Training, Exercise, and Sports in the Age of COVID-19: Session Recap
The opening event for the first virtual American College of Cardiology (ACC) Care of the Athletic Heart 2020 meeting was a high-profile panel session discussing the very topic that prompted the transition to a virtual format: COVID-19. Along with most of the worldwide economy, the entire sporting world shut down in March 2020. As societies have embarked on their reopening plans, a central question among sports medicine and cardiology practitioners has been: How can we safely resume sport and exercise in the current pandemic environment?
This topic was the focus of a featured session of Athletic Heart Virtual 2020, entitled "Training, Exercise, and Sports in the Age of COVID-19." Course director Dr. Jonathan Kim, Director of Sports Cardiology at Emory University, moderated an expert panel consisting of:
- Dr. Jonathan Finnoff, Chief Medical Officer of the US Olympic & Paralympic Committee,
- Dr. Celine Gounder, Infectious Disease Specialist at NYU Langone Health and CNN Medical Correspondent,
- Dr. Benjamin Levine, Distinguished Professor of Exercise Sciences at UT Southwestern Medical Center,
- Dr. Dermot Phelan, Director of Sports Cardiology at Sanger Heart & Vascular Institute, and
- Dr. Paul Thompson, Chief Emeritus of Cardiology at Hartford Hospital.
The panel shared their expert opinions on the challenging questions that currently face the sports cardiology community. The discussion revolved around three major areas, as detailed below.
Return-to-Play in Athletes with COVID-19
With early studies demonstrating evidence of troponin elevations in roughly 20% of hospitalized patients with COVID-191 and with continued concern about a myocarditis pathophysiology,2 the panelists discussed the concern that even young, otherwise healthy athletes may experience subclinical myocardial injury if they acquire COVID-19. Dr. Phelan, co-lead author with Dr. Kim on the recently published recommendations in JAMA Cardiology for resumption of sport and exercise after COVID-19,3 described the rationale behind the authors' relatively conservative recommendations for athletes who test positive for COVID-19. For instance, per these recommendations, athletes who test positive and are asymptomatic are advised to rest with no exercise for 2 weeks. If mildly symptomatic but not hospitalized, athletes are advised to avoid exercise for 2 weeks after symptom resolution, followed by medical evaluation that may include checking a troponin level, electrocardiogram, and echocardiogram. The majority of the panel agreed with these conservative recommendations, and Dr. Phelan emphasized that with the lack of robust data, it is important to err on the side of caution, even in apparently otherwise healthy patients. Dr. Levine pointed to studies showing increases in out-of-hospital cardiac arrests during the pandemic, further increasing concern that we are uncertain of the true prevalence of myocardial injury in COVID-19. More studies are needed on the prevalence of cardiovascular involvement of COVID-19 and its longer-term effects in the athlete population, as these data can help refine (and perhaps liberalize) the current recommendations.
Per Dr. Levine, the priorities in counseling athletes on return to play after a COVID-19 diagnosis should be to: (1) Protect the individual athlete, and (2) Protect the team and staff. With regard to #1, as part of the recommendations mentioned above, athletes recovering from COVID-19 are advised to return to exercise and sport slowly under the guidance of a health care team. Yet, this return should take into consideration the risks of the individual (e.g., comorbidities) and of the sport (e.g., level of peak intensity). With regard to #2, potential infectious risks to teammates and staff must be considered if allowing the athlete to return to sport participation. The individual versus team-based nature of the sport should also be taken into consideration here.
Training and Exercise in the Age of COVID-19
An ongoing challenge in this pandemic has been determining a safe way for people of all athletic levels to continue to train and exercise. For those athletes without known disease, the question is how to minimize the risk of either becoming infected or asymptomatically transmitting disease to others while exercising. Notably, most gyms and workout studios have been closed over the past few months, and Dr. Gounder and panelists questioned whether exercising in an indoor gym could be considered safe any time in the near future.
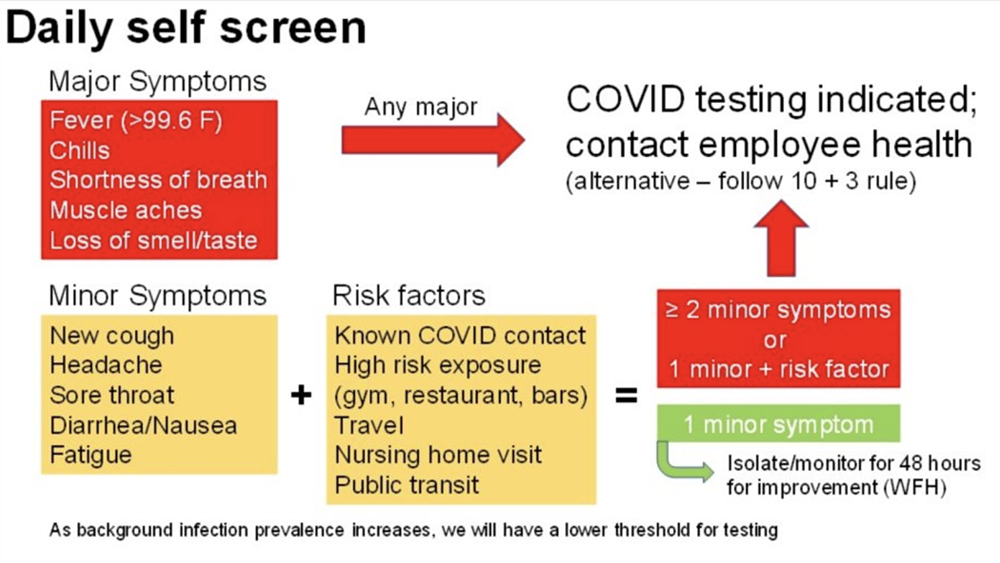
For competitive athletes, Dr. Thompson recommended that the decision to allow return to team practice and competition should factor in: (1) Local community prevalence and trends of COVID-19 cases, (2) Symptom and/or test-based screening of athletes, and (3) Infectious risks of the sport. With regard to #2, there were varying opinions among the panel of the efficacy and utility of a symptom-based screening strategy, and Dr. Gounder pointed out the well-known concern for asymptomatic transmission of COVID-19. She advocated for the need to regularly test athletes for COVID-19, describing the differences between the polymerase chain reaction (PCR), antibody-based, and newer antigen-based tests. Yet clearly there is severely limited capacity to perform these tests broadly. Dr. Finnoff highlighted the salient point that requirements of these tests will inevitably exacerbate disparities between socioeconomic communities, as access to testing will likely be scarce in poorer areas. To help guide a symptom-based self-screening strategy, Dr. Levine suggested the use of a clear self-screening protocol, and he shared a working algorithm used by his research team (Figure 1). Such procedures are clearly more accessible, though the ultimate efficacy in reducing disease spread in the sport community remains to be determined.
