Pretreatment with P2Y12 Inhibitor in Patients with Acute Coronary Syndromes
Quick Takes
- In patients with acute coronary syndrome, pretreatment, defined as the administration of a P2Y12 inhibitor before assessment of coronary anatomy, may reduce early ischemic complications, but may unnecessarily increase bleeding risk if coronary artery disease is ultimately not confirmed or if urgent surgery is needed.
- Routine pretreatment with a P2Y12 inhibitor is not recommended in patients with NSTE-ACS, whereas in those with STEMI, the evidence is conflicting.
- Assessment of coronary anatomy before administration of a P2Y12 inhibitor appears to be the most reasonable strategy in an ACS setting, unless invasive management is delayed.
Definition and Rationale of Pretreatment
Dual antiplatelet therapy (DAPT) with aspirin and a P2Y12 receptor inhibitor is the cornerstone of treatment in patients with acute coronary syndrome (ACS). DAPT reduces the risk of stent thrombosis and recurrent myocardial infarction (MI),1,2 but the optimal timing of P2Y12 administration is a matter of debate. Specifically, the benefit of pretreatment (also referred to as upstream treatment), which is the administration of a P2Y12 loading dose before assessment of the coronary anatomy (i.e., in the ambulance, emergency department, coronary care unit) is unclear.3
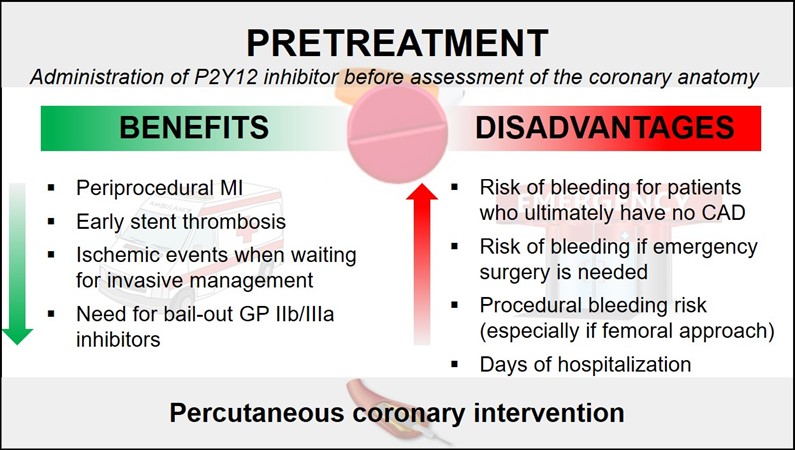
The rationale of pretreatment is to prevent early ischemic events occurring before or during percutaneous coronary intervention (PCI). However, this strategy may unnecessarily expose the patient to an increased bleeding risk if coronary artery disease (CAD) is ultimately not confirmed or if an urgent surgical procedure (e.g., coronary aortic bypass graft, repair of aortic dissection) is needed. In addition, it can increase the overall risk of periprocedural bleeding in patients undergoing PCI (Figures 1 and 2).
