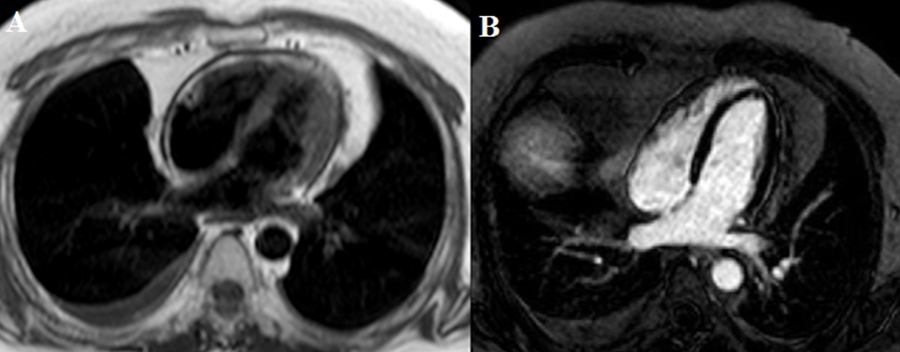
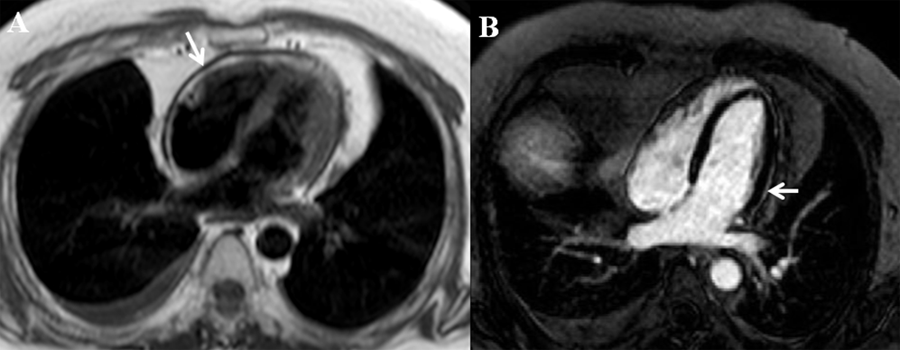
A 45-year-old male reformed smoker with a history of recurrent pericarditis presented with four months of worsening dyspnea, fatigue and peripheral edema. Eight months earlier he had presented with fevers, cough, and orthopnea and at that time was diagnosed with idiopathic acute pericarditis and initiated on triple therapy with ibuprofen 600 mg three times a day, colchicine 0.6 mg twice daily and a course of prednisone 40 mg taper. Since then he has had three episodes of recurrent pericarditis. He denied any history of malignancy, chest radiation or tuberculosis. He reported 30 pound weight gain, orthopnea, dyspnea, and peripheral edema. On physical exam, blood pressure was 120/88 mmHg, heart rate 72 beats per minute, temperature 98.6°C, respiratory rate of 22 per minute, oxygen saturation of 98% on room air. Exam was notable for increased jugular venous distension >20 cm, bibasilar decreased breath sounds, moderate pitting lower extremity edema to knees. Complete metabolic panel and complete blood count were normal. C-reactive protein and erythrocyte sedimentation rate were normal at 2.6 mg/dl and 1 mm/hour. Troponin T was <0.01 ng/mL and B-type natriuretic peptide 69 pg/mL. Rheumatoid factor, antinuclear antibody, and thyroid stimulating hormone levels were unremarkable. Electrocardiogram showed normal sinus rhythm with no ST or PR segment changes. Transthoracic echocardiogram revealed normal EF of 55%, and findings consistent with constrictive pericarditis with pericardial thickening, septal bounce, ventricular tethering with diastolic restraint, and inferior vena cava plethora. Cardiac magnetic resonance imaging (CMR) was performed and shown below (Figures A and B). The patient was diagnosed with transient constrictive pericarditis and treated with combined triple anti-inflammatory therapy with nonsteroidal anti-inflammatory drug, colchicine and steroids, with improvement in symptoms. Three months later, he presented again with dyspnea and fatigue. Cardiopulmonary exercise testing (CPX) was performed and showed normal ST segment response to stress, 110% maximal predicted heart rate, fair functional capacity for age with 5.3 metabolic equivalents, maximal oxygen uptake (peak VO2) of 18.4 ml/kg/min with adequate respiratory effort (respiratory exchange ratio) of 1.27 corresponding to low peak aerobic capacity (predicted peak VO2 %) of 44%, and low ventilatory efficiency or minute ventilation/carbon dioxide production slope (VE/VCO2) of 41. These findings suggest overall poor functional capacity.
The correct answer is: B. Refer for pericardiectomy
In our patient, idiopathic transient constrictive pericarditis (CP) was diagnosed. Due to persistent symptoms on medical therapy and poor performance on CPX, the patient underwent pericardiectomy with improved symptoms. On CMR, axial black blood image showed up to 5 mm circumferential pericardial thickening (Figure A arrow) and delayed enhancement imaging with phase sensitive inversion recovery showed very mild lateral pericardial gadolinium enhancement (Figure B arrow), suggestive of minimal residual inflammation. Pericardial inflammation and edema can lead to pericardial thickening resulting in poor compliance of the pericardium and eventually constrictive physiology. With conventional medical therapy – the use of triple anti-inflammatory therapy with nonsteroidal anti-inflammatory drug, colchicine and steroids – delayed enhancement and constrictive physiology can be reversed.1,2 Transient CP was first described in 1987 by Sagristà-Sauleda et al where 9% of patients identified with effusive acute idiopathic CP had reversible constriction after a mean period of 2.7 months.3 Immuno-modulating agents, such as azathioprine and the interleukin-1 receptor antagonist (anakinra), can be considered in refractory recurrent cases or when use of steroid sparing agents is preferred. However, use of these agents in CP are not standardized and further prospective randomized trials are needed.4-6 In our patient, there is only minimal residual inflammation on CMR and he had failed multiple trials of conventional medical therapy, therefore early referral for pericardiectomy should be considered.
