2022 AHA Statement on the Comprehensive Management of CV Risk Factors For Adults With T2DM
Quick Takes
- The American Heart Association (AHA) has released a scientific statement in 2022 offering new guidance for comprehensive management of diabetes highlighting the need for allocating preventive therapy based on the result of cardiovascular outcome trials (CVOTs).
- A key step in the care of patients with type 2 diabetes mellitus (T2DM) is to address lifestyle modification; cardiovascular (CV) risk assessment is recognized as a critical component of cardiovascular disease (CVD) risk reduction.
- The statement encourages cardiologists to recognize unmet needs in health care delivery, embracing the importance of prescribing evidence-based glucose lowering therapies shown to have cardiovascular benefit, and prescribing them beyond their historical comfort zone which will help to further lower CV risk.
The global prevalence of type 2 diabetes mellitus (T2DM) has sharply increased over the past four decades, and is projected to increase further, leading to substantial personal, social, and economic morbidity.1 Cardiovascular disease (CVD) remains the leading cause of death and disability in patients with diabetes. Clear, evidence-based recommendations for managing CV risks in diabetic or non-diabetic patients have never been more urgent.
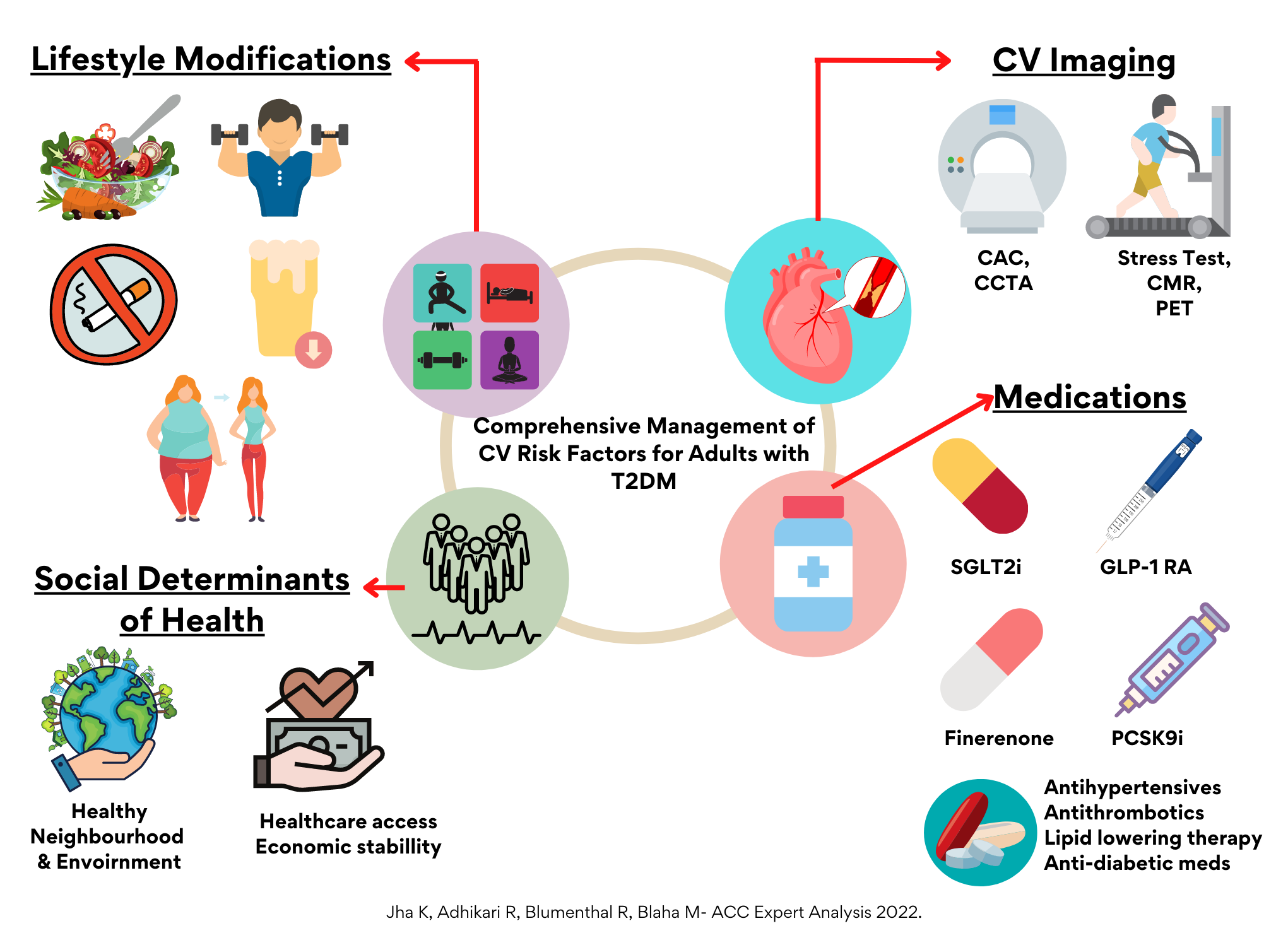
The American Heart Association (AHA) released a 2022 statement for comprehensive management of CV risk factors for adults with T2DM which include three key components: lifestyle interventions, screening for CV and renal complications, and pharmacological management.2 Since the prior joint statement by the AHA/American Diabetes Association (ADA) in 2015,3 there has been an unparalleled increase in new trials demonstrating CV benefits of novel preventive therapies; these include sodium glucose co-transporter 2 (SGLT2i), glucagon-like peptide-1 receptor agonists (GLP1-RA), icosapent ethyl, and selective nonsteroidal mineralocorticoid receptor antagonists, for example. These therapeutic options provide significant opportunities for improving care of patients with T2DM. There are several notable differences from prior AHA statements including advocating shared decision making regarding preventive pharmacotherapy considering evolving evidence.2,3
