Current and Emerging Strategies for RV Shock Management in the Setting of RV Infarct
Quick Takes
- Right ventricle (RV) failure is associated with increased morbidity and mortality across a spectrum of cardiovascular conditions including cardiogenic shock.
- Multiple hemodynamic parameters along with cardiac imaging can assist in the diagnoses of RV failure.
- RV - mechanical circulatory support (MCS) devices have demonstrated improvements in hemodynamics along with safety and feasibility of their use.
Determinants of Right Ventricle Function
Right Ventricle (RV) function is influenced by venous return, pulmonary pressures, myocardial contractility, and pericardial compliance.1 Unlike the left ventricle (LV) which is more adapted to maintaining stroke volume despite increases in afterload and systemic vascular resistance, the RV is particularly sensitive to increases in afterload as it typically pumps against the low resistance of the pulmonary system.
Ischemia and LV failure can lead to RV failure by decreasing stroke volume and increasing RV afterload through pulmonary vasoconstriction and edema.2 Myocardial infarction (MI) can also affect RV function by decreasing contractility of the RV free wall or interventricular septum. Injury to the RV free wall typically occurs secondary to occlusion of a RV marginal branch. Injury to the interventricular septum dysfunction is more common and typically occurs secondary to occlusion of a dominant right coronary or circumflex artery which perfuses about one-third of the interventricular septum, or occlusion of a left anterior descending artery which perfuses two-thirds of the interventricular septum.
Consequence of RV Failure
RV failure can result in RV dilatation causing leftward displacement of the interventricular septum, creating the classic 'D-shaped' septum. In this setting, patients develop worsening diastolic heart failure, impairing LV stroke volume, which can precipitate hemodynamic collapse.
RV dilation can also result in tricuspid regurgitation, increasing venous congestion and activation of neurohumoral signaling. Venous congestion significantly affects the hepatic and renal systems and can lead to multi-system organ failure.
Defining RV Failure
Multiple invasive hemodynamic variables can help to define RV failure and should be taken into context along with the clinical history, physical examination, and echocardiographic indices. In an acute setting such as an MI, RV dysfunction can be suggested by a central venous pressure (CVP) >12 mmHg, CVP:PCWP ratio >0.8 (which has been correlated to cardiac necrosis), pulmonary artery pulsatility index (PAPI) <1, and RV stroke index (RVSI) <300 g/m2/beat.3,4 Unfortunately invasive hemodynamics continue to be underutilized, as less than 20% of patients in cardiogenic shock receive such measures.
The identification of diastolic suction alarms can also be suggestive of RV failure. These alarms are triggered when univentricular left sided support devices are used in the setting of unidentified RV dysfunction, leading to decreased LV preload. If these alarms become frequent, clinicians should consider performing more definitive evaluation of RV function with an echocardiogram or invasive hemodynamics.5
Initial Management of RV Failure
Management of patients with RV dysfunction involves immediate optimization of preload. For acute presentations, patients typically have low blood volume and will respond to fluid resuscitation. Patients with a subacute or chronic presentation are typically fluid overloaded and respond to diuresis.
Inotropes like dobutamine and milrinone can be utilized to assist with contractility. Although, they should be used with caution in patients with acute MI as these agents increase myocardial oxygen demand and arrhythmogenicity.
Concomitant brady-arrhythmias are commonly seen in these patients, and often warrant pacing. In addition to these interventions, it remains essential that there is early and optimized revascularization.
RV Mechanical Circulatory Support Devices
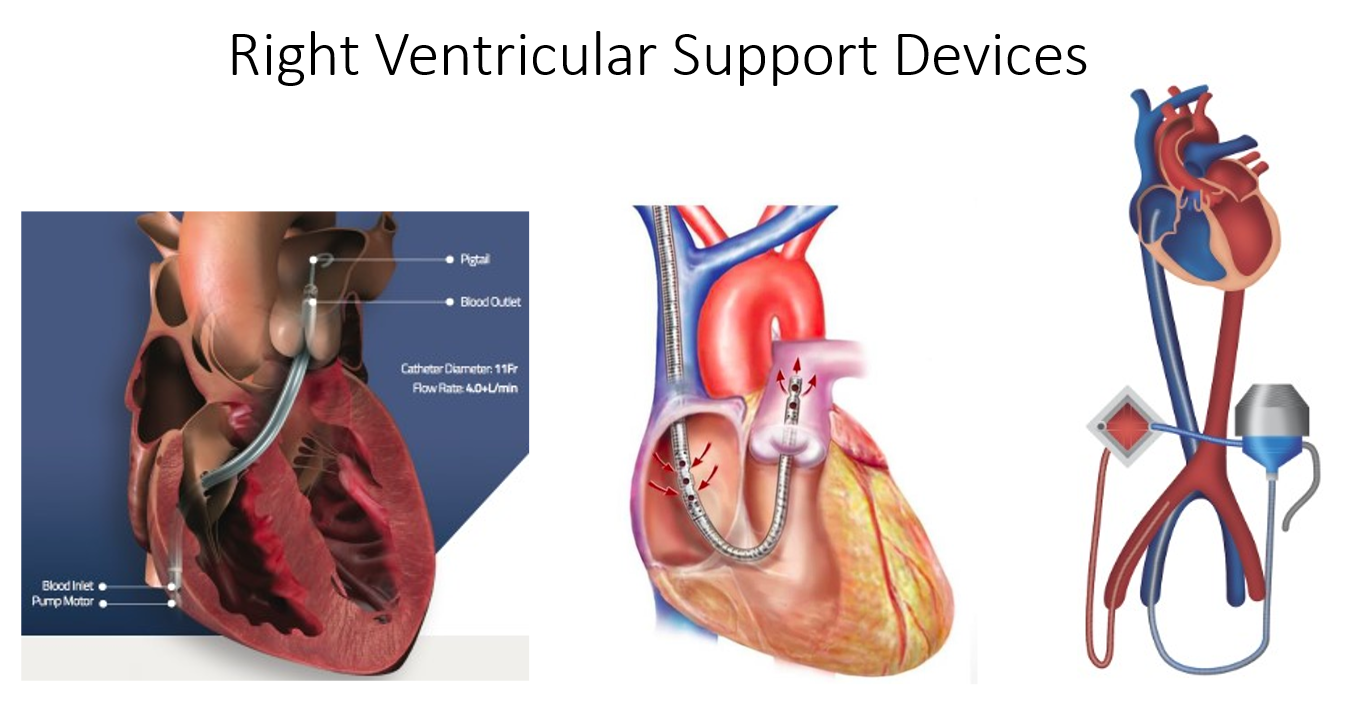
There are three commercially available percutaneous RV MCS devices (Figure 1) that are commonly used; RV Impella®, ProtekDuo TandemHeart, and Veno-Arterial Extracorporeal Membrane Oxygenation (VA-ECMO).
