Social Vulnerability Index Highlights the Most Vulnerable Among US to Cardiovascular Disease
Quick Takes
- In the United States (and globally), cardiovascular disease (CVD) continues to be the leading cause of mortality.
- US counties with higher social vulnerability have greater rates of premature CVD mortality, and this relationship was "dose" dependent.
- This study highlights particular subsets of the population especially susceptible to premature CVD mortality in vulnerable communities: non-Hispanic Black residents, women, and residents in rural areas.
BACKGROUND AND STUDY PREMISE
The link between adverse social determinants of health (SDOH) and adverse health outcomes has been highlighted during the COVID-19 pandemic. The wide media coverage and discussion of racial and ethnic disparities in COVID-19 mortality have prompted research efforts towards more effectively identifying susceptible populations. United States (US) counties with the greatest social vulnerabilities were more prone to become COVID-19 hotspots.1,2 This effect was exacerbated in rural areas and counties with a higher proportion of residents from racial and ethnic minorities. Greater SDOH burden has also been associated with lower adherence to COVID-19 risk-limiting practices.3
The Centers for Disease Control (CDC) and Prevention/Agency for Toxic Substances and Disease Registry (ATSDR) Social Vulnerability Index (SVI) was developed as a resource to aid emergency response planners and public health officials map communities that will most likely need support before, during, and after a hazardous event including natural disasters, disease outbreaks, or hazardous chemical exposures.4 The CDC-ATSDR SVI assesses the vulnerability of every US census tract to public health emergencies by ranking them on 15 social factors grouped into four related themes: 1) socioeconomic status, 2) household composition and disability, 3) minority status and language, and 4) housing type and transportation.
Despite the current focus placed on the COVID-19 pandemic, cardiovascular disease (CVD) remains the leading cause of mortality globally.5 The rate of premature CVD mortality in the US is increasing and CVD remains a significant cause of death in working age Americans.5,6
METHODS
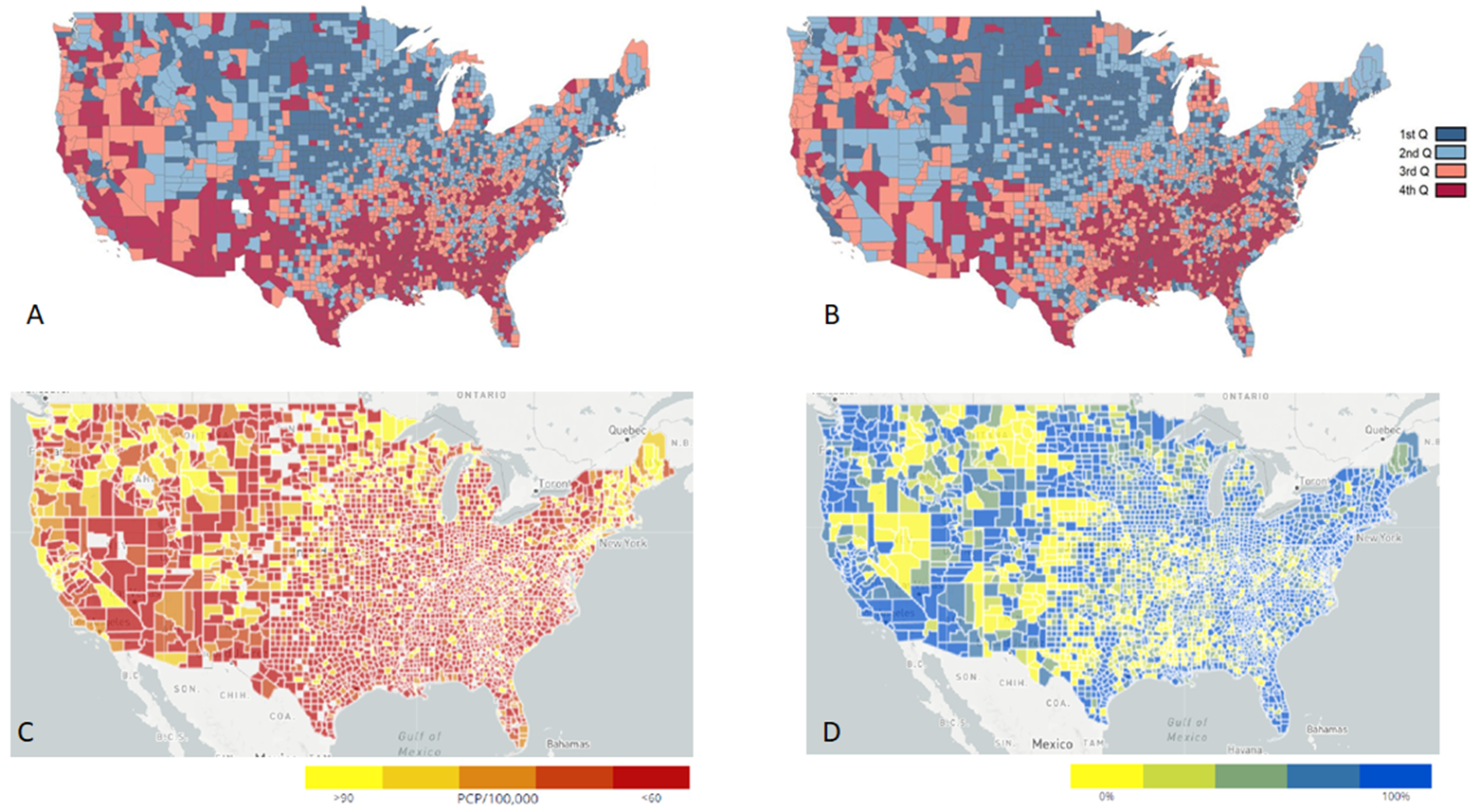
Khan et al. performed a comparison of SVI and CVD mortality data from CDC Wide-Ranging Online Data for Epidemiological Research (WONDER) at the US county level.6,7 Counties were ranked by SVI into quartiles and this was compared to overall CVD mortality and CVD subtype (ischemic heart disease, stroke, hypertension, and heart failure) mortality for adults <65 years old.
RESULTS
The study demonstrated that US counties with higher social vulnerability have greater rates of premature CVD mortality. This relationship was "dose" dependent: age adjusted mortality rates for CVD and CVD subtypes (ischemic heart disease, stroke, hypertension, and heart failure) increased with increasing SVI quartile.
Interestingly, the CVD mortality rate ratio between the fourth SVI quartile (most vulnerable) and first SVI quartile (least vulnerable) varied by sex, race, and county type. Women living in the most vulnerable counties had two-fold higher rate of CVD mortality when compared to those in the least vulnerable counties. Non-Hispanic Black residents of the most vulnerable counties had higher relative risk of stroke and heart failure mortality than those in the least vulnerable counties. Residents of rural counties with significant social vulnerabilities had two- to five-fold higher CVD and CVD subtype mortality rates compared to the residents of the least vulnerable rural counties.
