A Remote Technology-Enabled, Algorithm-Guided Program to Improve Health Equity in Hypertension and LDL-C Management
Quick Takes
- A remote technology-enabled monitoring program that delivers algorithm-based pharmacist-driven medication titration has shown potential in improving hypertension and cholesterol (LDL-C) control in high-risk patients.
- Combining technology (electronic health record screening tool, text messages, digitally connected blood pressure monitors) with non-physicians (i.e., patient navigators, pharmacists, advanced practice providers) increased patient access to guideline recommended therapies.
- Traditionally underserved patient populations participated in this program; this provides support for digitally enabled remote care models to deliver equitable care.
Achieving guideline-directed targets for hypertension (HTN) and cholesterol management has remained a daunting clinical challenge, particularly among underserved patient populations. About 30% to 50% of patients do not receive optimal medical treatment, despite guideline-directed recommendations and affordability.1,2 This is a major population health concern for both health inequalities and increased risk of preventable cardiovascular events, morbidity, and mortality. Digital health interventions have shown a great potential to improve access and adherence to guideline-recommended medical therapies (GDMT) for cardiovascular disease.3
An innovative study by Dr. Blood and colleagues conducted within the Massachusetts General Brigham Health System, initiated in January 2018, investigated the impact of a remote, algorithmically driven disease-management program targeting HTN and lipid control.4,5 Patients were identified using either a clinician referral or an electronic health record screening tool.
The program used an electronic medical record-based identification system to find eligible patients with elevated LDL-C and HTN. Patients were categorized, using current guidelines,6 based on the presence of atherosclerotic disease, diabetes, severe hypercholesterolemia or high-risk primary prevention. Blood pressure monitoring was performed via digitally connected home blood pressure devices. Pharmacists, using guideline-directed algorithms, initiated and titrated medications until a guideline-directed target LDL-C6 and average BP <130/80 mm Hg was achieved.
Throughout the program, there was physician oversight as needed. Patient navigators were the primary drivers of the intervention at the patient care level. They trained patients on proper blood pressure measurement techniques, provided education at preset intervals, shared