Figure 1: Courtesy of Salam MF, Gorgis S, Basir MB.
The RV Impella® is inserted through the femoral venous system via a 22-F sheath. It has an inlet port in the right atrium-inferior vena cava junction; blood is then displaced by a small impeller through the outflow cannula in the pulmonary artery. The device does not have an oxygenator and provides up to 5 L/min of flow.
The ProtekDuo TandemHeart is a 29- to 31-F device placed in the internal jugular vein. It is a dual lumen catheter that extracts blood from the right atrium, sends it through a centrifugal pump to the outflow cannula in the pulmonary artery. The circuit can be attached to an oxygenator and provides up to 5L/min of flow.
VA-ECMO can be inserted peripherally using a 15-19F arterial access and 21-29F venous access. VA-ECMO bypasses the RV, displacing 4 to 6 L/min of blood from the right atrium into the iliofemoral arterial system through a centrifugal pump and oxygenator. VA-ECMO requires trained nursing or perfusion teams as well as the need for large bore arterial access.
The data supporting these devices are small in number, primarily observational, and associated with varying outcomes as the studies have included a heterogeneous cohort of patients.6-8 The studies however do demonstrate overall improvement of hemodynamics and feasibility and safety of the use of such devices with expert teams and personnel.9
References
- Konstam M, Kiernan MS, Bernstein D, et al. Evaluation and management of right-sided heart failure: a scientific statement from the American Heart Association. Circulation 2018;137:e578-e622.
- Kapur NK, Esposito ML, Bader Y, et al. Mechanical circulatory support devices for acute right ventricular failure. Circulation 2017;136:314-26.
- Lala A, Guo Y, Xu J, et al. Right ventricular dysfunction in acute myocardial infarction complicated by cardiogenic shock: a hemodynamic analysis of the should we emergently revascularize occluded coronaries for cardiogenic shock (SHOCK) trial and registry. J Card Fail 2018;24:148-56.
- Korabathina R, Heffernan KS, Paruchuri V, et al. The pulmonary artery pulsatility index identifies severe right ventricular dysfunction in acute inferior myocardial infarction. Catheter Cardiovasc Interv 2012;80:593-600.
- Basir MB, Gorgis S, Lemor A, et al. TCT CONNECT-176 Diastolic suction alarms are an early marker for right ventricular failure in the setting of left ventricular mechanical circulatory support. J Am Coll Cardiol 202;76:b76.
- Salna M, Garan AR, Kirtane AJ, et al. Novel percutaneous dual-lumen cannula-based right ventricular assist device provides effective support for refractory right ventricular failure after left ventricular assist device implantation. Interact Cardiovasc Thorac Surg 2020;30:499-506.
- Kuchibhotla S, Esposito ML, Breton C, et al. Acute biventricular mechanical circulatory support for cardiogenic shock. J Am Heart Assoc 2017;6:e006670.
- Djordjevic I, Eghbalzadeh K, Sabashnikov A, et al. Single center experience with patients on veno arterial ECMO due to postcardiotomy right ventricular failure. J Card Surg 2020;35:83-88.
- Basir MB, Kapur NK, Patel K, et al. Improved outcomes associated with the use of shock protocols: updates from the National Cardiogenic Shock Initiative. Catheter Cardiovasc Interv 2019;93:1173-83.
Clinical Topics: Arrhythmias and Clinical EP, Cardiovascular Care Team, Heart Failure and Cardiomyopathies, Noninvasive Imaging, Vascular Medicine, Implantable Devices, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Acute Heart Failure, Chronic Heart Failure, Echocardiography/Ultrasound, Acute Coronary Syndromes
Keywords: Heart Ventricles, Milrinone, Dobutamine, Extracorporeal Membrane Oxygenation, Dilatation, Pulmonary Artery, Stroke Volume, Shock, Cardiogenic, Tricuspid Valve Insufficiency, Central Venous Pressure, Heart Failure, Diastolic, Vasoconstriction, Hyperemia, Jugular Veins, Vena Cava, Inferior, Cannula, Feasibility Studies, Echocardiography, Vascular Resistance, Heart Atria, Perfusion, Arrhythmias, Cardiac, Oxygenators, Blood Volume, Edema, Physical Examination, Diuresis, Stroke, Oxygen
< Back to Listings