ACC, AHA, ESC, WHF Issue Joint Opinion on Improving Clinician Well-Being Worldwide
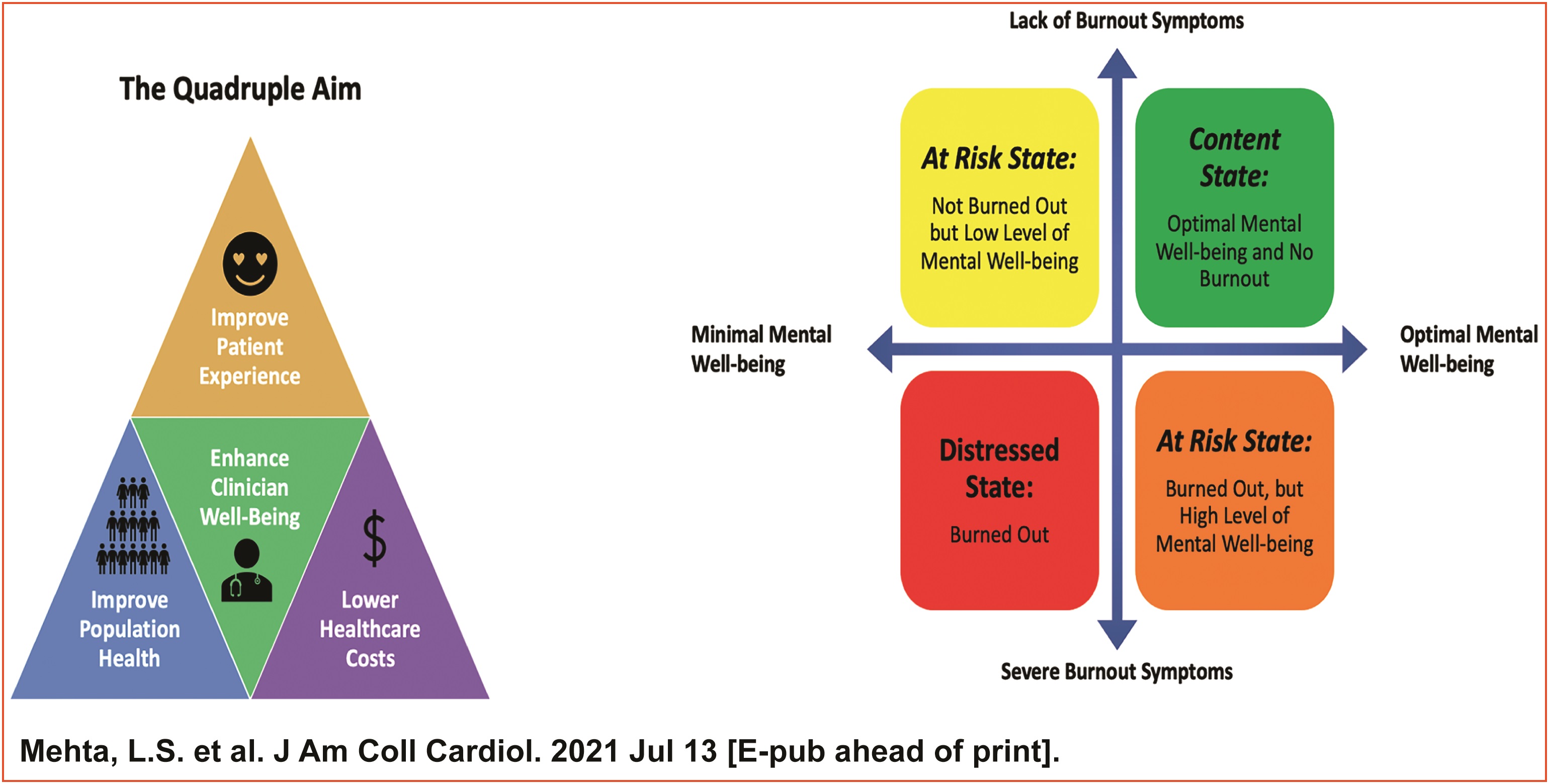
Clinician well-being is imperative to providing high-quality patient care, yet clinician burnout continues to increase, especially over the last year due to the COVID-19 pandemic. A joint opinion paper released July 13 by the ACC, American Heart Association (AHA), European Society of Cardiology (ESC) and World Heart Federation (WHF), calls for global action to improve clinician well-being.
