New Constriction: Transient or Chronic?
A 63-year-old male with no past medical history presents to clinic for a second opinion regarding new shortness of breath and lower extremity edema. The patient was in good health until 9 months ago when he had a viral illness with symptoms of fever, headache, and muscle aches for a week. He had an episode of palpitations that caused him to see a cardiologist. The cardiologist ordered a transthoracic echocardiogram which was notable for a large pericardial effusion. He was started on a 3-month course of ibuprofen 600mg three times a day and colchicine 0.6 mg twice daily. A repeat transthoracic echocardiogram after 3 months showed no residual effusion. Shortly after this repeat echocardiogram, the patient started noticing increased dyspnea on exertion, new lower extremity edema, and new ascites. He was referred to a pulmonologist, nephrologist, and gastroenterologist who found no abnormalities in his lungs, kidneys, or liver respectively.
Prior to this he was able to exercise on a treadmill daily without shortness of breath, but now he has trouble walking 50 feet before stopping to catch his breath. Similarly, his ascites has increased to the extent that requires monthly large volume paracenteses. He receives another repeat transthoracic echocardiogram that shows no pericardial fluid. The patient also receives a chest CT which is notable for thickened pericardium (8mm). The patient comes to clinic for a second opinion regarding his symptoms.
Physical exam: Pleasant middle-aged male in no acute distress. Blood pressure 126/93 mmHg, pulse 89, respirations 20. His jugular venous pressure is 20 cm H20 with positive Kussmaul's sign. His heart is regular without gallop or murmur but notable for a pericardial knock. Lungs are clear without any gallop or murmur. His skin is warm and he has 1+ pitting lower extremity edema bilaterally. Abdominal exam is notable for a large amount of ascites but shows no organomegaly.
Laboratory testing: Thyroid stimulating hormone normal; Sedimentation rate 6 mm/hr; C-reactive protein 10 mg/L; ANA and Rheumatoid Factor were negative. Pro-BNP was 1355 pg/mL. Sodium 136 mmol/L, Potassium 4.0 mmol/L, Chloride 89 mmol/L, Bicarbonate 31 mmol/L, Blood urea nitrogen 41mg/dL, Creatinine 1.59 mg/dL. His liver enzymes and complete blood count are normal.
EKG: Sinus rhythm, 68 beats per minute, evidence of left ventricular hypertrophy is present. QRS duration 80 milliseconds. PR interval is 156 milliseconds. Corrected QT interval is 442 milliseconds. There are no ST changes or abnormalities.