DISCUSSION
This study clearly demonstrates the connection between SDOH and health outcomes. Khan et al. highlight subgroups of the population where public health workers could prioritize resource allocation to improve community health. This information could be applied to better target future interventions and studies to improve health disparities.
For Black Americans and women, the effects of structural racism and gender inequality have had longstanding negative implications on wages, access to education, educational attainment, and financial stability. These factors have been linked to poorer health outcomes in both subpopulations.8,9 For rural American residents, reduced access to healthcare infrastructure, limited public health interfacing, neighborhood disadvantage, and differences in demographics all predispose underserved individuals to adverse CVD outcomes.10-12
Khan et al. suggest placing more emphasis on the implementation of population and community wide interventions. They also suggest that in-person visits be preferred as compared to telehealth for social and health assessments due to 5-7% of the US population lacking reliable access to broadband internet.13,14
Expansion of Medicaid to include nonelderly adults facing adverse social circumstances may narrow health disparities. States that have expanded Medicare under the Affordable Care Act have had reduced cardiovascular mortality more than non-expansion states.15 Notably, 8 of the 12 states that have not opted to expand Medicaid are located in regions of the US highlighted as socially vulnerable by Khan et al.6
In addition to expanding healthcare coverage, efforts to improve infrastructure in socially vulnerable communities are necessary to reduce CVD disparities. Neighborhood socioeconomic status, access to grocery stores, walkability, and access to areas for physical activities are associated with better cardiovascular health.6,16 Healthcare policymakers should place emphasis on ensuring access to healthy foods, green spaces, exercise facilities, and exercise equipment. For rural communities, efforts should be made to increase the availability of both primary care and subspecialty health care providers, and access to public health programs.
While public health campaigns have reduced overall CVD mortality, the decline in CVD death rates has slowed since 2010.6,17,18 Notably, the rate of premature CVD mortality in US continues to increase.5,6 This study performed by Khan et al. emphasizes the role of SDOH in health outcomes and specific subpopulations and regions more vulnerable to premature CVD mortality. This information can inform future policies to better allocate resources and more effectively implement public health efforts. If we fail to adequately address SDOH with future healthcare policies and practices, we could lose the previously achieved gains in CVD prevention.
Figure 1
References
- Neelon B, Mutiso F, Mueller NT, Pearce JL, Benjamin-Neelon SE. Spatial and temporal trends in social vulnerability and COVID-19 incidence and death rates in the United States. PLoS One 2021;16:e0248702.
