Predicting Long-Term Absence of Coronary Artery Calcium in Metabolic Syndrome and Diabetes
Quick Takes
- Among individuals with metabolic syndrome (MetS) and/or type II diabetes (T2DM) who had a baseline coronary artery calcium score (CAC) of 0, more than 40% remained free of coronary calcium on repeat imaging 10 years later. This demonstrates a heterogeneous risk for the development of coronary atherosclerosis in this group of individuals who are traditionally classified as intermediate-high risk.
- In patients with MetS and/or T2DM with a baseline CAC of 0, the strongest predictors of long-term absence of CAC were an absence of extracoronary atherosclerosis and a low metabolic syndrome score. These results provide additional information that may be useful for the clinician-patient risk discussion regarding whether to initiate primary prevention pharmacotherapies.
Introduction
The prevalence of MetS and T2DM has greatly increased and is predicted to affect over 700 million people worldwide by 2045.1,2,3 Persons with MetS and T2DM are often considered to have a uniformly increased risk for atherosclerotic cardiovascular disease (ASCVD). Accordingly, statin therapy is recommended for persons with diabetes aged 40-75 years old and an LDL-C ≥70 mg/dL, regardless of their estimated ASCVD risk.4,5
However, CAC more accurately classifies an individual's ASCVD risk compared to traditional ASCVD risk factors, because it is a direct measure of subclinical coronary atherosclerosis that integrates the cumulative effects of risk factor exposure and genetics. Notably, a CAC score of 0 is associated with a low risk for ASCVD events over the next decade even among patients with diabetes.6,7 Approximately 40% of individuals with MetS or T2DM may be expected to have a CAC score of 0, which demonstrates significant heterogeneity in risk among this group of individuals.8
The focus of this recent investigation was to add further information to the understanding of healthy arterial aging among individuals with MetS or T2DM by examining the proportion of individuals with a long-term absence of CAC and the risk predictors for this healthy arterial aging phenotype. Here, we summarize the findings of this recent Multi-Ethnic Study of Atherosclerosis (MESA) substudy.
Methods
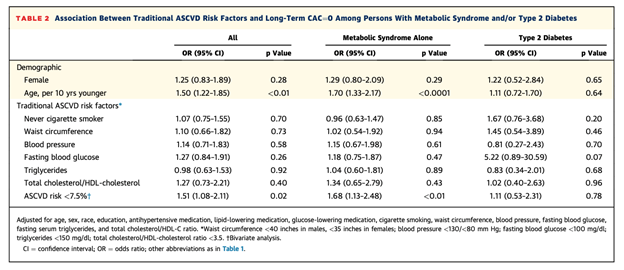
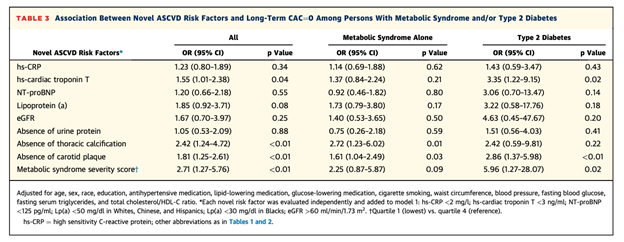
A total of 574 patients from the MESA database were selected based on three inclusion criteria 1) diagnosis of MetS and/or T2DM, 2) a CAC of 0 at baseline, and 3) a follow-up CAC scan 10 years later. The study used multivariable logistic regression to examine the association between 1) normal/ideal values of traditional risk factors (cigarette smoking, blood pressure, fasting blood glucose, age, smoking, cholesterol, etc.) and 2) novel atherosclerotic disease risk factors (thoracic aortic calcification, carotid plaque, high sensitivity troponin, MetS severity Z-score, etc.) with the maintenance of CAC of 0 at follow up scan 10-year follow-up.
