Statin Therapy Allocation in Intermediate Risk Population
Quick Takes
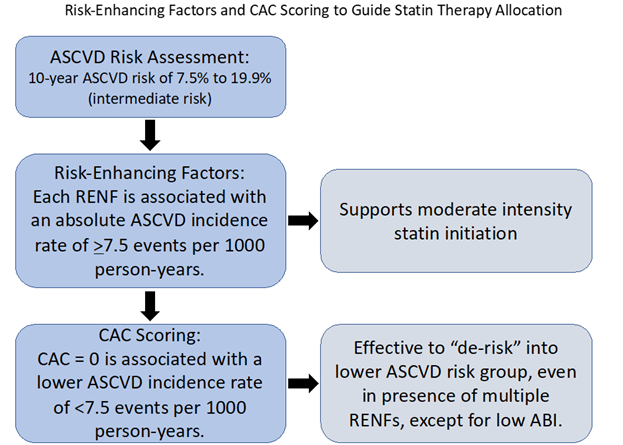
- Among those at intermediate risk by the Pooled Cohort Equations (PCE), each atherosclerotic cardiovascular disease (ASCVD) risk-enhancing factor (RENF) was found to be associated with an average ASCVD incidence rate above the threshold for consideration of statin therapy.
- The absence of coronary artery calcium (CAC=0), however, is associated with a lower incidence of ASCVD events, a rate which is below the recommended threshold of 7.5% for starting statin therapy, even in the presence of multiple RENFs (except for low ankle-brachial index). Thus, a CAC score of 0 can "de-risk" many individuals with RENFs into a lower risk group for ASCVD over the next decade.
- CAC scoring is a useful tool to more accurately risk stratify individuals with intermediate risk of ASCVD and to guide preventive pharmacotherapy. Nevertheless, RENFs are associated with increased long-term risk of ASCVD, and their presence may be used to further emphasize lifestyle optimization.
Introduction
The 2018 AHA/ACC/Multisociety (MS) guideline on the management of blood cholesterol recommends initiation of moderate-intensity statin in adults 40 to 75 years of age without diabetes mellitus and with LDL-C levels >70 mg/dl, at 10-year atherosclerotic cardiovascular disease (ASCVD) risk of 7.5% to 19.9% (intermediate risk), if discussion of treatment options favors statin therapy. This decision may also be influenced by the presence of one or more risk-enhancing factors (RENFs).1 Coronary artery calcium (CAC) scoring is recommended as an optional next step, if there is still uncertainty regarding whether statin therapy should be initiated.1
ASCVD Risk-Enhancing Factors
RENFs include family history of premature ASCVD, chronic kidney disease (CKD), metabolic syndrome, premature menopause (age <40 years), persistent hypertriglyceridemia ≥175 mg/dl, high-sensitivity C-reactive protein (hsCRP) ≥2.0 mg/L, lipoprotein (a) (Lp[a]) ≥50 mg/dL, apolipoprotein B100 (apo B100)≥130 mg/dL, and ankle-brachial index (ABI) <0.9.1
The 2018 AHA/ACC/MS cholesterol guideline referenced different studies in which the relationship between RENFs and ASCVD risk were assessed as the basis for the above recommendation. However, there was no study that quantified the relationship between the presence of RENFs and ASCVD incidence rates for all the above RENFs in a single, ethnically diverse population.
A recent analysis was performed regarding individuals aged 45 to 75 years of age with no clinical ASCVD or diabetes at baseline in the Multi-Ethnic Study of Atherosclerosis (MESA), a multicenter population-based prospective cross-sectional study in the United States. The authors found that on average the ASCVD incidence rates for each RENF was 7.5 or more events per 1000 person-years, the highest of which was premature menopause at 10.3 events per 1000 person-years (95% CI, 5.1-20.6).2 This data indicates that the presence of an individual RENF supports the use of statin therapy as advocated by the 2018 cholesterol guideline.
CAC Scoring
The 2018 AHA/ACC/MS cholesterol guideline also states that in intermediate-risk and selected borderline-risk individuals in whom the decision to initiate statin therapy remains uncertain, it is reasonable to use a CAC score to aid in the decision.1 Several studies have reported 10-year event rates of ASCVD below the threshold for statin initiation in adults with individual RENFs and CAC=0.3,4
The recent MESA analysis found even lower short-term event rates for both individual and combined RENFs (except for low ABI); this implies that even if an adult has multiple RENFs, a CAC score of 0 is enough to re-stratify them into a lower ASCVD risk category where initiating a statin at that time may not offer significant benefit over the next decade.2,5 This also held true in an analysis of grouped basic and advanced RENFs. Basic RENFs are those which were readily available to the clinician (family history of premature ASCVD, CKD, metabolic syndrome, premature menopause, hypertriglyceridemia) and advanced RENF are those which were not (elevated hsCRP, Lp[a], and apo B100, and low ABI).2
Implications in Women
In most cases, aside from low ABI, approximately half of women in the MESA analysis with at least one RENF had CAC score of 0.2 This held true even in those with ≥3 RENFs.2 In the prospective Chronic Renal Insufficiency Cohort study, 50% of women with CKD and eGFR of 20 to 70 mL/min/1.73m2 had a CAC of 0.4 Similarly, in women with premature ovarian insufficiency, the prevalence of CAC=0 at age ≥45 was similar to age- and race-matched controls without ovarian insufficiency.6
In MESA, even in women with premature menopause who had the highest absolute ASCVD incidence rate of the RENFs assessed, the absence of calcium was associated with a risk which was relatively low and well below the usual threshold for statin initiation.2 This implies that without CAC scoring it may be difficult to accurately assess ASCVD risk in women with RENFs. Thus, a CAC score can be considered for more accurate risk assessment.
