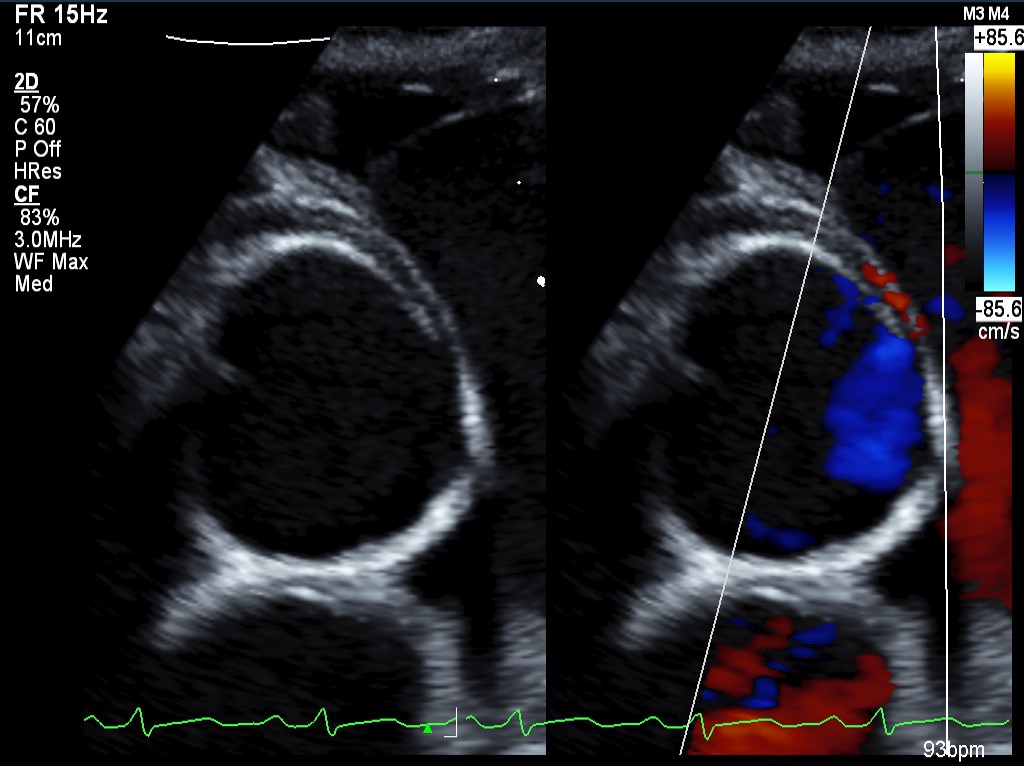
A 14-year-old, previously healthy male suffers a cardiac arrest while playing basketball. A bystander performs cardiopulmonary resuscitation (CPR) on the patient for several minutes before an automated external defibrillator (AED) is applied, and a single shock is delivered. He regains a perfusing rhythm but remains apneic and is intubated by emergency medical service personnel. Upon arrival at an outside hospital, he has a mild respiratory acidosis, is in normal sinus rhythm, and has an elevated troponin level of 3 ng/ml. A head computed tomography (CT) scan demonstrates cerebral edema, and he is managed with mannitol, hypertonic saline, and a brain-cooling protocol. His initial evaluation also includes a transthoracic echocardiogram that reveals a small right coronary artery arising from the left coronary sinus, coursing between the aorta and pulmonary artery, and with an intramural course (Figure 1). Left ventricular function is normal and the right ventricular function is mildly reduced.
