Myocarditis Mimicking Acute Coronary Syndrome With a Myriad of Arrhythmias
Editor's Note: This case took place at the National Heart Institute of Malaysia. Treatments are based on the resources available to physicians at this facility at the time of the case.
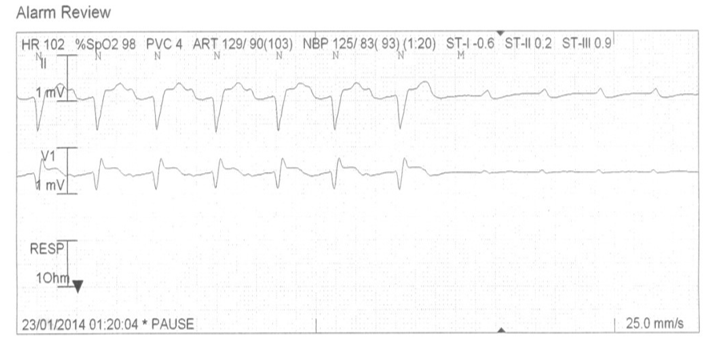
A 28-year-old female patient with no previous history of present illness and two days of fever presented to the emergency department with a syncopal attack. An electrocardiogram (ECG) was taken, which showed left bundle branch block. She was diagnosed to have an acute myocardial infarction. Subsequently, she developed right bundle branch block with left posterior hemiblock. Later, she developed complete heart block with ventricular standstill requiring a temporary pacemaker (Figure 1).
Figure 1
She was referred to the National Heart Institute of Malaysia for further management. She subsequently developed first-degree AV block. Her echocardiogram showed good left ventricular function with an ejection fraction of 55% with no regional wall motion abnormality. Her right ventricular function was depressed (tricuspid annular plane systolic excursion = 1.2). There were no valvular abnormalities and the myocardium appeared normal. Initial laboratory data are included in Table 1. She was planned for an elective coronary angiogram on day two. However on the same day, she developed ventricular fibrillation. She required CPR, intubation, and defibrillation once at 360J. A coronary angiogram revealed normal vessels. She was started on IV lignocaine infusion.
Table 1
|
Troponin T |
|
0.344g/l(0.003-0.100g/l) |
|
LFT |
ALT |
68 U/L (10-32) |
|
CBC |
WBC |
11 X109/L |
|
|
Neutrophil |
74% |
|
|
Lymphocytes |
15% |
|
|
Monocytes |
11% |
|
CRP |
|
18.8 mg/l(<10) |
|
ESR |
|
49 mm/h |
|
CXR |
|
Minimal congestion and upper lobe diversion of pulmonary vessels |
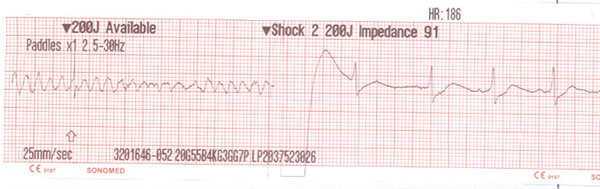
At this point in her treatment, acute viral myocarditis was highly suspected. She was started on IV Methylprednisolone 30mg/kg 6 hourly for 2 days. On day three, she developed pulseless ventricular tachycardia, which required CPR and reverted to sinus rhythm with cardioversion at 200J. She developed another episode of ventricular fibrillation that same day requiring defibrillation at 200J (Figure 2). She was also covered with antibiotic therapy (IV piperacillin/tazobactam 4.5g TDS) as her repeat white cell count was raised. Viral and autoimmune studies were sent (Table 2).