Figure 1
MI= myocardial infarction; CAD= coronary artery disease; GP= glycoprotein
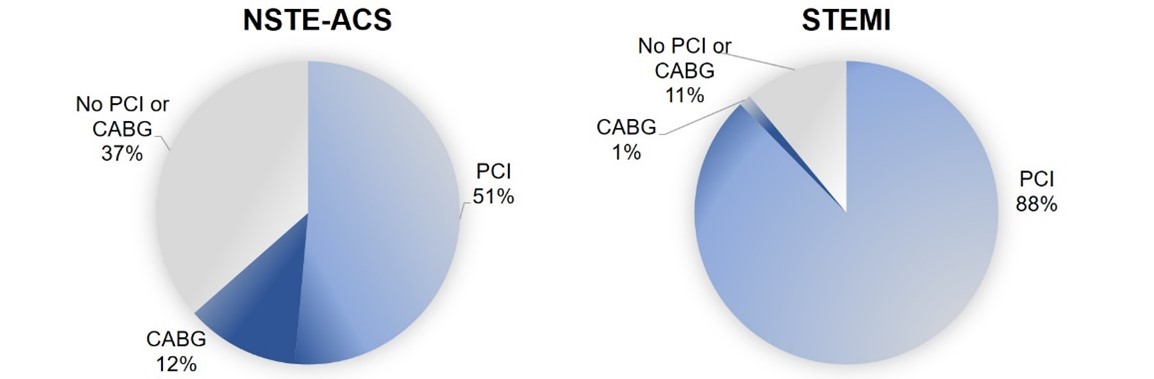
Figure 2
CABG= coronary artery bypass graft; PCI= percutaneous coronary intervention
Acute Coronary Syndrome Without ST-Elevation (NSTE-ACS)
The CURE trial4 is considered by some as acceptable evidence of the benefit of early pretreatment with clopidogrel in patients with NSTE-ACS. In this study, a strategy of clopidogrel 300mg followed by 75mg once daily was compared to placebo on a background of aspirin therapy. The clopidogrel arm had a lower risk of cardiovascular death, nonfatal MI, or stroke already at 24 hours after randomization (1.4% vs. 2.1%; relative risk [RR] 0.66; 95% CI 0.51 to 0.86) although at expense of more major bleeding (at 12 months: 3.7% vs. 2.7%; RR 1.38, 95% CI 1.13 to 1.67). However, the prolonged time interval between clopidogrel administration and coronary angiography (median of 10 days) and the low proportion of patients undergoing PCI (21%) do not reflect the current management of NSTE-ACS patients, making this study somewhat outdated (Table 1). In the CREDO trial,5 including 67% NSTE-ACS patients, a loading dose of clopidogrel 300mg administered 3 to 24 hours before PCI did not reduce the 28-day risk of death, MI, or urgent target-vessel revascularization (relative risk reduction [RRR] 18.5%; 95% CI, −14.2% to 41.8%; P = 0.23) compared with placebo, unless it was given ≥6 hours before (RRR 38.6%, 95% CI, −1.6% to 62.9%; P = 0.051). The risk of major bleeding was similar between clopidogrel and placebo (4.7% vs. 3.6%, P = 0.19). However, since only patients with coronary anatomy amenable to PCI were included, this study cannot be considered as a pretreatment trial. A small randomized trial6 failed to demonstrate a reduction in ischemic events with a loading dose of clopidogrel 600mg administered 4 to 8 hours versus administration in the catherization lab immediately before PCI. The ACCOAST trial7 also failed to demonstrate a reduction of ischemic events at 30 days after a prasugrel loading dose prior to (median of 4.3 hours) versus at time of PCI (10.8% vs. 10.8%, hazard ratio [HR] 0.997, 95% CI 0.83 to 1.20), but showed a significant increase in TIMI major and life-threatening bleeding (3.0% vs. 1.0%, HR 3.02, 95% CI 1.82 to 5.01 and 0.8% vs. 0.2%, HR 5.56, 95% CI 1.63 to 19.0, respectively). The DUBIUS trial8 showed no differences between ticagrelor administration before angiography or at the time of PCI for the composite ischemic endpoint (2.9% vs. 3.3%, absolute risk reduction [ARR] -0.46; 95% CI -2.90 to 1.90) or for Bleeding Academic Research Consortium (BARC) 3 to 5 at 30 days (1.6% vs. 1.9%, ARR -0.30, 95% CI -2.24 to 1.57). Notably, the trial was stopped early because of lower than anticipated event rates (futility), so no definitive conclusion can be drawn. Pretreatment versus no pretreatment was associated with a similar risk of ischemic events and more bleeding complications in one meta-analysis,9 while it reduced non-fatal ischemic events without increasing bleeding in two other meta-analyses.10,11 However, as dissimilar studies with different endpoint definitions were included in the three meta-analyses, these results must be considered only exploratory.3
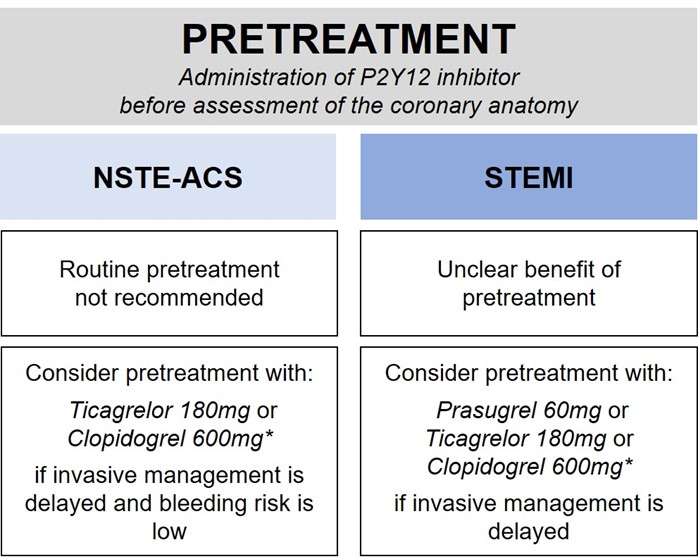
In conclusion, in patients with NSTE-ACS, routine pretreatment with a P2Y12 inhibitor is not recommended and may be considered only if an invasive approach is deferred and the patient's bleeding risk is low (Figure 3).12