Recent survey data among 2,274 U.S. cardiologists and fellows-in-training reported that more than one-quarter were burned out and almost 50% were stressed. Only 23.7% said that they enjoyed their work. Women reported burnout more frequently compared with men.
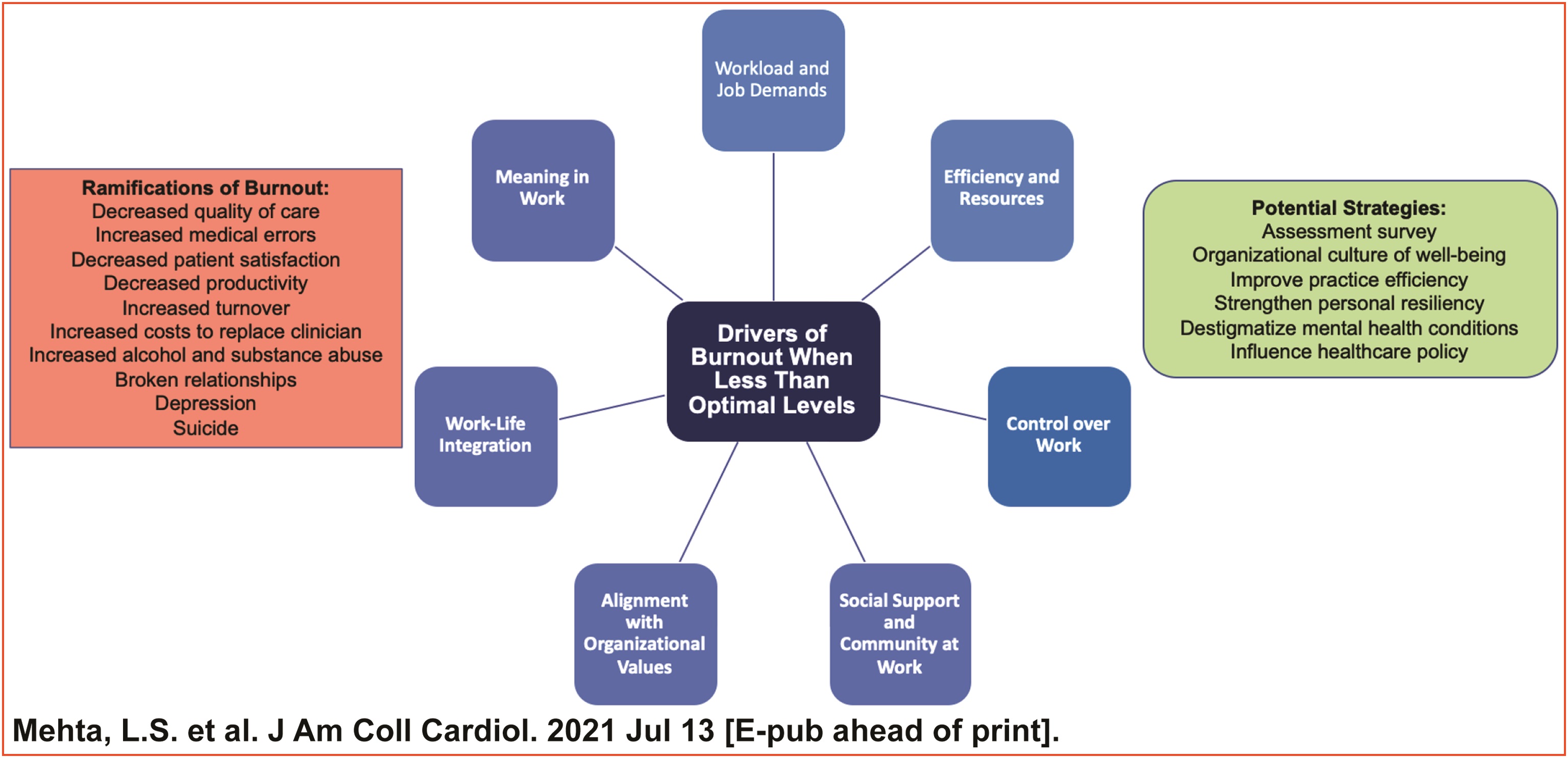
Drivers associated with burnout among cardiologists include lack of control over workload, a hectic work environment, misalignment of values and insufficient documentation time. Furthermore, women are under-represented in cardiology and may have added stressors contributing to burnout such as lack of career promotion, inequalities in income and disparities in mentorship, in addition to working in environments that lack diversity, equity, inclusion and belonging.