Figure 2
Table 2
|
INVESTIGATIONS |
|
RESULTS |
|
VIRAL STUDIES |
Cytomegalovirus |
Negative |
|
|
Influenza type A |
Negative |
|
|
Influenza type B |
Negative |
|
|
Parainfluenza type 1,2,3 and 4 |
Negative |
|
|
Human enterovirus |
Negative |
|
|
Human rhinovirus |
Negative |
|
|
Human adenovirus |
Negative |
|
|
Human bocavirus |
Negative |
|
|
Human metapneumovirus |
Negative |
|
|
Respiratory syncytial virus, groups A and B |
Negative |
|
|
Coronavirus type (229E, NL63,OC43) |
Negative |
|
|
Herpes virus |
Negative |
|
|
Parvovirus |
Negative |
|
|
Coxsackie A&B |
Negative |
|
|
Dengue serology |
Negative |
|
Autoimmune Studies |
ANA, dsDNA, complement factors (C3,C4) and rheumatoid factor, rheumatoid factor |
Positive for ANA antibodies (SSA pattern) but she was negative for anti dsDNA antibodies |
|
Complement Factor |
C3,C4 |
Normal |
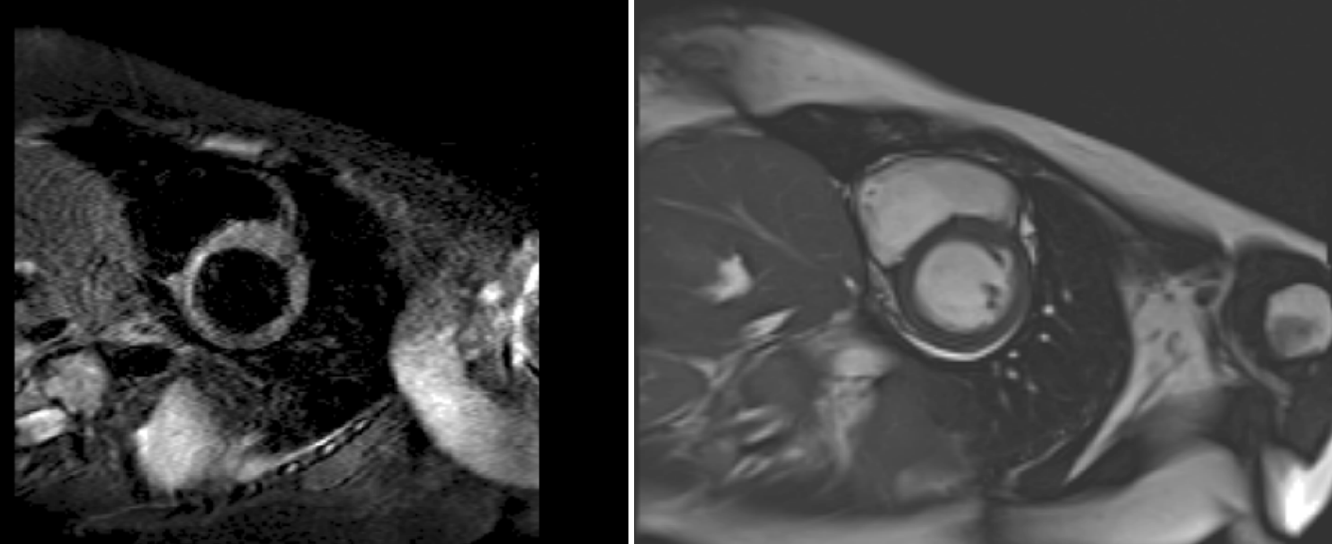
She responded well to pulsed IV methylprednisolone, which was given to her for two days, and then transitioned to oral prednisolone, which was tapered off over two months. Her blood culture was negative for any growth. She subsequently underwent cardiac magnetic resonance imaging (MRI), which showed features suggestive of myocarditis. There was normal indexed left ventricular volumes and systolic function. Right ventricular indexed volumes and function were within normal limits. Short-tau inversion recovery (STIR) positive changes were found in the mid-cavity septal wall suggestive of myocardial inflammation (Figure 3). A follow-up echocardiogram performed after two weeks showed good left ventricular function.
Figure 3
Which of the following statements describes the role for steroid therapy in patients with acute myocarditis?
Show Answer