Peri-Operative Risk Scores in Adult Congenital Heart Disease: 10 Points to Remember
This 10-point compilation serves as an introduction to peri-operative risk scoring for adults with congenital heart disease, based on the PErioperative ACHd (PEACH) score described in the manuscript Enhanced Assessment of Perioperative Mortality Risk in Adults with Congenital Heart Disease.1
- In developed countries, adults with congenital heart disease (ACHD) now outnumber children, with an increasing proportion of patients with complex anatomy.2,3
- ACHD patients may have residual or progressive hemodynamic lesions and, therefore, may require re-intervention. Their care requires high levels of surgical and medical expertise.
- Peri-operative risk in ACHD is related to sudden events including arrhythmia, ventricular dysfunction, bleeding (increased frequency in the presence of adhesions during re-sternotomy or collateral vessels), difficult venous or arterial access and anesthesia in patients with pulmonary vascular disease or univentricular physiology.
- Peri-operative risk factors in ACHD may be patient (genetics and other clinical characteristics including the number of re-sternotomies) or procedure-dependent (complexity, urgency, or the need to perform other procedures). For example, in the Society of Thoracic Surgeons Congenital Heart Surgery Database (STS-CHSD), elective secundum atrial septal defect repair carried a 0.3% mortality risk while Fontan revision surgery was associated with a 9.4% mortality.4,5
- Reliable peri-operative risk scoring is useful to (a) inform consent, (b) optimize potentially modifiable risk factors (e.g., pharmacotherapy for heart failure, iron replacement or blood transfusion for anemia), (c) allow adequate surgical planning e.g., the use of peri-operative extra-corporeal membrane oxygenation (ECMO), and (d) consider reoperation versus heart or heart-lung transplantation.
- In patients at increased peri-operative risk, percutaneous transcatheter options may be an attractive alternative, as they are less invasive, have shorter recovery times, and may result in similar hemodynamics.
- An ideal peri-operative risk score is characterized by:
- External validation in a separate and different patient population
- Specificity for the target population, i.e., patients operated on in high-volume surgical referral centers
- A contemporary cohort, i.e., patients operated on using modern surgical practices and established care pathways
- Ease of implementation at the bedside
- The PEACH score was designed to determine in-hospital mortality after cardiac surgery in ACHD. It was developed using a cohort of 1,782 patients in a high-volume surgical referral center in the United Kingdom. External validation was performed in a separate surgical referral center in Milan, Italy.
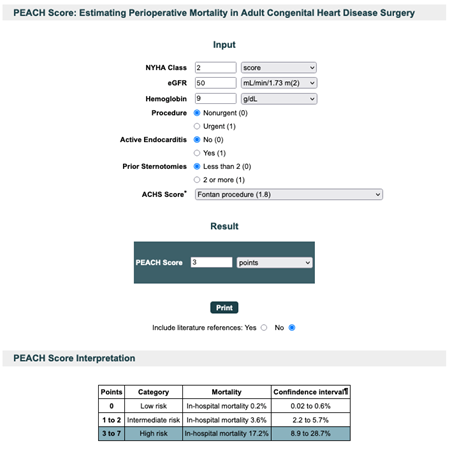
- The final PEACH score is a 3-tier score with seven clinical variables, to identify adult patients at low (0.2%), intermediate (3.6%), and high (17.2%) risk of in-hospital mortality after congenital cardiac surgery. Variables that result in a high (unfavorable) PEACH score are: NYHA functional class III or IV, urgent surgery, active endocarditis, two or more previous sternotomies, complex procedure (Adult Congenital Heart Surgery score >1.5), hemoglobin <100, or >200 g/L and an estimated glomerular filtration rate <60 mL/min/1.73m2.5
- The online PEACH score calculator (Figure 1) may be accessed here.6
Figure 1: PEACH Score Calculator
References
- Constantine A, Costola G, Bianchi P, et al. Enhanced assessment of perioperative mortality risk in adults with congenital heart disease. J Am Coll Cardiol 2021;78:234–42.
- Webb G, Mulder BJ, Aboulhosn J, et al. The care of adults with congenital heart disease across the globe: current assessment and future perspective: a position statement from the International Society for Adult Congenital Heart Disease (ISACHD). Int J Cardiol 2015;195:326–33.
- Marelli AJ, Ionescu-Ittu R, Mackie AS, Guo L, DendukuriN, Kaouache M. Lifetime prevalence of congenital heart disease in the general population from 2000 to 2010. Circulation 2014;130:749–56.
- Hörer J, Kasnar-Samprec J, Cleuziou J, et al. Mortality following congenital heart surgery in adults can be predicted accurately by combining expert-based and evidence-based pediatric risk scores. World J Pediatr Congenit Heart Surg 2016;7:425–35.
- Fuller SM, He X, Jacobs JP, et al. Estimating mortality risk for adult congenital heart surgery: an analysis of the Society of Thoracic Surgeons Congenital Heart Surgery Database. Ann Thorac Surg 2015;100:1728–35.
- PEACH Score: Estimating Perioperative Mortality in Adult Congenital Heart Disease Surgery (EBMcalc.com). 2021. Available at: https://ebmcalc.com/PEACH.htm. Accessed 08/11/2021.
Clinical Topics: Arrhythmias and Clinical EP, Cardiac Surgery, Congenital Heart Disease and Pediatric Cardiology, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Implantable Devices, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Cardiac Surgery and Arrhythmias, Cardiac Surgery and CHD and Pediatrics, Cardiac Surgery and Heart Failure, Congenital Heart Disease, CHD and Pediatrics and Arrhythmias, CHD and Pediatrics and Interventions, CHD and Pediatrics and Quality Improvement, Acute Heart Failure, Heart Transplant, Interventions and Structural Heart Disease
Keywords: Reoperation, Sternotomy, Heart-Lung Transplantation, Hospital Mortality, Glomerular Filtration Rate, Prunus persica, Developed Countries, Extracorporeal Membrane Oxygenation, Data Management, Heart Defects, Congenital, Cardiac Surgical Procedures, Arrhythmias, Cardiac, Heart Failure, Vascular Diseases, Ventricular Dysfunction, Heart Septal Defects, Atrial, Endocarditis, Anemia, Anesthesia, Blood Transfusion, Risk Factors, Hemodynamics, Referral and Consultation, Hemoglobins, Surgeons
< Back to Listings