"Over the last several decades, there have been significant changes in health care with the expansion of technology, regulatory burden and clerical task loads. These developments have come at a cost to the well-being and work-life integration of clinicians," said Athena Poppas, MD, MACC, immediate past president of the ACC and co-author of the joint opinion. "The COVID-19 pandemic has caused additional strain on clinicians through increased patient mortality, personal and family safety concerns, fear of the unknown and increased work demands. The time is now to join with our global health care professionals to call for quick action to improve clinician well-being worldwide."
"These stressors compound over time, and collectively, they diminish our abilities to provide high-quality patient care and to strengthen and diversify our workforce. In addition, stigma related to mental health care must be eradicated," said Mitchell S.V. Elkind, MD, MS, immediate past president of the AHA. "Our organizations are joined together in this report to ensure that we create a strong and supportive clinician environment – for our personal well-being and for our families, loved ones and patients. Well-being is essential to achieving personal fulfilment and satisfaction in our work."
There are serious personal and professional ramifications of clinical burnout. Personal ramifications of burnout consist of higher rates of alcohol abuse, substance use, dysfunctional relationships, depression and suicide. Professional ramifications of clinician burnout include higher rates of medical errors, lower quality of care, decreased patient satisfaction, increased disruptive behavior and loss of professionalism accompanied by a decreased level of empathy.
"The rising rate of stress and burnout among health professionals rings an alarm bell. As well as serious consequences for the individual, they will impact patient care. The ESC joins other professional societies today to raise a red flag and to urge health care systems to create healthy environments for all those providing patient care," said Stephan Achenbach, MD, FACC, ESC president.
The joint opinion urges health care organizations and medical specialty societies to implement strategies to prevent clinician burnout. For health care organizations, suggested prevention strategies include:
- Support the psychosocial health of employees and be accountable for a holistic approach.
- Create an organizational infrastructure within which clinicians can thrive.
- Provide employees with a structure that allows for confidential reporting of mistreatment, as well as destigmatization of clinician access to mental health resources.
For medical specialty societies, suggested prevention strategies include:
- Continue to provide recommendations to health care organizations and advocate for meaningful health policy changes.
- Develop specialty-specific tools that may improve practice efficiency or clinician knowledge base in a timely and convenient fashion.
- Expand initiatives in diversity and inclusion to improve feelings of being valued and belonging.
"Even before the COVID-19 pandemic, clinicians were often struggling in existing health systems that did not fully support them," said Fausto J. Pinto, MD, PhD, FACC, president of the WHF. "Strategies to prevent clinician burnout must target the root causes of the problem. Medical societies, as well as civil society foundations, have an important role to play in creating support networks for their members and pushing governments to enact meaningful health policy changes."
"As clinicians, we continuously strive for the improved health of our patients and at the same time recognize our own welfare is paramount to them receiving optimal care," said Laxmi S. Mehta, MD, FACC, chair of the report. "We will continue to work together and strategize to maintain the well-being of our workforce and keep the joy in cardiovascular medicine."
The joint opinion published simultaneously in the Journal of the American College of Cardiology, Circulation, European Heart Journal and Global Heart.
Clinical Topics: COVID-19 Hub
Keywords: ACC International, Workload, Health Resources, Personal Satisfaction, Patient Satisfaction, Mental Health, Alcoholism, COVID-19, Depression, Quality of Health Care, Patient Care, Health Policy
< Back to Listings