MINOCA from A to Z
Quick Takes
- MINOCA (myocardial infarction with non-obstructive coronary arteries) is common (5-10% of all myocardial infarctions).
- The etiology of MINOCA is heterogenous; thus, MINOCA should be considered a working diagnosis warranting further investigation to identify the underlying mechanism.
- CMR (cardiovascular magnetic resonance) imaging might be considered a standard examination when the underlying cause is not identified.
The prognosis for myocardial infarction (MI) due to coronary artery disease (CAD) has improved over the last decades due to the development of coronary care units and early revascularization strategies.1,2 However, the widespread use of highly sensitive troponin assays and coronary angiography have revealed that a substantial group of MI patients lack significant (≥50%) coronary stenoses. This group is referred to as myocardial infarction with non-obstructive coronary arteries (MINOCA).
The diagnostic criteria for MINOCA have been proposed as 1) fulfilling the universal definition for MI,3 2) having non-obstructive coronary arteries on angiography (<50% stenosis) and 3) no clinically overt specific cause for the acute presentation.4,5
The etiology of MINOCA is heterogeneous and can be divided into coronary, cardiac and extra-cardiac causes. Coronary causes are occult plaque rupture or erosion, coronary spasm, spontaneous coronary artery dissection, coronary embolization, and coronary microvascular disorders. Myocarditis, Takotsubo syndrome, cardiomyopathies, cardiac trauma, and tachyarrhythmias are accounted for as cardiac causes, and stroke, pulmonary embolism, sepsis, renal failure, and hypoxemia are examples of extra-cardiac causes. Therefore, MINOCA should be considered a working diagnosis, warranting further investigation of the underlying cause.4
The prevalence of MINOCA is around 5-10% of all MIs, and approximately one third of patients present with ST-segment elevation on the electrocardiogram (ECG). In comparison with patients with MI-CAD, MINOCA patients are more likely to be younger and female and less likely to have treated hyperlipidemia, although other cardiovascular risk factors are similar. The prognosis of MINOCA was previously perceived as excellent but has later been shown to be serious, with a 1-year all-cause mortality rate of 3.5%. Cardiac magnetic resonance (CMR) imaging has developed into an important tool for further investigation of MINOCA, due to its ability to distinguish normal myocardium from Takotsubo syndrome, cardiomyopathies, and tissue scarring due to MI or myocarditis. Overall, CMR shows myocarditis in approximately 30%, MI in 25%, Takotsubo in 20% and normal myocardium in 25% of MINOCA patients.6 The diagnostic yield has been shown to increase with early and comprehensive CMR imaging, enabling identification of reversible causes of MINOCA such as myocarditis and Takotsubo syndrome.7 The combination of CMR imaging and assessing coronary morphology with optical coherence tomography (OCT) has also been shown to determine the underlying cause of MINOCA in up to 85% of female patients. However, the study cohort was relatively small and strictly selected.8
