Cover Story | Cardiovascular Practices Today: Navigating the Business of Cardiovascular Medicine
No matter what size or type, running a practice hasn’t gotten any easier. Balancing the needs of patients with workforce well-being, while also navigating changing federal and state regulatory requirements and addressing demands from payers, practice partners and/or hospital or health system executives, keeps many a cardiovascular professional up at night.
Practice Integration: The New Normal
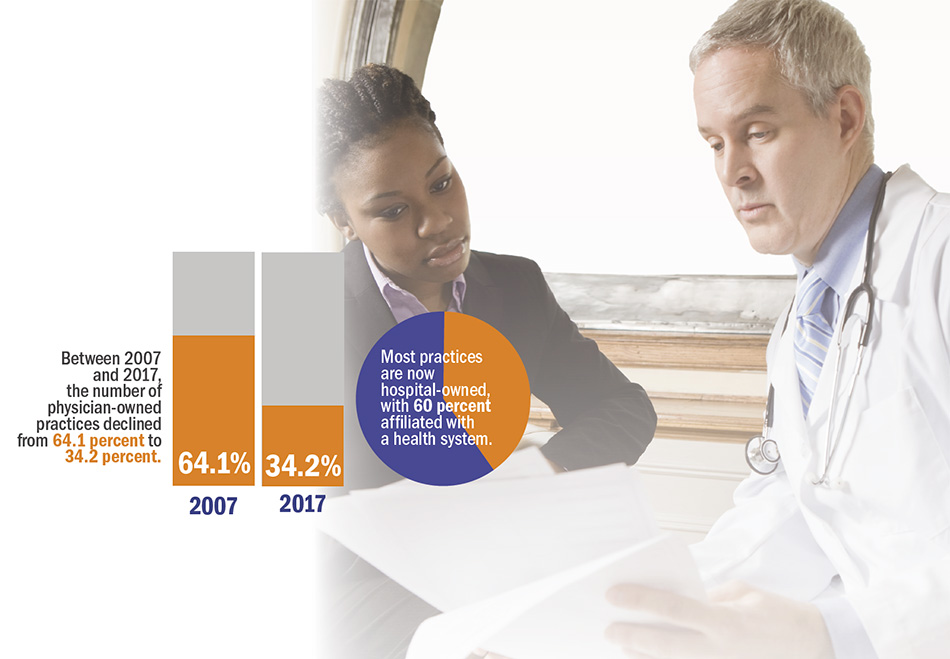
Practice integration has been one of the biggest stories over the last decade. Except for states like California, Arizona and Connecticut, integrated hospital- or health–system-owned practices have now become the norm. ACC’s latest survey of cardiovascular practices shows that between 2007 and 2017, the number of physician-owned practices declined from 64.1 percent to 34.2 percent.
Most practices are now hospital-owned, with 60 percent affiliated with a health system. This mass migration to integration has forced practices and providers to make significant shifts in operations and management structure. Understanding the “business of medicine” — contract negotiations, building an effective cardiovascular service line, dyad management, etc. — has become as essential as understanding the latest clinical research developments.
"Now, our practice has grown to include several hundred multi-specialty providers, meaning more people are involved in decision making, and implementing changes that meet the needs of a diverse group of specialties is much slower." — C. Michael Valentine, MD, FACC
Contract negotiations, or more aptly renegotiations, have been one of the larger hurdles for integrated practices. Of the 355 practices that noted a merger or integration as part of the ACC’s survey, 157 have already had to renegotiate their initial agreement. Of these, 67 percent say the newest contract is about the same or better, while roughly 25 percent say their new contract is worse. With a significant number of practices expected to go through the process in the next few years, there are opportunities to learn from those that have gone ahead to ensure the best possible contract.
Meanwhile, it’s not just contract renegotiations affecting integrated practice operations. ACC Vice President C. Michael Valentine, MD, FACC, says that many practices, including his own in Lynchburg, VA, that were front-runners in the move to integration have grown to include multiple specialties over the years. He notes it was much easier to make rapid change and have direct communication with C-Suite leaders when his integrated practice was smaller. “Now, our practice has grown to include several hundred multi-specialty providers, meaning more people are involved in decision making, and implementing changes that meet the needs of a diverse group of specialties is much slower,” he says.
Reimbursement: The New Seismic Shift
While the shift to hospital- or health system-owned (or at least tightly affiliated) practices has been the biggest story over the last 10 years, more recent changes related to reimbursement, with an emphasis on quality over quantity and population health is the new seismic shift underway, says Pamela S. Douglas, MD, MACC, from Duke University School of Medicine and co-director of ACC’s annual Cardiovascular Summit.
The Medicare and CHIP Reauthorization Act (MACRA) passed in 2015 ushered in the new Quality Payment Program (QPP) and further cemented efforts to transition the U.S. health care system away from a fee-for-service model to one that is focused on improved outcomes and lower costs. While long-term details of the QPP continue to roll out, the first year of the program is underway and practices not participating at this point will face a negative payment adjustment in 2019. (Oct. 2 was the last day for groups and individual clinicians seeking to report a minimum of one continuous 90-day period for 2017 to begin participating in any Merit-Based Incentive Payment System [MIPS] category.)
