When Things Go "POP"
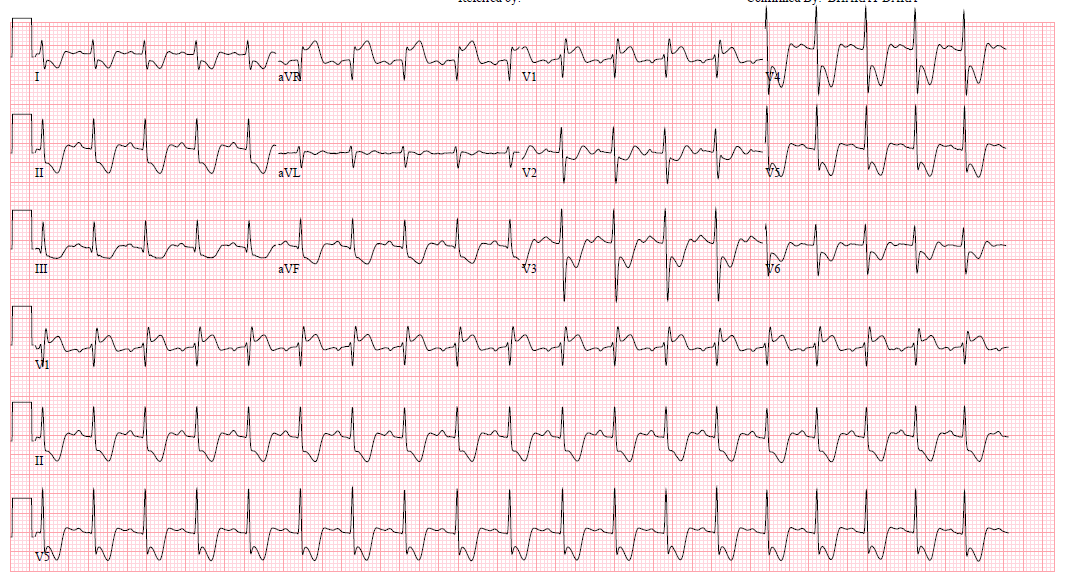
A 13-year-old Hispanic male presents to the emergency department (ED) with complaint of epigastric pain and a "fainting spell." He spent the day hiking with his family in the desert in June without drinking much water. Upon arriving home, he complained of epigastric pain and nausea. He went to lie down and his sister reports that he "threw up and then fainted." EMS was called and he was brought to the ED. He is noted to be hypotensive (85/42 mm Hg) on arrival and is given two liters of intravenous fluid. His heart rate was 115 bpm. He is awake and alert and has three further episodes of emesis. His parents report a febrile illness a week prior with a negative rapid strep screen. He has otherwise been healthy. He is adopted and no family history is known. An electrocardiogram (ECG) is obtained (Figure 1) and the on-call pediatric cardiologist is called for consultation.
Figure 1: ECG
The cardiologist's examination reveals a very ill appearing young man. The HR is 140 with a noninvasive blood pressure of 83/28 mm Hg. The respiratory rate is 32 breaths per minute, and there is a hyperactive precordium. On auscultation, a soft low-pitched diastolic murmur is heard at the right lower sternal border. Troponins are pending.
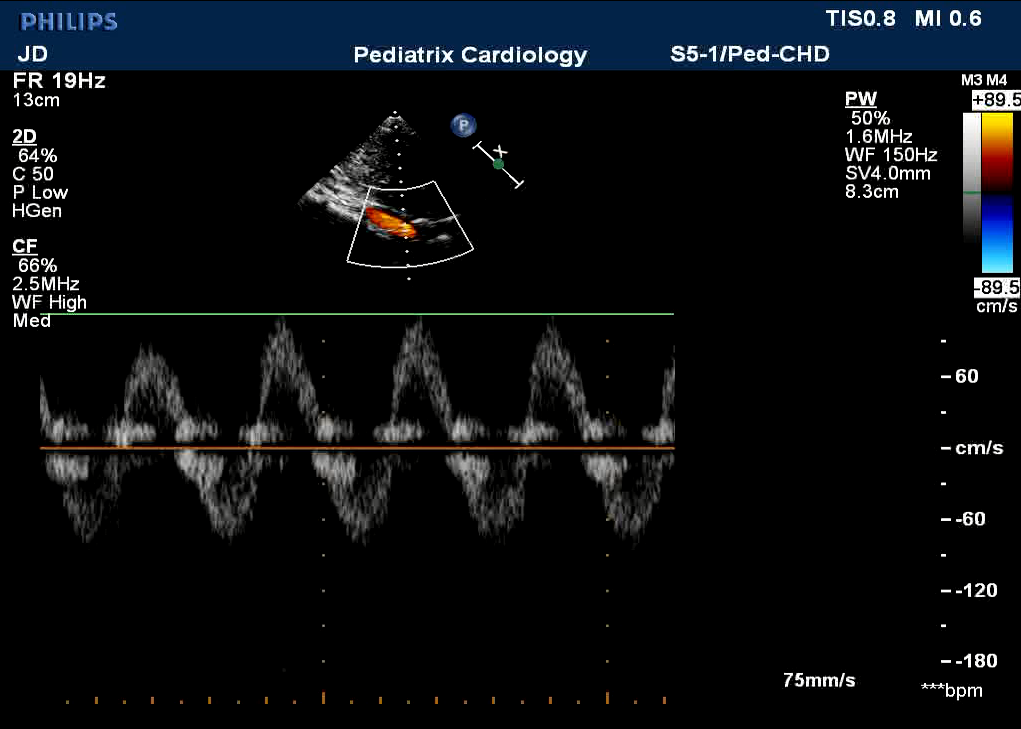
An echocardiogram is done with the patient sitting up in bed due to ongoing emesis (Figure 2, Video 1). There are no evident vegetations or valvar pathology (regurgitation or stenosis).
Video 1: Original Aortic View
Figure 2: Abd Ao Doppler
The patient becomes more hypotensive and unresponsive. He is intubated and a norepinephrine drip is started. He is transferred to the pediatric intensive care unit. Dopamine is added shortly thereafter.
Further echo imaging is obtained with the patient sedated and muscle-relaxed after intubation. As the consultant cardiologist, which of the following is the best next step?
Show Answer