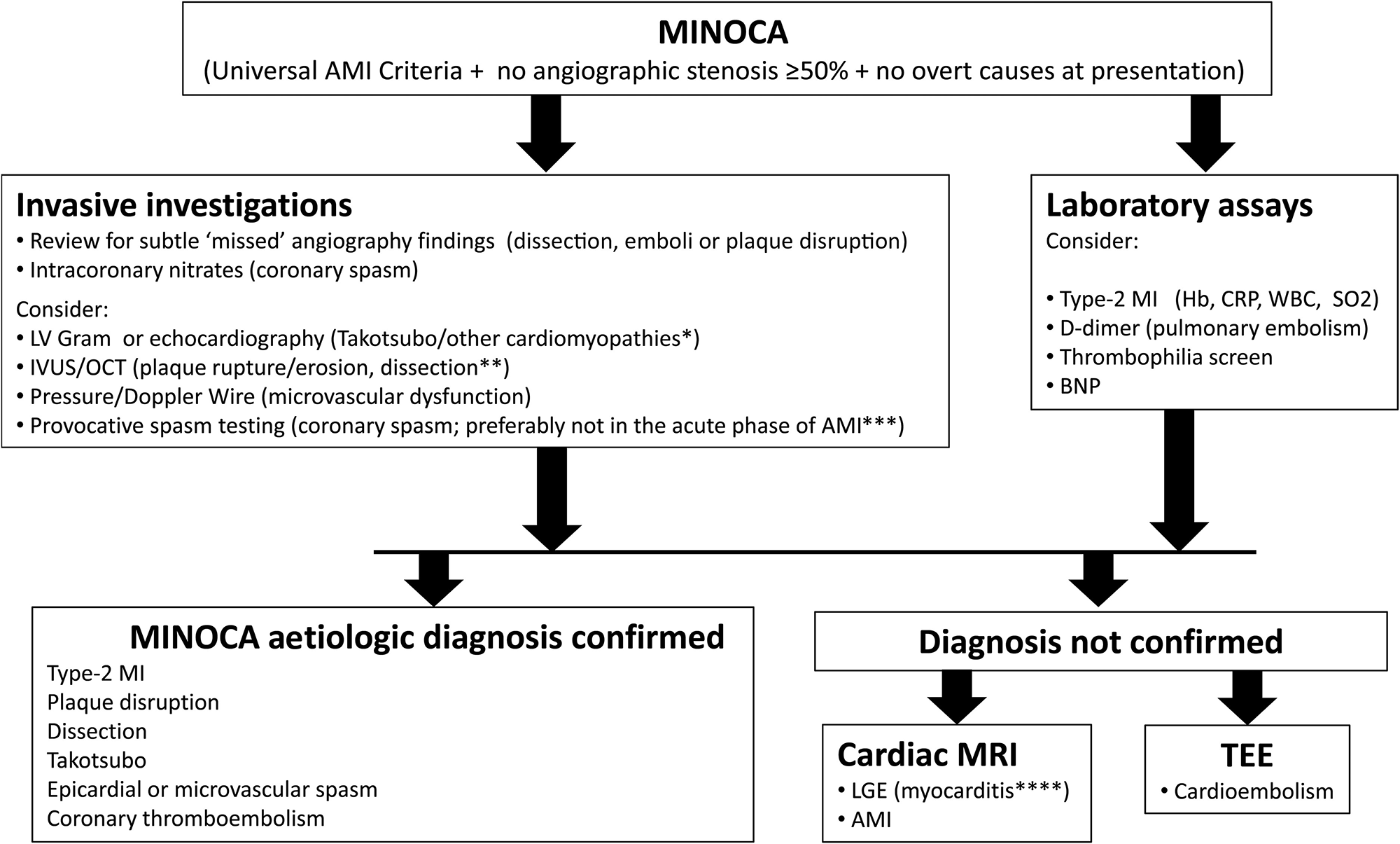
The investigation of MINOCA needs to be undertaken at two levels. Firstly, disorders mimicking MI need to be excluded. Secondly, the underlying cause responsible for the MINOCA needs to be sought. This is of great importance since failure to identify the underlying cause may result in inadequate treatment and inappropriate information given to the patient. When coronary angiography shows non-obstructive coronary arteries in a patient with MI, the clinical context should be reviewed for overlooked diagnoses i.e., extra-cardiac causes. The coronary angiography should be scrutinized for missed obstructions or dissections, and supplementary left ventricular angiogram or echocardiography performed to reveal wall motion abnormalities, Takotsubo syndrome, or pericardial effusion. Additional CMR imaging is recommended in unclear cases and should be performed promptly, preferably within 2 weeks, to ensure identification of transient causes of MINOCA. Further coronary vascular imaging with OCT or intravascular ultrasound (IVUS), and coronary functional assessment of microvascular function as well as coronary spasm provocation, are recommended if the etiology is not yet established (Figure 1).2,4,5
Figure 1
Figure 1: Recommended diagnostic algorithm for myocardial infarction with non-obstructive coronary arteries (MINOCA). * Cardiac magnetic resonance imaging (MRI) is recommended to verify the suspicion of Takotsubo syndrome. ** Intravascular ultrasound (IVUS) or optical coherence tomography (OCT) should be considered during index coronary angiography to detect occult plaque rupture/erosion or spontaneous coronary artery dissection (SCAD). *** Provocative testing for coronary artery spasm can be considered as a follow-up investigation in selected cases without an identified etiology. **** Certain and etiological diagnosis of myocarditis requires endomyocardial biopsy. AMI, acute myocardial infarction; BNP, B-type natriuretic peptide; CRP, C-reactive protein; Hb, hemoglobin; LGE, late gadolinium enhancement; LV, left ventricle; SO2, Oxygen saturation; TEE, transesophageal echocardiography; WBC, white blood cell count. Reprinted with permission Agewall S Beltrame JF, Reynolds HR, et al. ESC working group position paper on myocardial infarction with non-obstructive coronary arteries. Eur Heart J 2017;38:143-53.
