Dementia and Specialty Palliative Care Referral: Early Screening and Assessment for Older Adults with Cardiovascular Disease
Quick Takes
- There is a pathophysiologic and epidemiologic overlap in dementia and cardiovascular disease (CVD). Consider performing a cognitive assessment to screen for dementia if clinical suspicion exists.
- Despite known benefits of palliative care and hospice in advanced dementia and CVD, these specialty services are underutilized. Challenges to prognosis, heterogeneous disease characteristics, and access to specialty services are some of the major barriers to care.
- We recommend early referral to specialty palliative care for patients with CVD and dementia, which may assist in complex decision making and timely referral to hospice. Future research is needed to validate reliable screening tools in this patient population.
Geriatric Cardiology Take Home Points
- Though the exact prevalence of dementia in patients with cardiac disease is difficult to quantify, there is substantial intersection in the pathophysiology and epidemiology of the two diagnoses.1
- Specialty palliative care and hospice are underutilized in patients with cardiovascular disease (CVD) and dementia. There are many shared barriers to referrals, including challenges to prognosis, unpredictable disease trajectory, and access to resources.2-4
- Patients with both CVD and dementia are at increased risk of complicated palliative care needs, and referral to specialty palliative care should be considered at early signs of cognitive decline.
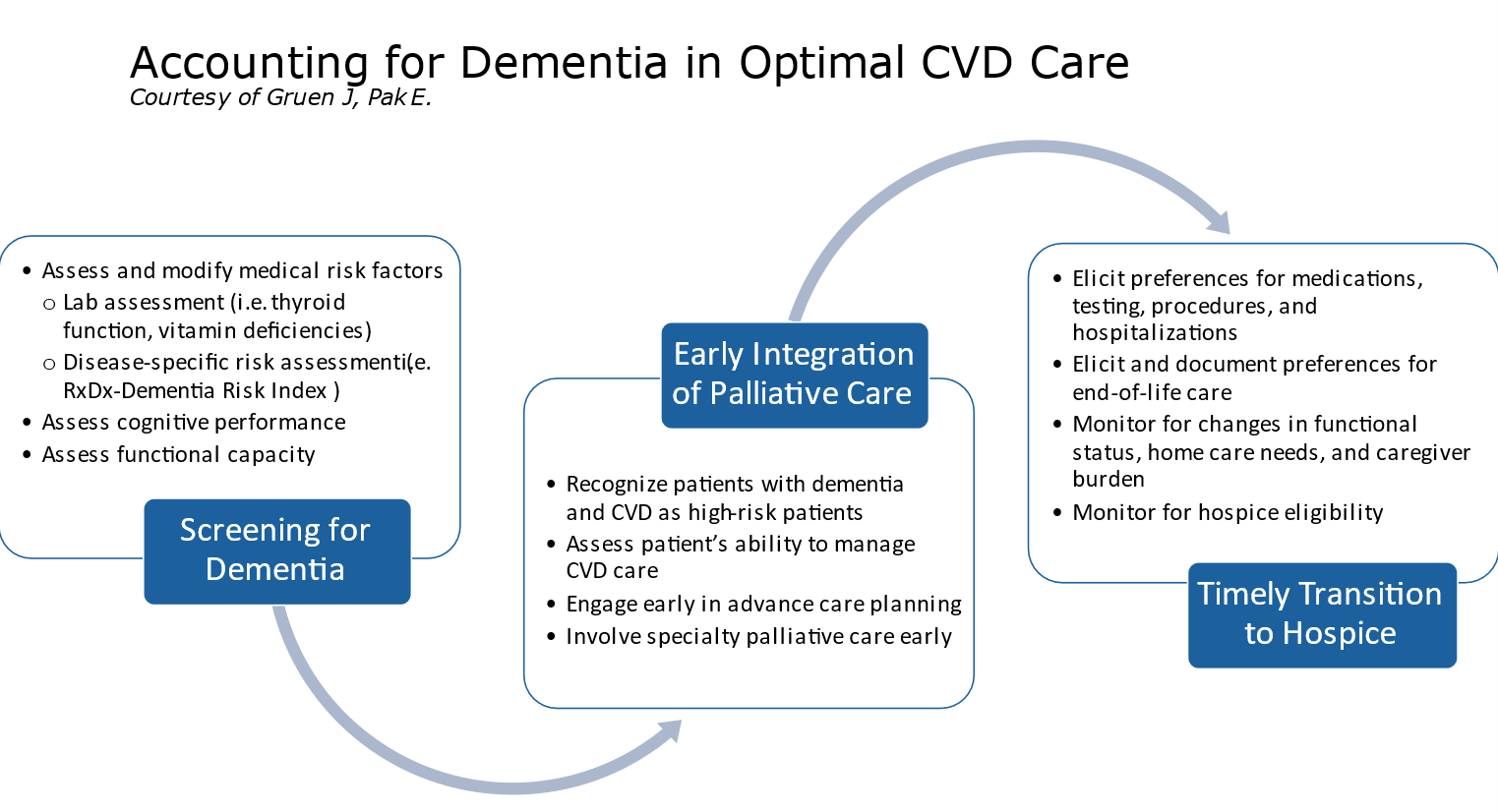
- We propose guidance on early screening and referral to specialty palliative care as a part of routine assessment of patients with CVD (Figure 1). There are no risk scores specific to CVD, though the RxDx-Dementia Risk Index has been established for patients with hypertension and type 2 diabetes.5
- While there exist numerous predictive models for patients with dementia and comorbidities, most lack external validity and economic impact.6 Future research may target the development of better tools to screen and prognosticate for dementia in patients with heart disease.
Figure 1
Commentary based on Lackraj D, Kavalieratos D, Murali KP, Lu Y, Hua M. Implementation of specialist palliative care and outcomes for hospitalized patients with dementia. J Am Geriatr Soc 2021;69:1199-1207.7
Background
- Dementia is a chronic, progressive illness that affects millions of adults. Despite uncertain benefit, one in four patients with dementia are hospitalized in the last 30 days of life.8
