The Effect of Statin Therapy on the Progression and Composition of Coronary Atherosclerotic Plaque Identified on Coronary CTA
Quick Takes
- Coronary CTA has improved clinicians' ability to treat patients with coronary artery disease.
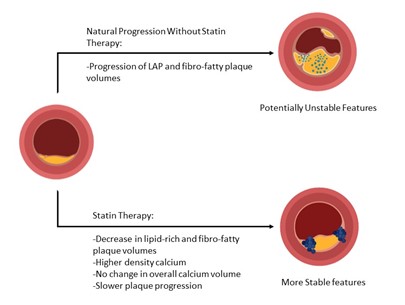
- Statin therapy is associated with reduced plaque progression, decrease in MACE, but increase in coronary calcium score.
- Statin therapy is associated with alteration in coronary plaque features, namely higher calcium density and lower low-attenuation and fibro-fatty plaque volumes.
- Higher calcium density is associated with slower plaque progression.
Commentary based on: van Rosendael AR, van den Hoogen IJ, Gianni U, et al. Association of statin treatment with progression of coronary atherosclerotic plaque composition. JAMA Cardiol 2021;6:1257-66.
Introduction
Coronary artery disease (CAD) is highly prevalent and if inadequately treated can often lead to major adverse cardiovascular events (MACE).1 Treatment begins with aggressive lifestyle and behavioral modifications, but often requires pharmacologic therapy with statin therapy for appropriate risk factor control in those with elevated atherosclerotic cardiovascular disease (ASCVD) risk. Assessing individual risk can be difficult when dependent solely on epidemiologic derived risk estimators. Direct visualization of CAD by coronary computed tomography angiography (CCTA) provides high diagnostic accuracy comparable to the reference standard of invasive coronary angiography (ICA).
CCTA has improved clinicians' ability to treat patients with CAD by identifying patients with at least mild coronary atherosclerotic disease; this may result in earlier implementation of treatment to reduce ASCVD risk with pharmacotherapy. More detailed plaque characterization may allow for further risk stratification and personalized management recommendations.
Statin therapy leads to reduced plaque progression, likely representing a central mechanism for its favorable clinical effect. Counterintuitively, however, coronary calcium scores continue to increase with statin therapy but probably at a slower rate.2 Furthermore, the presence of very dense calcium (>1000 Hounsfield units, or 1K) seems to be associated with lower rates of major events for a specific plaque.3,4 Therefore, delineating the effects of statin therapy on plaque composition may help guide risk estimation and management decisions for patients with CAD.
Statin Therapy and Atherosclerotic Plaque Composition
In a recent issue of JAMA Cardiology, van Rosendael et al. studied the association of statin therapy with progression of coronary plaque composition. Importantly, coronary artery plaque burden predicts risk of MACE. Specific plaque features identified via coronary CTA are risk factors for coronary events. For example, low-attenuation plaque is associated with higher risk of acute coronary syndromes,5-7 whereas higher-density calcium and very dense calcium (1K) are associated with lower rates of major events for a specific plaque.3,4
To better understand the changes associated with statin therapy on certain plaque subtypes, the authors enrolled 2,252 patients from the CCTA PARADIGM study. These patients had suspected or known CAD and underwent serial CCTA 2 or more years apart between 2013 to 2016 across seven countries; 857 patients were included in this analysis.
The study excluded patients with noninterpretable CCTA findings, patients without lesions at baseline as well as at follow-up, patients initiating or stopping statin after baseline CCTA, patients with unknown information regarding statin use, and those with tandem lesions at baseline that were confluent at follow-up. A total of 2,458 coronary lesions were assessed.
CCTA evaluated all coronary arteries, including side branches that were at least 2 mm in diameter. Using fixed Hounsfield units, coronary lesions were categorized by plaque volumes and calcium composition as low-attenuation plaque, fibro-fatty plaque, fibrous plaque, low-density calcium, high-density calcium, and very densely calcified 1K plaque. The statistical model was adjusted for age, sex, diabetes, hypertension, smoking status, body mass index, and the CT interval.
Statin therapy was associated with lower low-density cholesterol levels in patients treated with statins at follow-up (88 vs. 110 mg/dL, p < 0.001). In patients not on a statin, low-attenuation and fibro-fatty plaque volumes increased over time. In patients on a statin, coronary lesions had a lower volume of low-attenuation plaques and a higher volume of calcium-containing plaques.
Statin therapy was also associated with larger decreases in volume of low-attenuation plaques and fibro-fatty plaques as well as larger increases in volumes of high-density calcium and 1K plaques without being associated with change in overall calcium volume. The progression of higher-density calcification was greater in statin-treated patients. Increasing plaque calcium density was associated with lower proportion of low-attenuation plaque, fibro-fatty plaque, and fibrous plaque.
In both statin and non-statin treated patients, lesions with a higher calcium proportion displayed less plaque progression; the least progression was observed in the very densely calcified plaque. This was especially evident in the statin group, where smaller plaque progression was observed for both high-density and very densely calcified plaques, as opposed to the non-statin group, in which smaller plaque progression only occurred in the very densely calcified plaques.