lab results, and served as the main point of contact during the study. The navigator coordinated the GDMT management with the pharmacist and if needed the supervising clinician until a target LDL-C per guidelines and average BP <130/80 mm Hg was achieved.
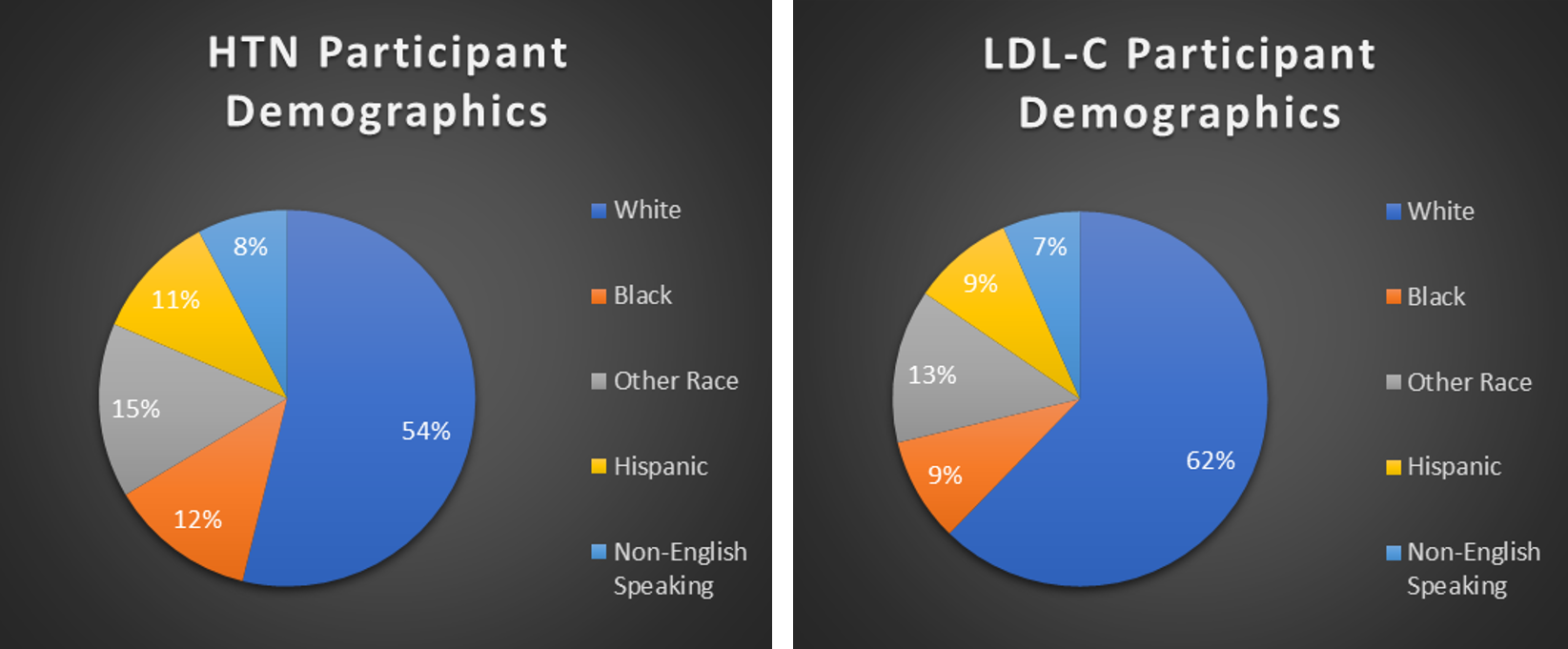
In total, 28,473 patients were screened, and 10,803 patients were enrolled of which 9,547 elected to be medically managed. Approximately one-third of patients who elected to be medically managed continued to participate in the study. A total of 3,367 patients were enrolled in the HTN program and 6,887 were enrolled in the lipid program.
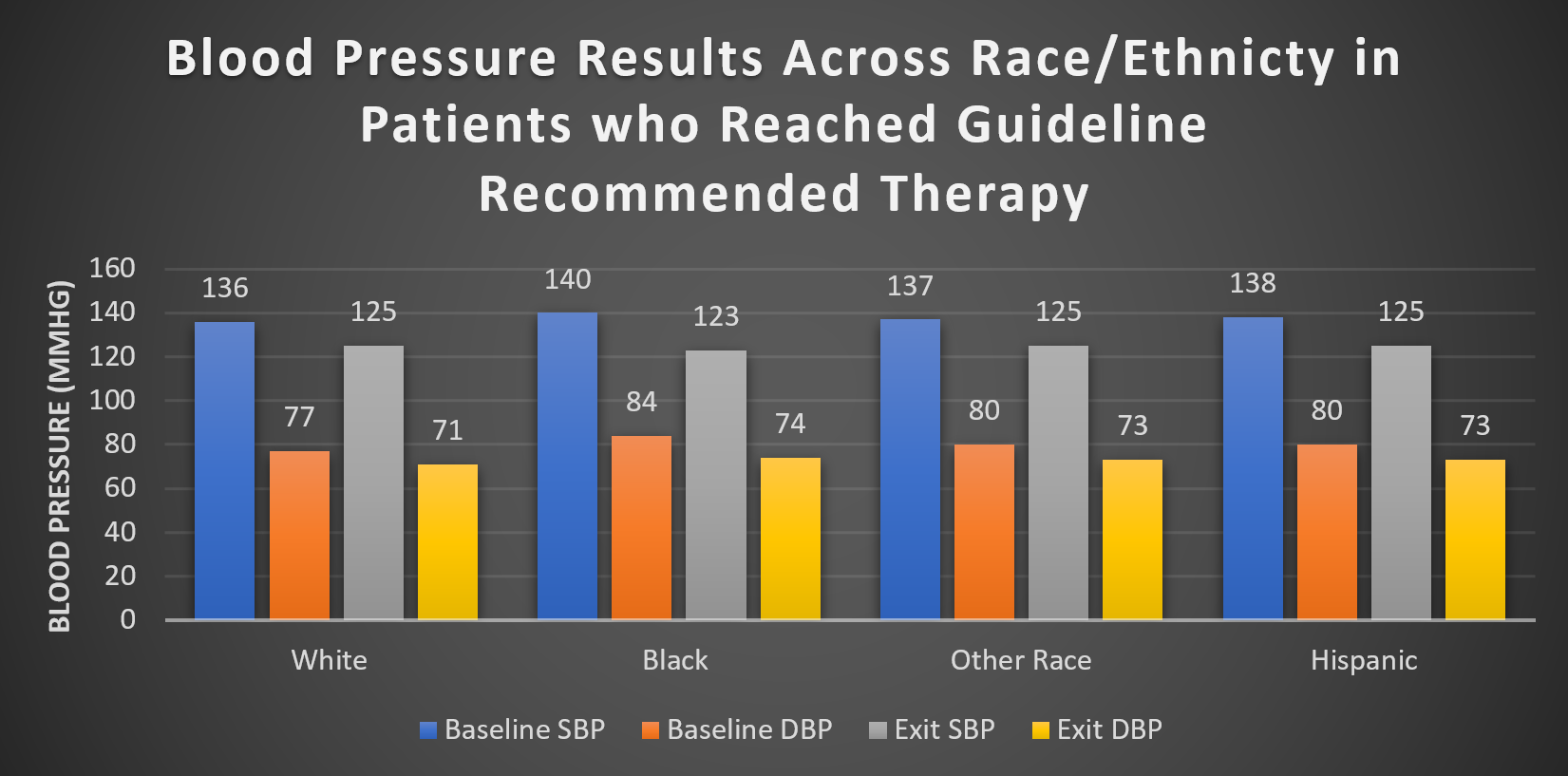
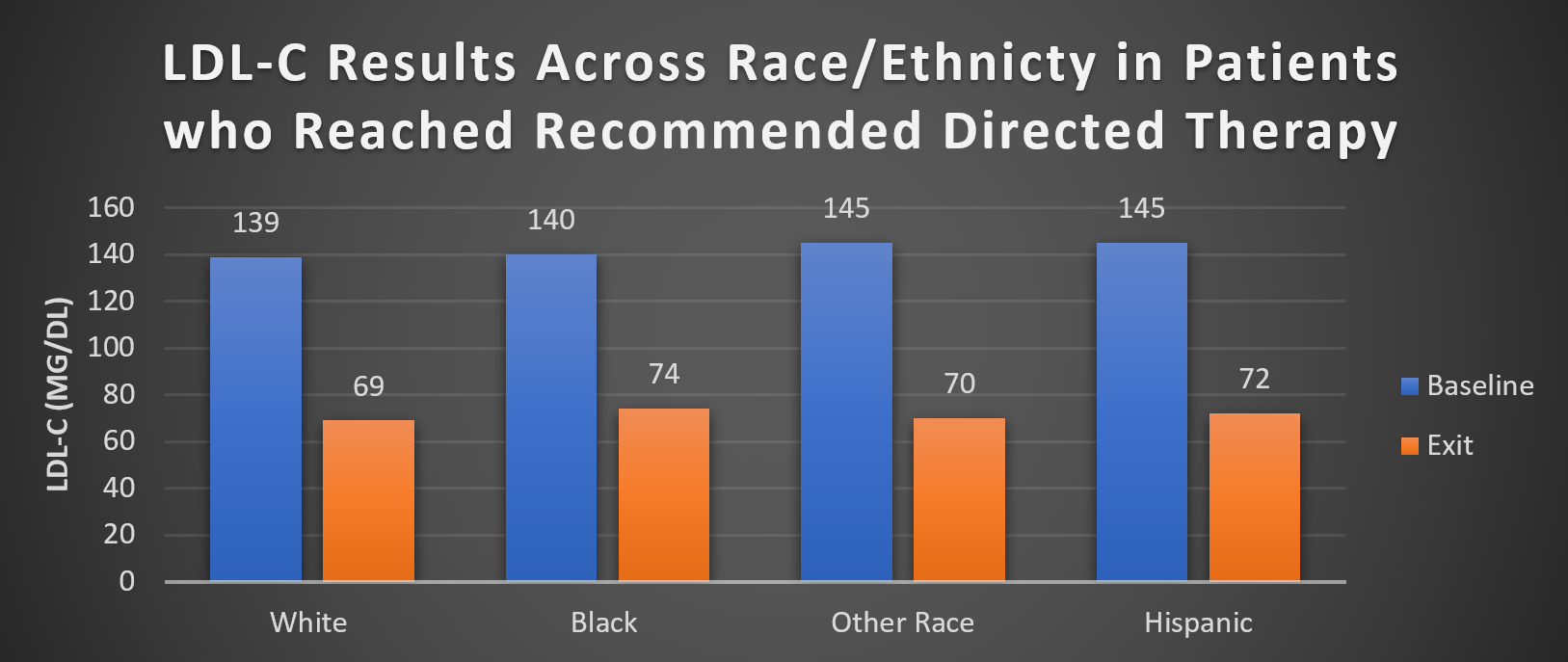
Based on preliminary data at 3 months, 1,555 patients (23%) in the lipid program and 510 patients (15%) in the HTN program had their medications up titrated by a pharmacist. Furthermore, 40% (2,753 patients) of those in the lipid arm and 44% (1,492 patients) in the blood pressure arm achieved guideline-recommended goal. The average reduction in blood pressure was 12 mmHg systolic and 7 mmHg diastolic in patients who reached guideline-recommended blood pressure goal. There was a 50% decrease in LDL-C from 140 mg/dL to 70 mg/dL in those who achieved a guideline-recommended lipid-lowering regimen.