Lifetime Risk
The absence of CAC, especially among young individuals, does not indicate low lifetime risk; therefore, such individuals should continue to focus on maintaining a healthy lifestyle. Indeed, a CAC score of 0 can progress to detectable within 5-10 years, particularly in adults with RENFs.7,8 As such, a repeat CAC scan in about 5 years would be reasonable for those with diabetes or family history of premature coronary heart disease (CHD) who prefer not to start a statin, as outlined by available guidelines.6
Life's Simple 7® paradigm advocates for managing blood pressure, controlling cholesterol, reducing blood sugar, daily physical activity, healthy diet, weight loss, and smoking cessation in all adults.8 The presence of an RENF's should be considered as a marker of having a higher long-term risk of ASCVD.
Conclusions
The 2018 AHA/ACC/MS cholesterol guideline for adults ages 40-75 years of age without diabetes mellitus and with LDL-C level >70 with an estimated 10-year ASCVD risk between 7.5% and 19.9% (intermediate risk) recommends initiation of moderate-intensity statin if discussion of statin therapy favors statin initiation, particularly if there are RENFs present.1 The study by Patel et al. indicates that the presence of an individual RENF may warrant statin consideration.2 However, there is discordance when also considering the use of CAC, as even in the presence of multiple RENFs, a CAC score of zero is associated with a risk level which is below the current recommended statin initiation threshold, except for those with a low ABI.2
Given the approximate 50% prevalence of CAC scores of 0 in women with RENFs, except for low ABI, it may be challenging to accurately risk stratify women who are at intermediate risk of ASCVD without CAC scoring. CAC scoring can help re-classify adults into lower ASCVD risk categories and support delaying statin use at a time when there might be little benefit over the next 5-10 years.2,5
Given that CAC scores of 0 are likely to progress over the course of 15-20 years, a CAC score of 0 should still motivate individuals to make healthy lifestyle modifications where possible to prevent the development of measurable subclinical coronary atherosclerosis. The authors of this MESA analysis argue that CAC scores should be considered for intermediate risk adults, who are not inclined to go on statin therapy or those uncertain of its benefit to guide statin therapy initiation.
Figure 1
References
- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019;73:e285-e350.
- Patel J, Pallazola VA, Dudum R, et al. Assessment of coronary artery calcium scoring to guide statin therapy allocation according to risk-enhancing factors: the Multi-Ethnic Study of Atherosclerosis. JAMA Cardiol 2021;Jul 14:[Epub ahead of print].
- Malik S, Zhao Y, Budoff M, et al. Coronary artery calcium score for long-term risk classification in individuals with type 2 diabetes and metabolic syndrome from the Multi-Ethnic Study of Atherosclerosis. JAMA Cardiol 2017;2:1332-40.
- Chen J, Budoff MJ, Reilly MP, et al. Coronary artery calcification and risk of cardiovascular disease and death among patients with chronic kidney disease. JAMA Cardiol 2017;2:635-43.
- Mitchell JD, Fergestrom N, Gage BF, et al. Impact of statins on cardiovascular outcomes following coronary artery calcium scoring. J Am Coll Cardiol 2018;72:3233-42.
- Gunning MN, Meun C, van Rijn BB, et al. Coronary artery calcification in middle-aged women with premature ovarian insufficiency. Clin Endocrinol (Oxf) 2019;91:314-22.
- Dzaye O, Dardari ZA, Cainzos-Achirica M, et al. Warranty period of a calcium score of zero: comprehensive analysis from MESA. JACC Cardiovasc Imaging 2021;14:990-1002.
- Han L, You D, Ma W, et al. National trends in American Heart Association revised Life's Simple 7 metrics associated with risk of mortality among US adults. JAMA Netw Open 2019;2:e1913131.
Clinical Topics: Diabetes and Cardiometabolic Disease, Dyslipidemia, Advanced Lipid Testing, Hypertriglyceridemia, Lipid Metabolism, Nonstatins, Novel Agents, Statins
Keywords: Middle Aged, C-Reactive Protein, Hydroxymethylglutaryl-CoA Reductase Inhibitors, Calcium, Cholesterol, LDL, Cross-Sectional Studies, Coronary Vessels, Lipoprotein(a), Metabolic Syndrome, Ankle Brachial Index, Cardiovascular Diseases, Menopause, Premature, Menopause, Premature, Prospective Studies, Prospective Studies, Atherosclerosis, Cholesterol, Diabetes Mellitus, Hypertriglyceridemia, Renal Insufficiency, Chronic, Apolipoproteins, Women, Blood Pressure, Renal Insufficiency, Hydroxymethylglutaryl-CoA Reductase Inhibitors
< Back to Listings