"What keeps me up at night is designing our strategic plan to be flexible enough to meet these changing requirements coming out of Washington. All practices need to be thinking about this." — Cathleen Biga, RN, MSN
Cathleen Biga, RN, MSN, with Cardiovascular Management of Illinois and co-director of the Cardiovascular Summit, says all practices (integrated and physician-owned) need to understand the QPP and develop strategic plans to guide them going forward. The ACC’s practice survey suggests there is room for improvement in this area. While more than half of practices surveyed report a QPP implementation plan at their practice, nearly 18 percent still do not have a plan and 27 percent are unsure.
“This is coming full steam,” Biga cautions. “What keeps me up at night is designing our strategic plan to be flexible enough to meet these changing requirements coming out of Washington. All practices need to be thinking about this.”
Specifically, Biga suggests that all practices and providers should be reviewing and understanding Quality and Resource Use Reports (QRURs), released to every group practice and solo practitioner based on their TIN, or Taxpayer Identification Number. The QRURs show how clinicians and groups perform on Quality and Cost measures and are critical for understanding quality and cost performance, she says.
Practices should also have a solid understanding of the cardiac measures within the QPP, as well as taking advantage (if appropriate) of voluntary payment bundle programs. While mandatory bundles may be on the back-burner for now, this is an issue that isn’t going way, Biga says. For the roughly 40 percent of practices that are not integrated, she recommends looking at virtual groups as a means of easing MIPs burden and/or exploring whether joining an accountable care organization could provide cost savings. Virtual groups would allow individual eligible clinicians or solo practitioners and small group practices to come together and report on MIPS reporting requirements as a collective entity.
The ACC’s QPP/MACRA hub on ACC.org is a good way to keep up to date on key dates, understand the latest cardiac measures, and find step-by-step instructions for participating in MIPS or Advanced Alternative Payment Models (APMS). Both Biga and Valentine say the Cardiovascular Summit taking place in February in Las Vegas (see sidebar) will also have sessions dedicated to understanding QPP basics. Additionally, ACC’s suite of NCDR registries are providing practices — both integrated and physician-owned — with opportunities to help meet QPP requirements. These options will only continue to grow in the coming years.

Practice Survival Tips
How do practices and providers balance the realities of the current health care environment with patient needs? Some of the most successful practices are those that find novel ways to ensure patient satisfaction, make the most of team-based care to manage and improve population health, and address workforce or provider well-being, says Andrew Freeman, MD, FACC, of National Jewish Health and a member of the Cardiovascular Summit Planning Committee.
“In the past, the physician was responsible for managing a patient’s care and patient input mattered much less,” Freeman says. “However, our new reimbursement environment focuses heavily on patient satisfaction and has changed the patient/clinician dynamic. I now tell my patients: ‘You’re the captain of the ship, but I’m your navigator. Our job is to work together to avoid any icebergs.’” Finding ways to ensure patients are involved in — and satisfied with — their care is one of the biggest challenges facing providers today, says Freeman. “We have to make sure patients are happy with their care, while also making sure we collect the necessary metrics for reimbursement. However, when done right, this is also the biggest reward.”
"In the past, the physician was responsible for managing a patient’s care and patient input mattered much less ... However, our new reimbursement environment focuses heavily on patient satisfaction and has changed the patient/clinician dynamic. I now tell my patients: ‘You’re the captain of the ship, but I’m your navigator. Our job is to work together to avoid any icebergs." — Andrew Freeman, MD, FACC
Freeman leads Walk With A Doc programs each month that provide an opportunity to not only model healthy behavior, but get to know patients in a more informal setting. Walk With A Doc is a global program that started in 2005 and has grown to include more than 300 Chapters worldwide. He has also established a workplace wellness portal where his patients and staff are encouraged to take part in healthy activities. “Patient-centered programs like these that directly address patients’ needs, preferences, circumstances and well-being can lead to greater satisfaction and hopefully improved outcomes. It can also make medicine fun,” he says.