Figure 1
Figure 2
Figure 3
This remote technology-enabled, algorithm-guided monitoring program is a promising model to deliver guideline-directed care to patients including traditionally underserved populations. To make advancements in prevention, multidisciplinary approaches, such as the use of patient navigators, text message, and wireless communication to improve medical adherence,7,8 are becoming more important. Developing innovative models that are inclusive and consider social determinants of health9 in patients within vulnerable populations (e.g., elderly, low socioeconomic class, low health literacy) is crucial.
The strengths of this model include decreasing the need for in-person visits. Patient navigators can assist patients with low health literacy. Pharmacists can offer recommendations that are affordable and accessible via generic medication to address health economic challenges for low-income populations. These are important barriers to address to provide equitable care accessible to patients from all backgrounds.
With the continual advancement in technology, we are excited about the future, which will continue to incorporate behavior trends from wearables and integrate other smartphone health data into more advanced cardiovascular prediction models. These programs reinforce self-management of cardiovascular risk factors (e.g., blood pressure control, sleep hygiene, glycemic control, exercise, and diet). There is great potential to further risk stratify and increase cardiovascular disease prevention and advance health equity in a more patient-centered way. In the future, we hope to see these types of innovative technology-based and community health worker driven programs scaled to larger patient populations and expanded to address other cardiovascular conditions.
References
- Muntner P, Hardy ST, Fine LJ, et al. Trends in blood pressure control among US adults with hypertension, 1999-2000 to 2017-2018. JAMA 2020;324:1190-1200.
- Nirav P, Anirudh B, Rajat K, et al. Trends in lipid, lipoproteins, and statin use among U.S. adults. J Am Coll Cardiol 2019;74:2525-28.
- Khairat S, Haithcoat T, Liu S, et al. Advancing health equity and access using telemedicine: a geospatial assessment. J Am Med Inform Assoc 2019;26:796-805.
- Scirica BM, Cannon CP, Fisher NDL, et al. Digital care transformation: interim report from the first 5000 patients enrolled in a remote algorithm-based cardiovascular risk management program to improve lipid and hypertension control. Circulation 2021;143:507-09.
- Does a Remote Algorithm-Based CV Risk Management Program Lower Lipid and HTN Levels? http://www.acc.org. Nov 17, 2020. Accessed Dec 16, 2021 .https://www.acc.org/latest-in-cardiology/articles/2020/11/12/20/28/tues-127pm-digital-care-transformation-aha-2020.
- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019;73:3168-3209.
- Schwebel FJ, Larimer ME. Using text message reminders in health care services: a narrative literature review. Internet Interv 2018;13:82-104.
- McBrien KA, Ivers N, Barnieh L, et al. Patient navigators for people with chronic disease: a systematic review. PLoS One 2018;13:e0191980.
- Butler SM. What is the outlook for addressing social determinants of health? JAMA Health Forum 2021;2:e213639.
Clinical Topics: Cardiovascular Care Team, Dyslipidemia, Prevention, Homozygous Familial Hypercholesterolemia, Lipid Metabolism, Nonstatins, Diet, Hypertension
Keywords: Vulnerable Populations, Cardiovascular Diseases, Cholesterol, LDL, Pharmacists, Electronic Health Records, Hypercholesterolemia, Blood Pressure, Community Health Workers, Glycemic Control, Health Equity, Health Literacy, Health Status Disparities, Patient Navigation, Preliminary Data, Smartphone, Social Determinants of Health, Text Messaging, Risk Factors, Hypertension, Diabetes Mellitus, Referral and Consultation, Heart Disease Risk Factors, Primary Prevention, Population Health, Costs and Cost Analysis, Socioeconomic Factors, Patient Care, Algorithms, Physicians, Technology, Wearable Electronic Devices, Diet
< Back to Listings