- Freese KE, Vega A, Lawrence JJ, Documet PI. Social vulnerability is associated with risk of COVID-19 related mortality in U.S. counties with confirmed cases. J Health Care Poor Underserved 2021;32:245-57.
- Hagan KK, Javed Z, Cainzos-Achirica M, et al. Social determinants of adherence to COVID-19 risk mitigation neasures among adults with cardiovascular disease. Circ Cardiovasc Qual Outcomes 2021;14:690-700.
- CDC/ATSDR Social Vulnerability Index (Agency for Toxic Substances and Disease Registry website). 2021. Available at: https://www.atsdr.cdc.gov/placeandhealth/svi/index.html. Accessed 11/20/2021.
- Virani SS, Alonso A, Aparicio HJ, et al. Heart disease and stroke statistics—2021 Update. Circulation 2021;143:e254-e743.
- Gangavelli A, Morris AA. Premature cardiovascular mortality in the United States: who will protect the most vulnerable among us? Circulation 2021;144:1280-83.
- Khan SU, Javed Z, Lone AN, et al. Social vulnerability and premature cardiovascular mortality among US counties, 2014 to 2018. Circulation 2021;144:1272-79.
- Nayak A, Hicks AJ, Morris AA. Understanding the complexity of heart failure risk and treatment in African Americans. Circ Heart Fail 2020;Aug 13:[Epub ahead of print].
- Shaw LJ, Pepine CJ, Xie J, et al. Quality and equitable health care gaps for women: attributions to sex differences in cardiovascular medicine. J Am Coll Cardiol 2017;70:373-88.
- Cross SH, Mehra MR, Bhatt DL, et al. Rural-urban differences in cardiovascular mortality in the US, 1999-2017. JAMA 2020;323:1852-54.
- Cross SH, Califf RM, Warraich HJ. Rural-urban disparity in mortality in the US From 1999 to 2019. JAMA 2021;325:2312-14.
- Shiels MS, Berrington de González A, Best AF, et al. Premature mortality from all causes and drug poisonings in the USA according to socioeconomic status and rurality: an analysis of death certificate data by county from 2000-15. Lancet Public Health 2019;4:e97-e106.
- Perrin A, Atske S. 7% of Americans don't use the internet. Who are they? (pewresearch.org). 2021. Available at: https://www.pewresearch.org/fact-tank/2021/04/02/7-of-americans-dont-use-the-internet-who-are-they/. Accessed 11/20/2021.
- Connect2HealthFCC - Mapping Broadband Health in America 2017 (fcc.gov). 2017. Available at: https://www.fcc.gov/reports-research/maps/connect2health/#ll=40.042098,-94.962764&z=4&t=insights
&inb=in_bb_access&inh=in_diabetes_rate&dmf=none&inc=none&slb=90,100&slh=10,22. Accessed 11/20/2021. - Khatana SAM, Bhatla A, Nathan AS, et al. Association of Medicaid expansion with cardiovascular mortality. JAMA Cardiol 2019;4:671-79.
- Unger E, Diez-Roux AV, Lloyd-Jones DM, et al. Association of neighborhood characteristics with cardiovascular health in the multi-ethnic study of atherosclerosis. Circ Cardiovasc Qual Outcomes 2014;7:524-31.
- Sidney S, Quesenberry CP Jr, Jaffe MG, et al. Recent trends in cardiovascular mortality in the United States and public health goals. JAMA Cardiol 2016;1:594-99.
- Ma J, Ward EM, Siegel RL, Jemal A. Temporal trends in mortality in the United States, 1969-2013. JAMA 2015;314:1731-39.
Clinical Topics: Cardiovascular Care Team, COVID-19 Hub, Diabetes and Cardiometabolic Disease, Heart Failure and Cardiomyopathies, Prevention, Acute Heart Failure, Exercise, Hypertension, Dyslipidemia
Keywords: Patient Protection and Affordable Care Act, COVID-19, SARS-CoV-2, Cardiovascular Diseases, Medicaid, Rural Population, Emergencies, Risk, Housing, African Americans, Racism, Hazardous Substances, Cause of Death, Social Determinants of Health, Social Factors, Parks, Recreational, Medicare, Exercise, Social Class, Hypertension, Telemedicine, Myocardial Ischemia, Heart Failure, Heart Failure, Health Promotion, Delivery of Health Care, Health Policy, Primary Health Care, Centers for Disease Control and Prevention, U.S., Resource Allocation, Registries, Stroke, Health Personnel, Disease Outbreaks, Outcome Assessment, Health Care
< Back to Listings