Figure 3
*consider clopidogrel if a potent P2Y12 inhibitor is not available or is contraindicated
STEMI
A few small, randomized studies mostly relying on surrogate endpoints have explored the role of P2Y12 pretreatment in the setting of STEMI. Both the CIPAMI13 and the Load and GO14 trials failed to demonstrate a benefit of pretreatment with clopidogrel (Table 1). In the ATLANTIC study,15 the largest randomized evaluation of pretreatment in STEMI patients, ticagrelor 180mg given in the ambulance immediately after diagnosis of STEMI resulted in similar 30-day major adverse cardiovascular events (4.5% vs. 4.4%) and bleeding (1.3% vs. 1.3%) as compared with delayed administration in the catheterization laboratory. The rate of definite stent thrombosis at 30 days was significantly lower in the pretreatment arm but given the small number of events (2 vs. 11) and the absence of a consistent trend with respect to the other ischemic endpoints, the interpretation of this finding remains controversial. In ISAR-REACT 516 (41% STEMI patients), a prasugrel-based strategy with deferred loading after assessment of coronary anatomy was superior to a ticagrelor-based strategy involving routine pretreatment.
In summary, there is no conclusive evidence supporting pretreatment in STEMI patients. Because pretreatment was allowed in the studies that led to the approval of ticagrelor or prasugrel (PLATO17 and TRITON-TIMI 38,18 respectively), current international guidelines recommend administering one of the two agents, or clopidogrel if these are unavailable or contraindicated, before or at latest at the time of PCI (Figure 3).19,20
Summary
In patients with NSTE-ACS, routine pretreatment with a P2Y12 inhibitor before assessment of coronary anatomy is not supported by current evidence but it may be considered if invasive management is delayed and the patient is not at high bleeding risk. Similarly, it is unclear whether pretreatment provides any benefit to STEMI patients, in whom the P2Y12 inhibitor should be given before or at the latest at the time of PCI, according to invasive management delay, patient bleeding risk, and probability of an alternative diagnosis (e.g., aortic dissection).
References
- Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines: an update of the 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention, 2011 ACCF/AHA guideline for coronary artery bypass graft surgery, 2012 ACC/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease, 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction, 2014 AHA/ACC guideline for the management of patients With non-ST-elevation acute coronary syndromes, and 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery. J Am Coll Cardiol 2016;68:1082-115.
- Valgimigli M, Bueno H, Byrne RA, et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: The Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2018;39:213-60.
- Sibbing D, Kastrati A, Berger PB. Pre-treatment with P2Y12 inhibitors in ACS patients: who, when, why, and which agent? Eur Heart J 2016;37:1284-95.
- Yusuf S, Zhao F, Mehta SR, et al. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med 2001;345:494-502.
- Steinhubl SR, Berger PB, Mann JT 3rd, et al. Early and sustained dual oral antiplatelet therapy following percutaneous coronary intervention: a randomized controlled trial. JAMA 2002;288:2411-20.