Figure 1
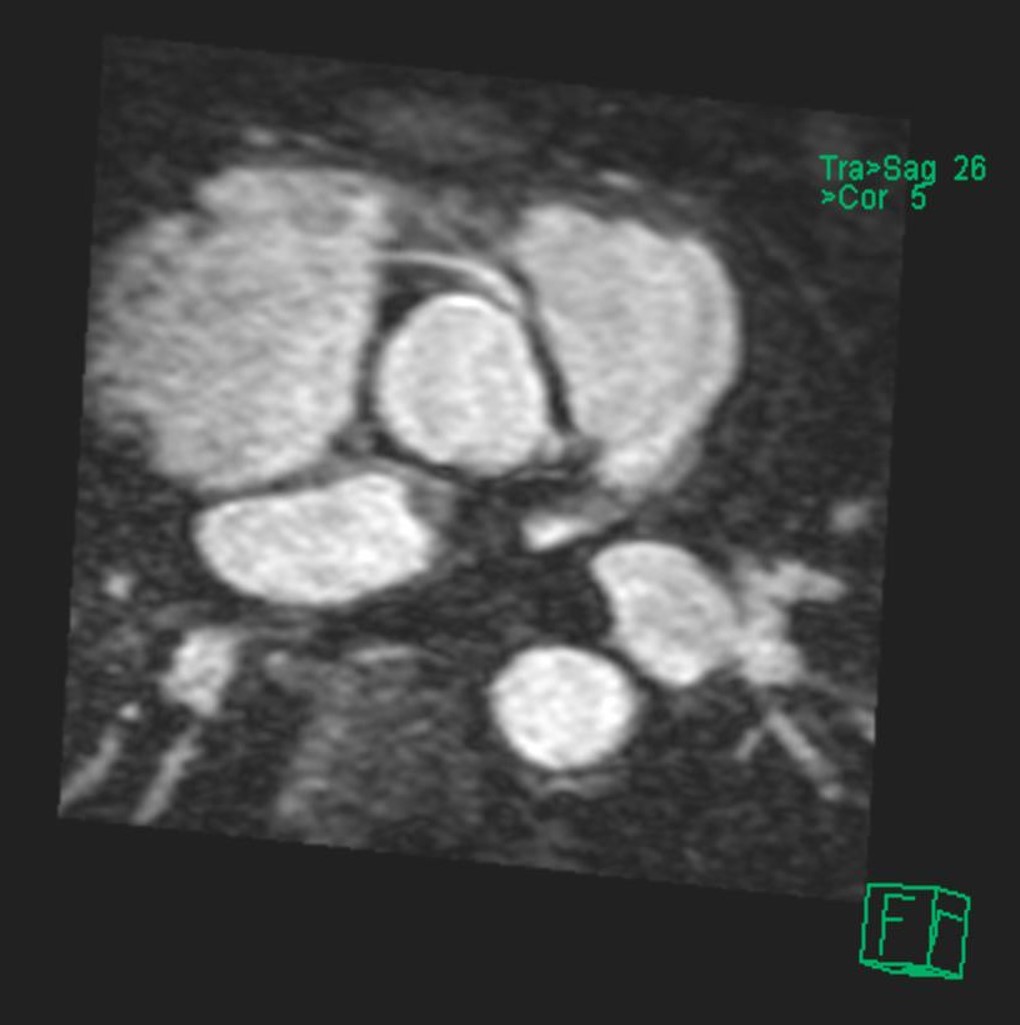
He is transferred to a tertiary care center for further evaluation and management. Four days after his arrest, he is extubated. He continues to exhibit delirium, possibly secondary to anoxic encephalopathy. Cardiac magnetic resonance imaging (MRI) is obtained to further evaluate the anomalous right coronary and confirm the previous diagnosis (Figure 2). In addition, a possible left-sided pulmonary embolism (PE) is seen. A chest CT with PE protocol further delineates the left lower lobar PE with distal filling defects. Anticoagulation with low molecular weight heparin is initiated. His neurologic status includes mild delirium that improves by hospital discharge, as well as subclinical seizures that are managed with levetiracetam. He is discharged to home on enoxaparin, metoprolol, levetiracetam, and exercise restrictions with ongoing occupational therapy for his neurologic injury. Follow-up brain imaging is unremarkable.
Figure 2
The correct answer is: E. Coronary artery unroofing and possible osteoplasty.
The incidence of anomalous aortic origin of a coronary artery (AAOCA) in the general population is estimated to be 0.1-0.9%, though the true incidence remains unknown. This category of lesions includes anomalous origins of the right and left main coronary arteries, usually from the opposite coronary sinus in the aorta or opposite coronary vessel. Of particular concern is the association with an increased risk of sudden cardiac death (SCD) when the anomalous artery takes an interarterial course between the aorta and pulmonary artery and has an intramural course within the wall of the aorta. Historically, a greater risk of SCD has been associated with anomalous aortic origin of the left coronary artery (AAOLCA) than with anomalous aortic origin of the right coronary artery (AAORCA), though SCD has been reported in conjunction with both types of anomalies. Currently, AAOCA is considered to be the second leading cause of SCD in children and adolescents behind hypertrophic cardiomyopathy. The symptoms of AAOCA, while highly variable, may include chest pain, palpitations, and/or dizziness, especially after exertion.
The 2008 ACC/AHA Guidelines for the Management of Adults with Congenital Heart Disease recommend surgical revascularization for AAOLCA with or without evidence of myocardial ischemia and for AAORCA when signs or symptoms of ischemia are present.1 Initial medical management of a patient with AAOCA at increased of SCD or who has suffered such an event may include beta-blockade and exercise restriction to reduce myocardial work and potential ischemia. Although there are no formal guidelines regarding this management, there may be significant inter-intuitional variation. Given that the presented patient suffered an SCD event as a result of the AAORCA, simple medical management and further observation may not be adequate. Therefore, answer option A is incorrect.