Figure Legends
Figure A: Cardiac magnetic resonance imaging in the setting of constrictive pericarditis showing pericardial thickening (arrow) on axial black blood image.
Figure B: Mild pericardial enhancement (arrow) suggesting residual pericardial inflammation is seen on delayed enhancement imaging with phase sensitive inversion recovery on cardiac magnetic resonance imaging.
References
- Feng D, Glockner J, Kim K et al. Cardiac magnetic resonance imaging pericardial late gadolinium enhancement and elevated inflammatory markers can predict the reversibility of constrictive pericarditis after antiinflammatory medical therapy: a pilot study. Circulation. 2011;124:1830-7.
- Haley JH, Tajik AJ, Danielson GK, Schaff HV, Mulvagh SL, Oh JK. Transient constrictive pericarditis: causes and natural history. J Am Coll Cardiol. 2004;43:271-5
- Sagrista-Sauleda J, Permanyer-Miralda G, Candell-Riera J, Angel J, Soler-Soler J. Transient cardiac constriction: an unrecognized pattern of evolution in effusive acute idiopathic pericarditis. Am J Cardiol. 1987;59:961-6.
- Imazio M, Lazaros G, Brucato A, Gaita F. Recurrent pericarditis: new and emerging therapeutic options. Nat Rev Cardiol. 2015 Aug 11.
- Jain S, Thongprayoon C, Espinosa RE et al. Effectiveness and Safety of Anakinra for Management of Refractory Pericarditis. Am J Cardiol. 2015 Oct 15; 116(8):1277-9.
- Lazaros, G. et al. Anakinra: an emerging option for refractory idiopathic recurrent pericarditis. A systematic review of published evidence. J. Cardiovasc. Med. (Hagerstown)
- Milani RV, Lavie CJ, Mehra MR. Cardiopulmonary exercise testing: how do we differentiate the cause of dyspnea? Circulation. 2004 Jul 27;110(4):e27-31.
- Iorio A, Magrì D, Paolillo S, Salvioni E, Di Lenarda A, Sinagra G, Agostoni P, Sciomer S. Rationale for cardiopulmonary exercise test in the assessment of surgical risk. J Cardiovasc Med (Hagerstown). 2013 Apr;14(4):254-61.
- Balady GJ, Arena R, Sietsema K, Myers J, Coke L, Fletcher GF, Forman D, Franklin B, Guazzi M, Gulati M, Keteyian SJ, Lavie CJ, Macko R, Mancini D, Milani RV; American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee of the Council on Clinical Cardiology; Council on Epidemiology and Prevention; Council on Peripheral Vascular Disease; Interdisciplinary Council on Quality of Care and Outcomes Research. Clinician's Guide to cardiopulmonary exercise testing in adults: a scientific statement from the American Heart Association. Circulation. 2010 Jul 13;122(2):191-225.
- Guazzi M, Adams V, Conraads V, Halle M, Mezzani A, Vanhees L, Arena R, Fletcher GF, Forman DE, Kitzman DW, Lavie CJ, Myers J; European Association for Cardiovascular Prevention & Rehabilitation; American Heart Association. EACPR/AHA Scientific Statement. Clinical recommendations for cardiopulmonary exercise testing data assessment in specific patient populations. Circulation. 2012 Oct 30;126(18):2261-74.
- Mehra MR, Kobashigawa J, Starling R, Russell S, Uber PA, Parameshwar J, Mohacsi P, Augustine S, Aaronson K, Barr M. Listing criteria for heart transplantation: International Society for Heart and Lung Transplantation guidelines for the care of cardiac transplant candidates--2006. J Heart Lung Transplant. 2006 Sep;25(9):1024-42.
- Mancini DM, Eisen H, Kussmaul W, Mull R, Edmunds LH Jr, Wilson JR. Value of peak exercise oxygen consumption for optimal timing of cardiac transplantation in ambulatory patients with heart failure. Circulation. 1991 Mar;83(3):778-86.
- Arena R, Myers J, Aslam SS, Varughese EB, Peberdy MA. Peak VO2 and VE/VCO2 slope in patients with heart failure: a prognostic comparison. Am Heart J. 2004 Feb;147(2):354-60.
- Arena R, Myers J, Abella J, Pinkstaff S, Brubaker P, Moore B, Kitzman D, Peberdy MA, Bensimhon D, Chase P, Forman D, West E, Guazzi M. Determining the preferred percent-predicted equation for peak oxygen consumption in patients with heart failure. Circ Heart Fail. 2009 Mar;2(2):113-20
- Arena R, Myers J, Guazzi M. The clinical and research applications of aerobic capacity and ventilatory efficiency in heart failure: an evidence-based review. Heart Fail Rev. 2008 Jun;13(2):245-69.