- Palliative care is specialized medical care for people living with serious illness and aims to provide support for patients and their caregivers.
- Primary palliative care includes basic symptom management and shared decision-making, and it is delivered by primary providers (i.e. hospitalists, emergency room clinicians, neurologists, and cardiologists).
- Specialty palliative care may be necessary to navigate challenging ethical, social, and symptomatic concerns, and it is delivered by practitioners with specialized training in palliative medicine and hospice.
- The use of palliative care in patients with dementia has not been widely studied, but limited literature suggests that specialty palliative care may increase advance care planning and referrals to hospice.9 The goal of the present study was to examine whether the implementation of hospital-based specialty palliative care programs impacted outcomes for hospitalized patients with dementia.
Exposure and Outcomes
- The primary exposure was the implementation of a hospital-based specialist palliative care program in New York state hospitals between 2008 and 2014. Hospitals with a palliative care program through the entire study period were excluded.
- The authors chose a hospital-level exposure to palliative care specialists due to challenges in accurately determining patient-level palliative care use in United States registries.
- The study population included patients with a diagnosis of dementia who were hospitalized in New York state between 2008-2014. Dementia diagnosis was based on ICD-9 codes and data were collected from the New York Statewide Planning and Research Cooperative System (SPARCS).
- The primary outcome was discharge to hospice (home or inpatient). Hospice was chosen as the primary outcome because it was available in population-level data and it was likely affected by a specialty palliative care intervention.
- Secondary outcomes included hospital length of stay, use of mechanical ventilation, use of dialysis, and days in the intensive care unit.
Results
- A palliative care program was implemented in 24 hospitals and not implemented in 29 hospitals. There were 82,068 patients with dementia hospitalized. A slight majority of these patients were admitted to a hospital that implemented a palliative care program (n=41,227) compared to a hospital that did not (n=40,841).
- Discharge to hospice for patients with dementia only occurred for 5.1% of patients. Using difference-in-difference analysis, patients in hospitals that implemented a palliative care program were 35% more likely to be discharged to hospice after implementation of a palliative care program (adjusted odds ratio = 1.35 (1.19-1.51), p < .001).