Figure 1: Sample daily self-screening algorithm4
Yet arguably the most critical aspect of deciding to resume a team-based competitive sport is the firm establishment of a code of conduct among the team members and staff. Leaders must emphasize the necessity of every single member of the team to eliminate high-risk behavior from their activities outside of practice and competition, such as strict adherence to social distancing practices and avoidance of large gatherings or parties. If team members cannot adhere to this code of conduct, they should not be allowed to participate in practice and competition, as they pose an increased risk to the other athletes, coaches, staff, and themselves.
For the recreational athlete, the panelists reiterated the importance that regular physical activity be continued. While many gyms remain closed, they suggested outdoor and physically spaced activities. For cardiovascular activities such as jogging and cycling, Dr. Levine shared the motto of the four D's: "Double your Distance. Don't Draft." While we are advised to generally stay at least 6 feet away from other people, he advises this distance should be increased to at least 12 feet while exercising, given the aerosolizing nature of heavy breathing during exercise. Further, he cautions that entering the airstream draft of another runner or cyclist in front of you may increase the risk of inhaling their expired particulate matter.
The Near-term Future of Sporting Events in the COVID-19 Era
After professional sports worldwide came to a complete halt in early March 2020, the absence of sports only served to remind us of just how deeply interwoven into our society they were. While some professional leagues have returned successfully thus far (i.e., Bundesliga football league in Germany, the Korean Baseball Organization league), many professional leagues in the United States have encountered significant obstacles in their plans to resume competition. Yet for the foreseeable future, the professional sporting environment will be far from normal, as teams will compete in empty stadiums and arenas.
The Summer Olympic and Paralympic Games, the world's largest sporting event, were postponed until 2021. Dr. Finnoff described the tremendous challenges that the US Olympic and Paralympic committee has faced in preparing American athletes for the event in the current environment, and he elaborated on the meticulous details of the policies they have implemented to create a safe training environment for the athletes. Yet, given the international nature of the Games, there will be heterogeneity in these policies between countries, and the ability of all participating countries to successfully guide their athletes through training and Trials and ultimately the Games is uncertain. Thus, Dr. Finnoff emphasized the complexity of this planning process, and the Games will inevitably be markedly different from the Olympic and Paralympic Games we are used to seeing.
Finally, Dr. Kim concluded the session commenting that the return of recreational endurance exercise events, such as local road races and larger high-profile marathons, will most likely and unfortunately be the last sporting events to return. While not impossible to conduct an event, the tremendous logistics involved to ensure the safety of runners and volunteers demands significant control of the pandemic. Until we are there from a public health standpoint, mass gathering events present high risk and should be avoided.
Summary
As with the rest of global societies, the world of sport and exercise has been upended by the pandemic. More robust data are needed to help the sports cardiology community guide its athletes to a responsible and reasonably safe resumption of competition. The panelists called for the swift collection of COVID-19 data relevant to our patients and its rapid dissemination to the sports cardiology community. Until then, the priorities must be to protect the health of the individual athlete and to protect other team members and staff. Organization leaders should err on the side of caution, even if it means making the difficult decision to cancel competition, as we aim to move towards a "new normal" for our athletes.
For those who registered for ACC Care of the Athletic Heart Virtual 2020, the video recordings of this two-part session (as well as all of the other sessions of the meeting) are available on-demand through the end of the year at ACC.org.
References
- Shi S, Qin M, Shen B, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol 2020;5:802-10.
- Hendren NS, Drazner MH, Bozkurt B, Cooper LT Jr. Description and proposed management of the acute COVID-19 cardiovascular syndrome. Circulation 2020;141:1903–14.
- Phelan D, Kim JH, Chung EH. A game plan for the resumption of sport and exercise after coronavirus disease 2019 (COVID-19) infection. JAMA Cardiol 2020 May 13 [Epub ahead of print].
- Levine B, Sarma T. Slides included in "Training, Exercise, and Sports in the Age of COVID-19". Presented by Dr. Benjamin Levine at the Care of the Athletic Heart.20 Virtual Course, June 20, 2020.
Clinical Topics: COVID-19 Hub, Sports and Exercise Cardiology
Keywords: Sports, Athletes, COVID-19, Pandemics, Public Health, severe acute respiratory syndrome coronavirus 2, Coronavirus, Particulate Matter, Volunteers
< Back to Listings