and sudden cardiac death. A physical exam reveals normal vital signs and an unremarkable cardiopulmonary exam. An ECG obtained at the ED is shown (Figure 1).
Figure 1
The correct answer is: C. She requires urgent coronary angiography given evidence of diffuse subendocardial ischemia.
The patient has diffuse subendocardial ischemia seen on ECG, as identified by the diffuse ST depression. Additionally, there is ST elevation seen in augmented vector right (aVR), and in V1, with a greater degree of ST elevation in aVR compared with V1. These ECG findings are very suggestive of an acute left main coronary artery (LMCA) obstruction.1 In this patient, who is recently post-partum presenting with symptoms and ECG findings suggestive of an acute left main coronary artery obstruction, spontaneous coronary artery dissection (SCAD) must be considered. This patient was diagnosed with SCAD by urgent coronary angiography.
Spontaneous coronary artery dissection (SCAD) is a non-traumatic and non-iatrogenic separation of the endothelium of the coronary artery; specifically, a false lumen is created between either the intima and the media or between the media and the adventitia.2 It is fairly uncommon, but is seen most commonly in women who present with acute coronary syndrome. Risk factors include a predisposing arteriopathy, a post-partum state, and various connective tissue disorders.3 Her prior mantle field radiation therapy also put her at risk. Up to 80% of patients who present with SCAD can present with ST elevation seen on the ECG.4
Management of SCAD is often conservative unless high-risk criteria are present. The high-risk criteria include a left main dissection, sustained ventricular arrhythmias, cardiogenic shock requiring inotropes and/or mechanical support, refractory chest pain or ischemia seen on ECG, or recurrent chest pain requiring serial hospital readmissions.4 For isolated left main dissection, left main percutaneous coronary intervention (PCI) can be performed if it is feasible; if left main PCI is not feasible, the patient should be referred for urgent coronary artery bypass surgery.
Choice A is incorrect as this ECG is inconsistent with acute pericarditis, and there are no physical findings suggestive of acute pericarditis. In acute pericarditis, the classic ECG shows diffuse ST elevation and PR-segment depression.
Choice B is incorrect as her chest pain is certainly related to the ECG findings. While there is ST elevation in V1, its appearance is not consistent with a Brugada pattern, which would be secondary to a congenital sodium channel defect. A type 1 Brugada pattern shows coved ST elevation of at least 2mm in V1 through V3, with a negative T-wave. Her negative family history would also argue against inherited channelopathies, as most are autosomal dominant.
Choice D is incorrect as the ECG findings are not consistent with left ventricular hypertrophy (LVH) with repolarization changes. This ECG shows no clear criteria for LVH, and the T-waves are not inverted, which would be expected in an ECH showing LVH with repolarization changes.
Given the chest pain syndrome and the concerning ECG findings, the patient underwent urgent coronary angiography, which showed severe obstructive disease of the distal left main coronary artery involving the ostium of the left anterior descending, left circumflex, and ramus intermedius arteries. She underwent urgent coronary artery bypass grafting and did well post-operatively. She was discharged seven days after admission.
References
- Yamaji H, Iwasaki K, Kusachi S, et al. Prediction of acute left main coronary artery obstruction by 12-lead electrocardiography. ST segment elevation in lead aVR with less ST segment elevation in lead V(1). J Am Coll Cardiol 2001;38:1348-54.
- Saw J. Spontaneous coronary artery diseection. Can J Cardiol 2013;39:1027-33.
- Yip A, Saw J. Spontaneous coronary artery dissection -- A review. Cardiovasc Diagn Ther 2015;5:37-48.
- Mortensen KH, Thuesen L, Kristensen IB, Christiansen EH. Spontaneous coronary artery dissection: A Western Denmark Heart Registry study. Catheter Cardiovasc Interv 2009;74:710-7.