Results
Of the 574 subjects, 422 had MetS and 152 had T2DM. The mean age was 59 years old, and 67% were women. There was a similar proportion of individuals with long-term CAC of 0 between the T2DM group and the MetS group (41.5% vs. 42%, respectively). Among individuals who did develop incident CAC, the median CAC score was low, at about 30, regardless of age group, ASCVD risk, or diagnosis of MetS/T2DM.
Among all the individual traditional ASCVD risk factors, only a younger age was associated with a higher likelihood of a long-term maintenance of CAC=0 (Odds Ratio [OR] 1.50; 95% Confidence Interval [95% CI] 1.22-1.85). However, among nontraditional risk factors, an absence of thoracic calcification (OR 2.42; 95% CI 1.24 to 4.72), absence of carotid plaque (OR 1.81; 95% CI 1.25 to 2.61), high sensitivity troponin <3 ng/ml (OR 1.55; 95% CI 1.01 to 2.39) and a MetS severity score in the lowest quartile (OR 2.71; 95% CI 1.27 to 5.76) were all significantly associated with the long-term absence of CAC. There was no association of Lp(a), hsCRP, or NT-proBNP with maintenance of CAC of 0.
Conclusion and Interpretation
This study employed a novel approach of examining predictors for healthy arterial aging in persons with MetS or T2DM, who are traditionally classified as intermediate to high-risk. This MESA substudy is most notable for its finding that approximately 40% of participants with MetS or T2DM maintained a CAC of 0 during a 10-year follow up period. Additionally, it demonstrated that among individual traditional risk factors only a younger age was significantly associated with long-term CAC=0, but that the strongest predictors of maintaining a long-term CAC=0 were an absence of extracoronary atherosclerosis and low MetS severity score.
These results show that younger patients with MetS and/or diabetes who have a low metabolic severity score are most likely to maintain healthy arterial aging. Furthermore, the absence of carotid or thoracic aortic atherosclerosis were the strongest individual negative risk markers. A finding of a CAC=0 has up to an 80% reduction in post-test risk for coronary heart disease. Thus, an optimal cardiovascular risk profile with the absence of extracoronary atherosclerosis is more important than an ideal valve of any individual risk factor for the maintenance of healthy artery aging.
While the current guidelines recommend a uniform approach to initiating primary prevention pharmacotherapy in patients with diabetes, the results from this study suggests that further investigation is needed to more accurately define this group's heterogeneous risk for developing atherosclerosis and ASCVD.
References
- Geiss LS, Wang J, Cheng YJ, et al. Prevalence and incidence trends for diagnosed diabetes among adults aged 20 to 79 years, United States, 1980-2012. JAMA 2014;312:1218-26.
- Saklayen MG. The global epidemic of the metabolic syndrome. Curr Hypertens Rep 2018;20:12.
- IDF Diabetes Atlas 9th Edition 2019 (International Diabetes Federation website). 2019. Available at https://www.diabetesatlas.org/en/. Accessed 11/23/2020.
- Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019;74:1376-1414.
- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019;73:3168-3209.
- Greenland P, Blaha MJ, Budoff MJ, Erbel R, Watson KE. Coronary calcium score and cardiovascular risk. J Am Coll Cardiol 2018;72:434-47.
- Blaha MJ, Cainzos-Achirica M, Greenland P, et al. Role of coronary artery calcium score of zero and other negative risk markers for cardiovascular disease: the Multi-Ethnic Study of Atherosclerosis (MESA). Circulation 2016;133:849–58.
- Wong ND, Sciammarella MG, Polk D, et al. The metabolic syndrome, diabetes, and subclinical atherosclerosis assessed by coronary calcium. J Am Coll Cardiol 2003;41:1547–53.
Clinical Topics: Diabetes and Cardiometabolic Disease, Dyslipidemia, Prevention, Atherosclerotic Disease (CAD/PAD)
Keywords: Dyslipidemias, Metabolic Syndrome, Diabetes Mellitus, Diabetes Mellitus, Type 2, Coronary Artery Disease, Calcium, Dietary, Primary Prevention, Atherosclerosis
< Back to Listings