- When stratified by teaching and nonteaching hospital, patients with dementia who received care at teaching hospitals were 74% more likely to be discharged to hospice (odds ratio = 1.74 (1.49-1.99), p < .001). This association was not seen in nonteaching hospitals.
- There was no statistical significance in any secondary outcomes, except there was an increased length of stay after implementation of a palliative care program that was not clinically meaningful.
Conclusions
- Hospitalized patients with dementia were more likely to be discharged to hospice if they were admitted to a hospital with specialized palliative care. The primary outcome was seen only in teaching hospitals, which points to the heterogeneity in palliative care referral in different care centers. These data suggest that palliative care programs may impact outcomes for patients with dementia, though this effect likely depends on hospital-specific characteristics.
- The study highlights the relative paucity of hospice referrals for patients with dementia and the need to better understand how palliative care should be implemented in chronic illness. Challenges to hospice referral include prognostic uncertainty and unpredictable disease trajectory.2 Acute hospitalizations may be important opportunities to involve palliative care for patients with chronic, progressive diseases like dementia.
- A major limitation of this study was the inference of palliative care utilization based on program availability instead of patient-specific referrals. The authors also included a wide range of dementia diagnoses based on coding, and there was no way to elucidate whether these diagnoses directly contributed to the hospitalization or hospice referral. Finally, there was likely heterogeneity in the implemented palliative care programs, which was not described.
References
- Santos CY, Snyder PJ, Wu WC, Zhang M, Echeverria A, Alber J. Pathophysiologic relationship between Alzheimer's disease, cerebrovascular disease, and cardiovascular risk: a review and synthesis. Alzheimers Dement (Anist) 2017;7:69-87.
- Erel M, Marcus EL, Dekeyser-Ganz F. Barriers to palliative care for advanced dementia: a scoping review. Ann Palliat Med 2017;6:365-79.
- Warraich HJ, Xu H, DeVore AD, et al. Trends in hospice discharge and relative outcomes among Medicare patients in the Get with The Guidelines–Heart Failure Registry. JAMA Cardiol 2018;3:917-26.
- Patel B, Secheresiu P, Shah M, et al. Trends and predictors of palliative care referrals in patients with acute heart failure. Am J Hosp Palliat Care 2019;35:147-53.
- Mehta HB, Mehta V, Tsai CL, Cheun H, Aparasu RR, Johnson ML. Development and validation of the RxDx-Dementia Risk Index to predict dementia in patients with type 2 diabetes and hypertension. J Alzheimers Dis 2016;49:423-32.
- Stephan BCM, Tang E, Muniz-Terrera G. Composite risk scores for predicting dementia. Curr Opin Psychiatry 2016;29:174-80.
- Lackraj D, Kavalieratos D, Murali KP, Lu Y, Hua M. Implementation of specialist palliative care and outcomes for hospitalized patients with dementia. J Am Geriatr Soc 2021;69:1199-1207.
- Teno JM, Keohane LM, Mitchell SL, et al. Dying with dementia in Medicare Advantage, Accountable Care Organizations, or traditional Medicare. J Am Geriatr Soc 2021;May 14:[Epub ahead of print].
- Hanson LC, Kistler CE, Lavin K, et al. Triggered palliative care for late-stage dementia: a pilot randomized trial. J Pain Symptom Manage 2019;57:10-19.
Clinical Topics: Geriatric Cardiology, Prevention, Hypertension, Sleep Apnea
Keywords: Geriatrics, Aged, Patient Discharge, Palliative Care, Hospices, Palliative Medicine, Caregivers, Inpatients, Cardiovascular Diseases, Prevalence, Respiration, Artificial, International Classification of Diseases, Hospitals, State, Diabetes Mellitus, Type 2, Length of Stay, Decision Making, Shared, Renal Dialysis, Advance Care Planning, Intensive Care Units, Heart Diseases, Hypertension, Hospitals, Teaching, Cognitive Dysfunction, Registries, Dementia, Emergency Service, Hospital
< Back to Listings