There are so far no randomized controlled trials on secondary prevention treatment for MINOCA. In a SWEDEHEART registry study of more than 9,000 MINOCA patients followed for 4 years, a propensity score model showed significantly reduced major adverse cardiovascular events (MACE) (composite of all-cause mortality, hospitalization for MI, ischemic stroke, and heart failure) in patients treated with statins or angiotensin-converting enzyme inhibitors/angiotensin receptor blockers. Treatment with β-blockers also showed a positive trend, but dual antiplatelet therapy the first year after diagnosis was neutral.9 The results of the study should however be interpreted with caution due to the retrospective observational design with uncertainty in MINOCA diagnosing and risk of residual confounding. There is an immense need for well powered, randomized, controlled trials for the treatment of MINOCA.
References
- Collet JP, Thiele H, Barbato E, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J 2021;42:1289-1367.
- Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2018;39:119-77.
- Thygesen K, Alpert JS, Jaffee AS, et al. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol 2018;72:2231-64.
- Agewall S, Beltrame JF, Reynolds HR, et al. ESC working group position paper on myocardial infarction with non-obstructive coronary arteries. Eur Heart J 2017;38:143-53.
- Tamis-Holland JE, Jneid H, Reynolds HR, et al. Contemporary diagnosis and management of patients with myocardial infarction in the absence of obstructive coronary artery disease: a scientific statement from the American Heart Association. Circulation 2019;139: e891-e908.
- Pasupathy S, Air T, Dreyer RP, Tavella R, Beltrame JF. Systematic review of patients presenting with suspected myocardial infarction and nonobstructive coronary arteries. Circulation 2015;131:861-70.
- Sorensson P, Ekenback C, Lundin M, et al. Early comprehensive cardiovascular magnetic resonance imaging in patients with myocardial infarction with nonobstructive coronary arteries. JACC Cardiovasc Imaging 2021;14:1774-83.
- Reynolds HR, Maehara A, Kwong RY, et al. Coronary optical coherence tomography and cardiac magnetic resonance imaging to determine underlying causes of myocardial infarction with nonobstructive coronaryarteries in women. Circulation 2021;143:624-40.
- Lindahl B, Baron T, Erlinge D, et al. Medical therapy for secondary prevention and long-term outcome in patients with myocardial infarction with nonobstructive coronary artery disease. Circulation 2017;135:1481-89.
Clinical Topics: Arrhythmias and Clinical EP, Dyslipidemia, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Pericardial Disease, Prevention, Vascular Medicine, Atherosclerotic Disease (CAD/PAD), SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Nonstatins, Novel Agents, Statins, Acute Heart Failure, Heart Failure and Cardiac Biomarkers, Interventions and Coronary Artery Disease, Interventions and Imaging, Interventions and Vascular Medicine, Angiography, Echocardiography/Ultrasound, Magnetic Resonance Imaging, Nuclear Imaging, Acute Coronary Syndromes
Keywords: C-Reactive Protein, Contrast Media, Gadolinium, Hydroxymethylglutaryl-CoA Reductase Inhibitors, Natriuretic Peptide, Brain, Platelet Aggregation Inhibitors, Sulfur Dioxide, Coronary Angiography, Coronary Artery Disease, Takotsubo Cardiomyopathy, Tomography, Optical Coherence, Retrospective Studies, Follow-Up Studies, Prevalence, Brain Ischemia, Cardiovascular Diseases, Cicatrix, Constriction, Pathologic, Coronary Care Units, Echocardiography, Transesophageal, Heart Ventricles, Hyperlipidemias, Myocarditis, Pericardial Effusion, Propensity Score, Secondary Prevention, Risk Factors, Stroke, Coronary Stenosis, Registries, Troponin, Electrocardiography, Ultrasonography, Interventional, Angiotensin-Converting Enzyme Inhibitors, Hospitalization, Angiotensin Receptor Antagonists, Heart Disease Risk Factors, Magnetic Resonance Imaging, Leukocyte Count, Pulmonary Embolism, Magnetic Resonance Spectroscopy, Ischemic Stroke, Tachycardia, Renal Insufficiency, Heart Failure, Dissection, Hemoglobins, Algorithms, Myocardium
< Back to Listings