Transthoracic echocardiography is highly accurate in determining the course of anomalous coronary arteries and is often employed as an initial imaging modality. Given its accuracy and noninvasive nature, echocardiography has reduced the role of diagnostic catheterization to that of determining whether associated atherosclerotic disease is present in adult patients. Thus, answer option B is incorrect. Similarly, given the low risk of concomitant atherosclerotic coronary artery disease in this patient, catheter-based intervention is unlikely to be needed and answer option C is incorrect. Cardiac MRI and contrast-enhanced CT may provide further definition of the coronary anatomy, and as such have a class I recommendation for inclusion in the initial evaluation process (Level of Evidence: B).1
The diagnostic accuracy of CT and MRI are well-documented.2-3 As MRI can characterize intracardiac and intravascular flow without subjecting the patient to ionizing radiation, it has gained increasing popularity in pediatric cardiology. Conversely, given the greater availability and speed of acquisition as well as the ability to visualize intricate coronary anatomy, cardiac CT is more commonly utilized at our adult center. CT and MRI may also allow clarification of ostial anatomy specifically in cases of AAOLCA.4
The options for surgical repair for AAOCA include coronary unroofing, coronary translocation, pulmonary artery translocation, osteoplasty, and coronary artery bypass grafting.5 Coronary artery bypass grafting as a stand-alone revascularization option may carry a high rate of symptom recurrence and should be reserved for cases involving associated atherosclerotic disease or concern for proximal arterial stenosis. As there is little concern for these in this case, answer option D is incorrect. Interarterial, intramural lesions are often repaired using coronary unroofing techniques, whereas non-intramural lesions may be managed with coronary transfer or translocation.6 These procedures have been shown to be associated with low morbidity and mortality in the short- and long-term periods.6,7 Answer option E, then, is the correct answer.
As revealed by a recent survey of Congenital Heart Surgeons' Society (CHSS) members, significant variability exists among providers and institutions regarding the optimal management of patients with AAOCA, including the indications and timing for surgical intervention. Recently, the CHSS formed the AAOCA Working Group to prospectively collect data for patients who have undergone AAOCA repair across multiple institutions in order to guide the determination of optimal management strategies for the variety of lesions AAOCA encompasses.8
Following a period of anticoagulation for PE, the patient undergoes interval repair of the AAOCA. Intraoperatively, the RCA is seen arising not from the right coronary sinus but from the left sinus. The aorta is incised near the level of the sinotubular junction, and a slit-like orifice of the RCA is seen adjacent to the orifice of the left main coronary artery. The intramural course of the RCA is opened widely along the aortic wall, and the edges are tacked in place with interrupted sutures. Separation from bypass is uneventful, and an intraoperative transesophageal echocardiogram demonstrates normal biventricular function and adequate flow in the unroofed vessel. He is extubated in the operating room prior to transfer to the intensive care unit. He does well postoperatively and is discharged to home on the fifth postoperative day on warfarin. He is able to return to school following recovery from surgery. Four months after surgery, he undergoes a stress echocardiogram, which shows no evidence of ischemia and unchanged biventricular function, and he is released to resume athletic activities.
References
- Warnes CA, Williams RG, Bashore TM, et al. ACC/AHA 2008 guidelines for the management of adults with congenital heart disease. J Am Coll Cardiol 2008;52:143-263.
- Turner II, Turek JW, Jaggers J, Herlong JR, Lawson DS, Lodge AJ. Anomalous aortic origin of a coronary artery: preoperative diagnosis and surgical planning. World J Pediatr Congenit Heart Surg 2011;2:340-5.
- Tangcharoen T, Bell A, Hedge S, et al. Detection of coronary artery anomalies in infants and young children with congenital heart disease by using MR imaging. Radiology 2011;259:240-7.
- Brothers JA, Whitehead KK, Keller MS, et al. Cardiac MRI and CT: differentiation of normal ostium and intraseptal course from slitlike ostium and interarterial course in anomalous left coronary artery in children. AJR Am J Roentgenol 2015;204:104-9.
- Mery CM, Lawrence SM, Krishnamurthy R, et al. Anomalous aortic origin of a coronary artery: toward a standardized approach. Semin Thoracic Surg 2014;26:110-22.
- Mainwaring RD, Reddy VM, Reinhartz O, Petrossian E, Punn R, Hanley FL. Surgical repair of anomalous aortic origin of a coronary artery. Euro J Thorac Cardiovasc Surg 2014;46:20-6.
- Krasuski RA, Magyar D, Hart S, et al. Long-term outcome and impact of surgery on adults with coronary arteries originating from the opposite coronary cusp. Circulation 2011;123:154-62.
- Poynter JA, Bondarenko I, Austin EH, et al. Repair of anomalous aortic origin of a coronary artery in 113 patients: a Congenital Heart Surgeons' Society Report. World J Pediatr Congenit Heart Surg 2014;5:507-14.