Risk Stratification of Patients With Refractory Angina | Patient Case Quiz
A 56-year-old man with diabetes, history of tobacco use, coronary artery disease (CAD) treated five years ago with a 2-vessel coronary artery bypass graft surgery and chronic class III angina despite optimal medical therapy presented to the emergency department for evaluation of worsening chest pain. He reported moderate severity, retrosternal chest pressure associated with dyspnea, similar to his prior ischemic pain, but increasing in frequency from a few times every other day to multiple times daily for the past week.
In the emergency room, he was given sublingual nitroglycerin, aspirin and initiated on intravenous unfractionated heparin with complete resolution of his chest pain. The initial electrocardiogram (ECG) revealed normal sinus rhythm with non-specific ST segment changes, unchanged compared with prior ECGs. Initial troponin I was undetectable. Due to concern for unstable angina, he was admitted to the cardiology service for monitoring and serial cardiac biomarker testing.
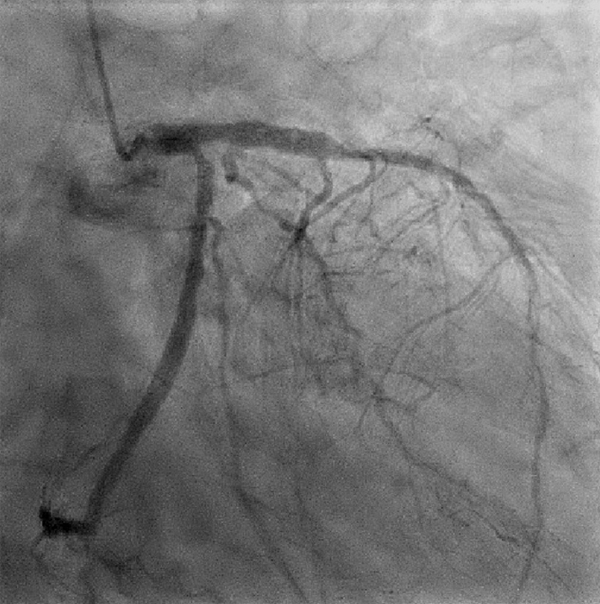
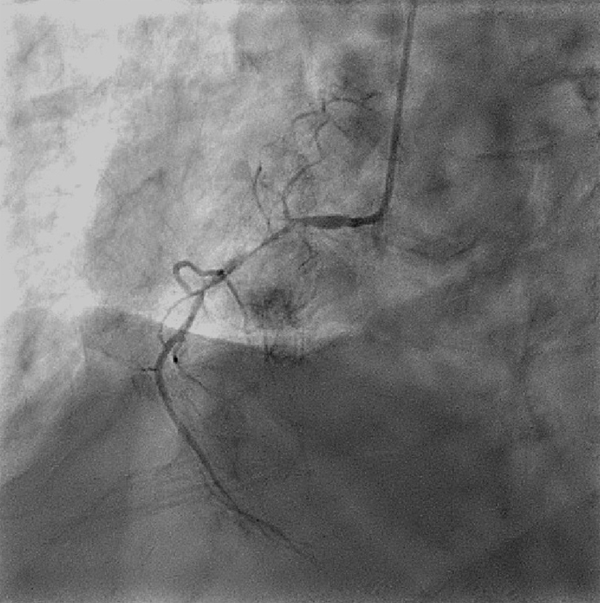
Overnight, he remained chest pain free and serial troponin I levels were undetectable. He was referred for coronary angiography, which revealed a patient left internal mammary artery graft to the left anterior descending artery with diffuse disease distal to the anastomosis, chronically occluded saphenous vein graft to the proximal left circumflex artery with a 60% ostial stenosis and TIMI 3 distal vessel flow and a 95% discrete stenosis of the right coronary artery which was small and non-dominant (figures 1 and 2). The proximal left circumflex artery stenosis was assessed with fractional flow reserve (FFR) and determined to be non-flow limiting (FFR = 0.90). Based on this coronary angiogram, revascularization was deemed to be infeasible due to calcified vessels with poor distal runoff. He was discharged with plans to follow-up with his outpatient cardiologist.
|
Which of the following clinical characteristics is most strongly associated with risk of mortality over the next 3 years?
Show Answer