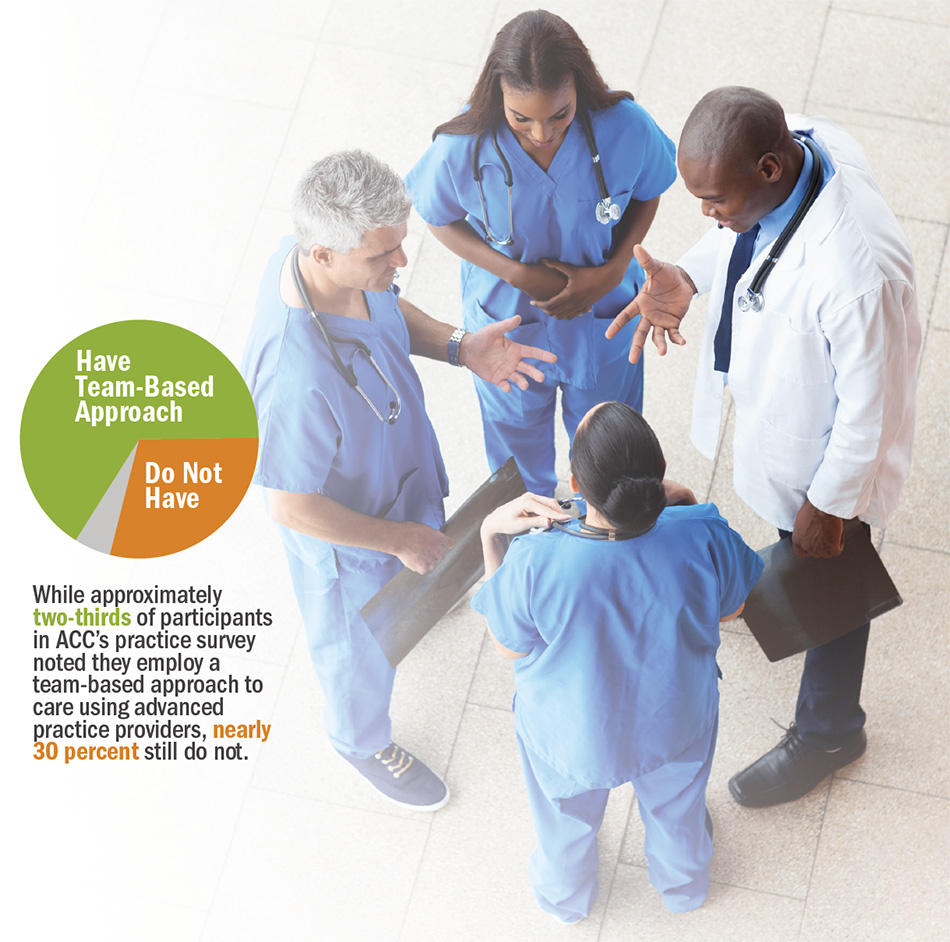
It’s not just patients who need to be part of the care team. A 2015 ACC Health Policy Statement on Cardiovascular Team-Based Care and the Role of Advanced Practice Providers highlights the importance of advanced practice providers in helping cardiovascular practices meet the challenges of workforce shortages, an aging patient population with growing complexities in care and a payment system in transition.
While approximately two-thirds of participants in ACC’s practice survey noted they employ a team-based approach to care using advanced practice providers, nearly 30 percent still do not. Among the biggest barriers to care: no established roles, responsibilities or expectations; a traditional view of patients and providers where care is delivered by an individual physician; lack of reimbursement; and no clear practice model. “We are still not using advanced practice providers to their full extent,” says Biga. “There’s lots of talk about team-based care, but we’re not living it in the real world. We need to move from concept to implementation.”
"This is a great opportunity to ‘up our game’ with positive effects across many functional areas of practices today." — Pamela S. Douglas, MD, MACC
Workforce well-being is the most recent concept to enter the lexicon of what defines a high-functioning practice. “The Institute for Healthcare Improvement recently expanded its widely accepted ‘triple aim’ to a ‘quadruple aim,’ adding provider well-being to cost, access and population health,” says Douglas. “Many practices suffer from the effects of inattention to this: burnout, attrition, poor team functioning, etc., and it will only worsen as the demands on practices continue to grow.”
Both Douglas and Valentine note that workforce well-being is shaping up to be an important part of the ACC’s strategic priorities for 2018, as well as key element of focus as the College plans its next Strategic Plan. It will also be a key part of the Cardiovascular Summit. “This is a great opportunity to ‘up our game’ with positive effects across many functional areas of practices today,” says Douglas. Valentine adds that preventing burnout, ensuring clinician wellness and improving employee competence can have very real impacts on patient satisfaction and successful team-based care.
“It’s important to balance mental, physical and spiritual health,” says Valentine. In my own life, I’m very focused on regular exercise which I think helps more than anything.”
What’s Next?
“Practices need dyad leadership in order to survive this,” says Biga. “If done successfully it is absolutely possible to balance business trends with the quality and patient outcomes that are mandated by the quadruple aim. Biga and Valentine stress the importance of building leaders and helping identify those who can effectively wear both a lab coat and a suit coat. They also note the importance of having a clear vision and strategic plan. This can help ensure practices are focused on more holistic strategic goals and not lost in “managing to metrics,” Douglas adds.
Tweet this article: Tweet
|
 |
|
| Click the cover image above to read the latest issue of Cardiology in e-pub format or click here to read it on the web! | |
Keywords: ACC Publications, Cardiology Magazine, Fee-for-Service Plans, Accountable Care Organizations, Patient Satisfaction, Cost Savings, Motivation, Personal Satisfaction, Workplace, Medicare, Group Practice, Mandatory Reporting, Health Policy, Registries
< Back to Listings