Discussion
This study confirmed the notion of statin therapy as a key intervention in stabilization atherosclerotic disease. Macroscopic calcification is uncommon in the early stages of atherosclerosis while its invariable presence during its later stages likely is related to decreasing inflammation and organization. Statin therapy appears to accelerate the process of transforming a potentially highly metabolically active plaque to a more inert state. Specifically, statin therapy is associated with a decrease in low-attenuation and fibro-fatty plaque volumes and an increase in high-density and 1K volumes. Higher calcium density is associated with slowed plaque progression.
The progression of atherosclerotic plaque composition has been previously described with intravascular ultrasound and CCTA. Using these modalities, it was noted that statin therapy is associated with a decrease in lipid-rich plaque and an increase in calcification. Pathologically, free calcium is released from dying macrophages and smooth muscle cells crystalize into microcalcifications in the deeper necrotic core, and later coalesce and form denser calcium sheets.8
The ability to study the progression of plaque and the specific effects on the composition of atherosclerotic plaques with various therapies, specifically statin therapy in CCTA PARADIGM, may further increase the utility of CCTA in the management of coronary artery disease. This data supports results previously reported in the ICONIC study, which showed that coronary plaque in patients with acute coronary syndrome had larger volume of noncalcified components, possibly reflecting an earlier, more active stage of atherosclerosis.5 Conversely, data from MESA and ICONIC revealed higher plaque calcium density in patients with lower risk of cardiac events.3,4 It is conceivable that the presence of high-density calcium sheets implies that plaque naturally progressed to a more stable form.
This present analysis supports findings from the above literature, i.e., suggesting a role of statin therapy in accelerating plaque transformation from noncalcified to calcified content and thus aiding plaque stabilization. Study limitations include the observational study design, lack of statin dosing information, and potential selection bias.
Conclusion
Statin therapy is associated with atherosclerotic plaque transformation to higher calcium density, which is associated with slower plaque progression.
Figure 1: Courtesy of Kazzi BE, Feldman DI, Blumenthal RS, Zadeh AA.
References
- Min JK, Dunning A, Lin FY, et al. Age- and sex-related differences in all-cause mortality risk based on coronary computed tomography angiography findings results from the International Multicenter CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter Registry) of 23,854 patients without known coronary artery disease. J Am Coll Cardiol 2011;58:849-60.
- Henein M, Granåsen G, Wiklund U, et al. High dose and long-term statin therapy accelerate coronary artery calcification. Int J Cardiol 2015;184:581-86.
- Criqui MH, Denenberg JO, Ix JH, et al. Calcium density of coronary artery plaque and risk of incident cardiovascular events. JAMA 2014;311:271-78.
- van Rosendael AR, Narula J, Lin FY, et al. Association of high-density calcified 1K plaque with risk of acute coronary syndrome. JAMA Cardiol 2020;5:282-90.
- Chang HJ, Lin FY, Lee SE, et al. Coronary atherosclerotic precursors of acute coronary syndromes. J Am Coll Cardiol 2018;71:2511-22.
- Motoyama S, Ito H, Sarai M, et al. Plaque characterization by coronary computed tomography angiography and the likelihood of acute coronary events in mid-term follow-up. J Am Coll Cardiol 2015;66:337-46.
- Williams MC, Kwiecinski J, Doris M, et al. Low-attenuation noncalcified plaque on coronary computed tomography angiography predicts myocardial infarction: results from the multicenter SCOT-HEART trial (Scottish Computed Tomography of the HEART). Circulation 2020;141:1452-62.
- Otsuka F, Joner M, Prati F, Virmani R, Narula J. Clinical classification of plaque morphology in coronary disease. Nat Rev Cardiol 2014;11:379-89.
Clinical Topics: Acute Coronary Syndromes, Cardiovascular Care Team, Dyslipidemia, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Prevention, Atherosclerotic Disease (CAD/PAD), Lipid Metabolism, Nonstatins, Novel Agents, Statins, Interventions and ACS, Interventions and Coronary Artery Disease, Interventions and Imaging, Angiography, Computed Tomography, Echocardiography/Ultrasound, Nuclear Imaging, Hypertension
Keywords: Hydroxymethylglutaryl-CoA Reductase Inhibitors, Plaque, Atherosclerotic, Acute Coronary Syndrome, Calcium, Coronary Artery Disease, Coronary Angiography, Computed Tomography Angiography, Body Mass Index, Selection Bias, Cardiovascular Diseases, Follow-Up Studies, Calcinosis, Ultrasonography, Atherosclerosis, Models, Statistical, Diabetes Mellitus, Risk Factors, Hypertension, Myocytes, Smooth Muscle, Cardiology, Life Style, Inflammation, Macrophages, Ultrasonography, Interventional, Risk Assessment, Lipids, Reference Standards, Cholesterol
< Back to Listings