A 20-year-old runner was seen in the general cardiology clinic for episodic palpitations and dyspnea on exertion of two-month duration. The episodes of palpitations would last for "a couple of minutes" and were associated with a recent decline in functional capacity for the last month. She denied any exertional chest pain, dizziness, or syncope. Physical examination was grossly normal. Resting 12-lead electrocardiogram is shown in Figure 1. Subsequent to the initial evaluation, an event monitor and echocardiogram were performed. The event monitor (Figure 2) demonstrated an episode of wide complex tachycardia at 185 beat per minute, which correlated with symptoms. Complete 2-D echocardiogram revealed global left ventricular hypokinesis with an ejection fraction of 35-40% and subsequent cardiac magnetic resonance confirmed the presence of mild to moderate left ventricular dilatation with mild global hypokinesis and estimated ejection fraction of 45%. There was no evidence of fibrosis or inflammation. During the initial clinical evaluation, the patient reported a family history of cardiomyopathy in two generations; however, follow-up genetic testing in the patient was unrevealing. No further functional exercise stress testing or stress echocardiogram was performed prior to the referral to electrophysiology for further evaluation of the recorded wide complex QRS tachycardia. After our initial evaluation, the patient proceeded with an electrophysiology study. Decremental atrial pacing resulted in transition from narrow QRS to wide QRS with left bundle branch morphology (Figures 3-5). Programmed ventricular stimulation induced tachycardia with typical left bundle branch block (LBBB) morphology.
Figure 1: Baseline electrocardiogram
Figure 2: Event monitor recording
Figure 3: Baseline AH and HV intervals
Figure 4: Rapid atrial pacing demonstrating prolongation of AH interval, and antegrade His activation
Figure 5
Rapid atrial pacing demonstrating change in QRS complex to typical left bundle branch block and retrograde activation of right bundle branch and prolonged AH interval. With progressively shorter atrial pacing cycle length, His bundle potential activated retrogradely (inscribed in QRS), as wavefront travels down the bypass tract and retrograde up the right bundle to His bundle.
The correct answer is: C. Pre-excited tachycardia.
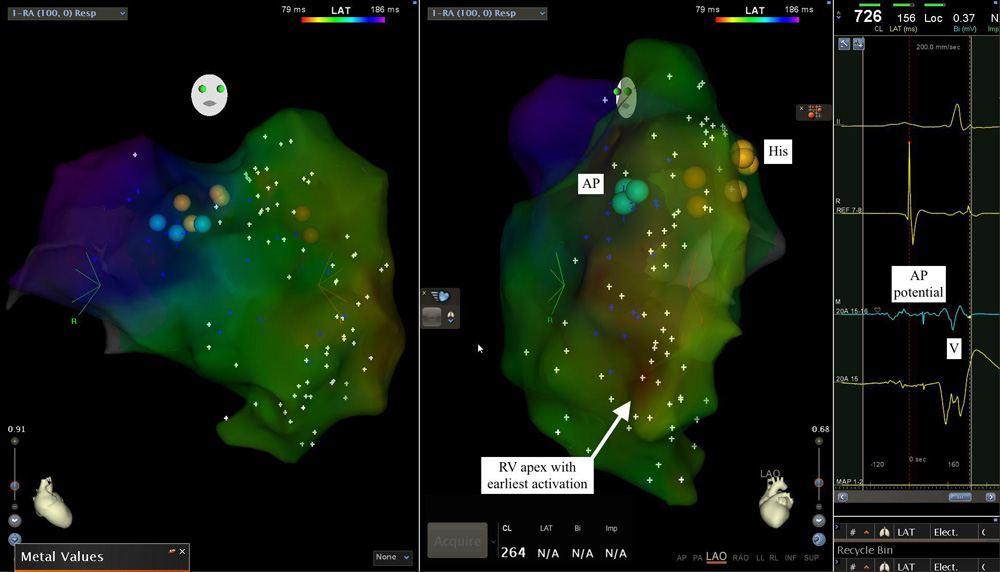
Figure 3 demonstrates baseline AH and HV intervals. During decremental atrial pacing there was a gradual increase in the AV interval and development of typical LBBB (Figures 4 and 5). This was accompanied by a gradual decrease in the HV interval (finally becoming negative) and change in RBB activation from anterograde to retrograde direction (Figures 5 and 6). This finding is consistent with a decrementally conducting right-sided accessory pathway. Further mapping demonstrated that the pathway inserted near the right ventricular apex. A sharp accessory pathway potential was recorded at the tricuspid annulus at 9 o'clock position (LAO view) (Figure 7). The tachycardia was demonstrated to be an antidromic atrioventricular tachycardia using an atriofasicular pathway in the antegrade direction and the AV node in the retrograde direction. Given her clinically symptomatic tachycardia, the atriofasicular pathway was targeted at the accessory pathway potential site on tricuspid annulus and was successfully ablated using radiofrequency energy.1,2 The patient was later seen in our cardiology office post catheter ablation and underwent repeat 2-D echocardiogram that demonstrated unchanged global left ventricular hypokinesis with an ejection fraction of 40-45%. It was thus our opinion that her presentation was most consistent with an idiopathic dilated cardiomyopathy and she was started on goal directed medical therapy.
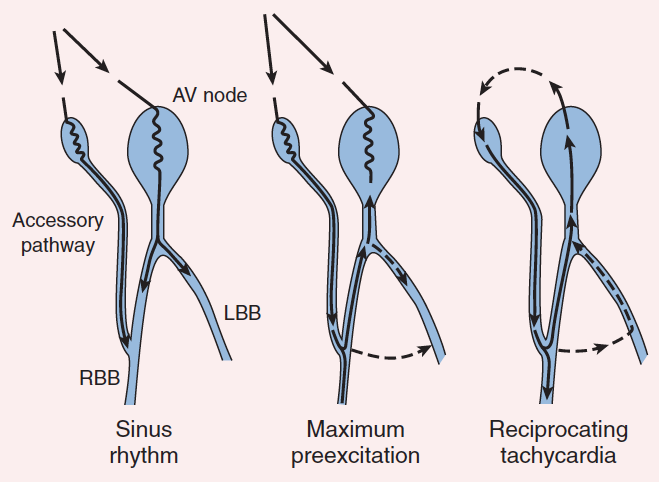
Figure 6
A cartoon of atriofasicular accessory pathway. Sinus rhythm results in a fusion QRS complex, as in the usual common form of accessory pathway. Maximum preexcitation results in ventricular activation over the accessory pathway, and retrograde activation of the His bundle. During the tachycardia, anterograde conduction occurs over the accessory pathway, with retrograde conduction over the normal pathway. LBB = left bundle branch; RBB = right bundle branch
Figure 7
Mapping demonstrates a sharp accessory pathway potential recorded at the tricuspid annulus at 9'0 clock position (LAO view) with earliest activation in right ventricular apex suggestive of pathway insertion near the right ventricular apex
References
- Miller J, Olgin JE. Catheter ablation of free-wall accessory pathways and "Mahaim" fibers. In: Zipes DP, Haissaguerre M, eds. Catheter Ablation of Arrhythmias. Armonk: Futura; 2002:277-303.
- Page RL, Joglar JA, Caldwell MA, et al. 2015 ACC/AHA/HRS guideline for the management of adult patients with supraventricular tachycardia: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 2016;67:1575-623.