Echocardiogram: Normal left ventricular size with severe septal hypertrophy with normal systolic function. Right ventricle is normal in size with normal systolic function. Estimated right ventricular pressure is 24 mmHg. Left and right atrial cavities are normal in size. There is no major valvular regurgitation or stenosis. There is no evidence of pericardial effusion. Left ventricular outflow gradient at rest is 19 mmHg without change with Valsalva maneuver or amyl nitrate. There is minimal systolic anterior motion of the anterior leaflet of the mitral valve at rest. Features of constriction are present including a subtle septal bounce, pericardial tethering, and a dilated inferior vena cava.
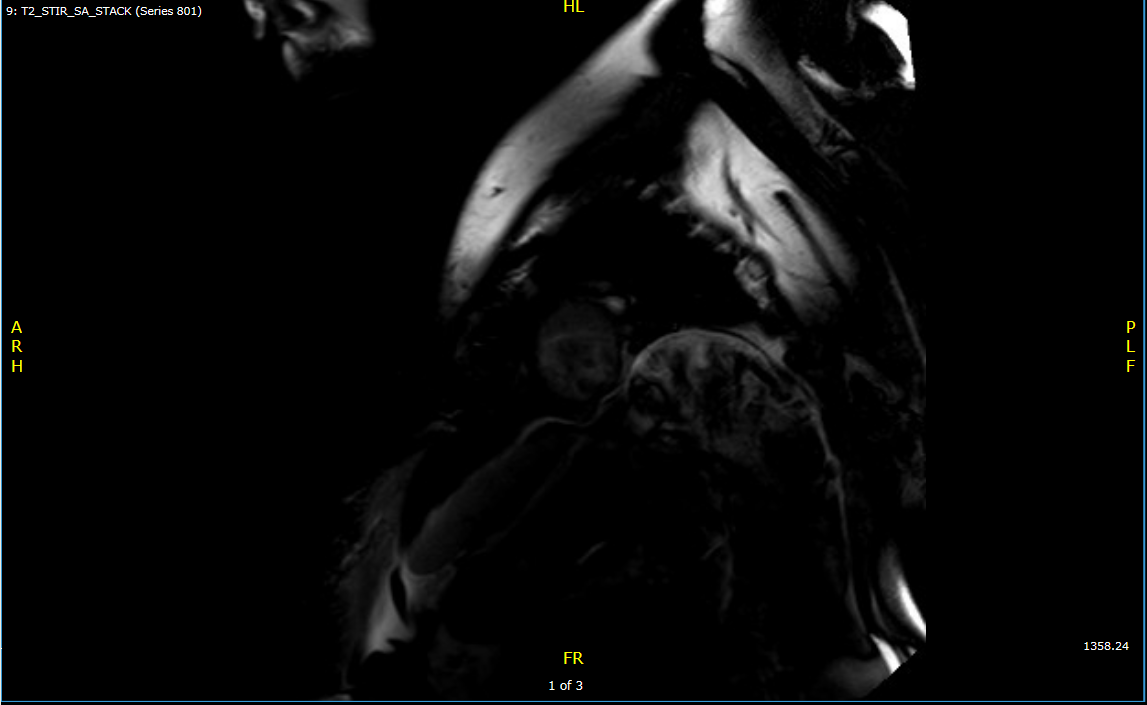
Cardiac MRI: Diffuse circumferential pericardial thickening. No increased pericardial enhancement. No pericardial delayed enhancement. Features of constriction are present with a mild septal bounce, mild conical deformity, diastolic restraint, and dilation of the suprahepatic IVC.
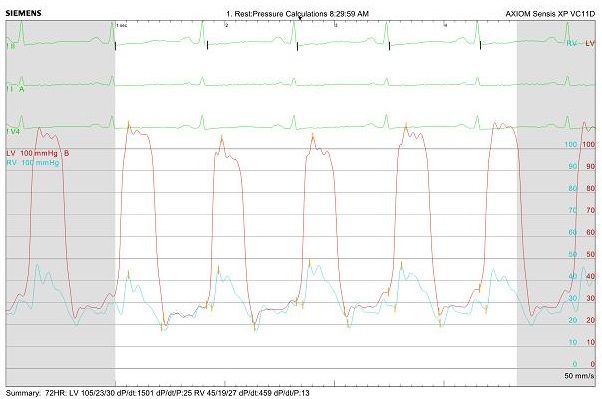
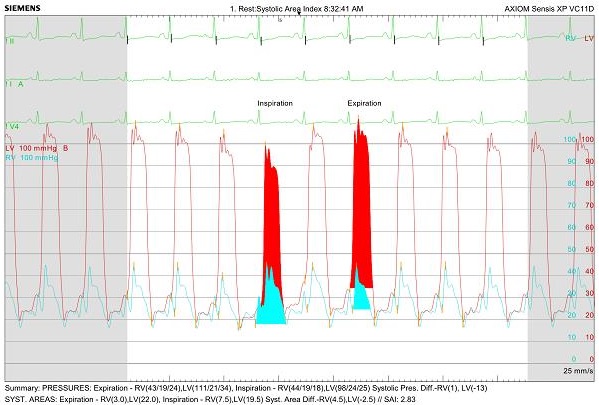
Left and right heart cardiac catheterization: Mean right atrial pressure 23 mmHg, right ventricular pressure 45/24 mmHg, pulmonary artery pressure 40/24 mmHg (mean 30mmHg), pulmonary wedge pressure 24 mmHg, and left ventricular end diastolic pressure 26 mmHg. Equalization of diastolic pressure in right and left ventricle. Right ventricular end diastolic pressure >1/3 right ventricular systolic pressure. No square root sign in right ventricle. No deep Y descent in right atrium. Evidence of ventricular interdependence with systolic area index 2.8 (>1.1 suggests constriction). No evidence of coronary artery disease. Subaortic gradient of 14mmHg.
Video 1: Transthoracic echocardiogram, Parasternal long axis view showing subtle septal bounce and septal hypertrophy
Video 2: Transthoracic echocardiogram, Apical 4 chamber view showing pericardial tethering
Video 3: Transthoracic echocardiogram, Subcostal inferior vena cava view showing dilated inferior vena cava
Figure 1: T2 STIR MRI showing no pericardial edema
Figure 2: PSIR MRI showing no pericardial late gadolinium enhancement (LGE)
Figure 3: Right and left heart catheterization hemodynamics showing equalization of diastolic pressures
Figure 4: Right and left heart catheterization hemodynamics showing evidence of ventricular interdependence and ventricular discordance (during inspiration: the area under the curve between left ventricular systolic and right ventricular systolic pressure tracing decreases)
How would you further manage the patient's constrictive pericarditis?
Show Answer