- Di Sciascio G, Patti G, Pasceri V et al. Effectiveness of in-laboratory high-dose clopidogrel loading versus routine pre-load in patients undergoing percutaneous coronary intervention: results of the ARMYDA-5 PRELOAD (Antiplatelet therapy for Reduction of MYocardial Damage during Angioplasty) randomized trial. J Am Coll Cardiol 2010;56:550-57.
- Montalescot G, Bolognese L, Dudek D et al. Pretreatment with prasugrel in non-ST-segment elevation acute coronary syndromes. N Engl J Med 2013;369:999-1010.
- Tarantini G, Mojoli M, Varbella F, et al. Timing of oral P2Y12 inhibitor administration in patients with non-ST-segment elevation acute coronary syndrome. J Am Coll Cardiol 2020;76:2450-59.
- Bellemain-Appaix A, Kerneis M, O'Connor SA, et al. Reappraisal of thienopyridine pretreatment in patients with non-ST elevation acute coronary syndrome: a systematic review and meta-analysis. BMJ 2014;349:g6269.
- Bellemain-Appaix A, O'Connor SA, Silvain, J et al. Association of clopidogrel pretreatment with mortality, cardiovascular events, and major bleeding among patients undergoing percutaneous coronary intervention: a systematic review and meta-analysis. JAMA 2012;308:2507-16.
- Nairooz R, Valgimigli M, Rochlani Y, et al. Meta-analysis of clopidogrel pretreatment in acute coronary syndrome patients undergoing invasive strategy. Int J Cardiol 2017;229:82-89.
- Collet JP, Thiele H, Barbato E, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J 2021;42:1289-1367.
- Zeymer U, Arntz HR, Mark B, et al. Efficacy and safety of a high loading dose of clopidogrel administered prehospitally to improve primary percutaneous coronary intervention in acute myocardial infarction: the randomized CIPAMI trial. Clin Res Cardiol 2012;101:305-12.
- Ducci K, Grotti S, Falsini G, et al. Comparison of pre-hospital 600 mg or 900 mg vs. peri-interventional 300 mg clopidogrel in patients with ST-elevation myocardial infarction undergoing primary coronary angioplasty. the Load&Go randomized trial. Int J Cardiol 2013;168:4814-16.
- Montalescot G, van 't Hof AW, Lapostolle F, et al. Prehospital ticagrelor in ST-segment elevation myocardial infarction. N Engl J Med 2014;371:1016-27.
- Schupke S, Neumann FJ, Menichelli, M et al. Ticagrelor or prasugrel in patients with acute coronary syndromes. N Engl J Med 2019;381:1524-34.
- Wallentin L, Becker RC, Budaj A, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 2009;361:1045-57.
- Wiviott SD, Braunwald E, McCabe CH, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 2007;357:2001-15.
- Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J 2019;40:87-165.
- O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013;61:485-510.
Clinical Topics: Acute Coronary Syndromes, Cardiac Surgery, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Stable Ischemic Heart Disease, Vascular Medicine, Atherosclerotic Disease (CAD/PAD), ACS and Cardiac Biomarkers, Aortic Surgery, Cardiac Surgery and SIHD, Interventions and ACS, Interventions and Coronary Artery Disease, Interventions and Imaging, Interventions and Vascular Medicine, Angiography, Nuclear Imaging, Chronic Angina
Keywords: Platelet Aggregation Inhibitors, Clopidogrel, Ticagrelor, Purinergic P2Y Receptor Antagonists, ST Elevation Myocardial Infarction, Percutaneous Coronary Intervention, Acute Coronary Syndrome, Coronary Artery Disease, Coronary Angiography, Coronary Care Units, Laboratories, Medical Futility, Numbers Needed To Treat, Risk, Hemorrhage, Aspirin, Stents, Thrombosis, Stroke, Coronary Artery Bypass, Emergency Service, Hospital, Biomarkers, Aneurysm, Dissecting, Glycoproteins, Algorithms
< Back to Listings