Lifestyle Management
Increased physical activity, smoking cessation, abstinence from or moderation of alcohol consumption, tailored nutrition plan, and evidence-based pharmacological/surgical interventions for weight reduction are important in CV risk reduction among individuals with T2DM. Consistent with other preventive guidelines, the AHA statement also recommends lifestyle modification as the primary intervention to prevent and treat T2DM.
Pharmacological Management
Timely and appropriate prescription of antihyperglycemic, lipid-lowering, antithrombotic, and antihypertensive therapies is central to comprehensive primary and secondary prevention of CVD in T2DM. The 2022 statement favorably recommends prescribing these medications.
- In 2008, the U.S. Food and Drug Administration (FDA) mandated that all new antihyperglycemic therapies demonstrate CV safety in phase 3 trials and further undergo post marketing phase 4 trials.4 Since then, multiple clinical trials of SGLT2i/GLP-1RA have demonstrated several cardiometabolic benefits including reduction in coronary artery disease (CAD), cerebrovascular disease, and heart failure prompting the FDA to grant major adverse cardiac event reduction labels to medications with demonstrated CV benefit.5,6 Multiple societies recommend initiating SGLT2is or GLP-1RAs for adults with atherosclerotic cardiovascular disease (ASCVD) risk factors, irrespective of baseline antihyperglycemic therapies of HbA1c. The updated 2022 AHA statement further endorses this strategy.
- Diabetic kidney disease (DKD) is independently associated with poor CV outcomes. Robust clinical trial data suggest that both SGLT2is and GLP-1RAs, and most recently finerenone, a selective nonsteroidal mineralocorticoid receptor antagonist, improve renal and CV outcomes in patients with DKD.5-7 In addition to these novel treatments, traditional strategies for delaying progression of DKD, including blood pressure (BP) control, glycemic control, and renin-angiotensin-aldosterone system (RAAS) inhibition, remain essential. The 2022 AHA statement endorses both traditional treatments and novel cardiometabolic therapies, including SGLT2i, GLP1-RA or finerenone, to lower CV and renal events in patients with DKD.
- The new AHA statement emphasizes established risk factor modification, including an individualized approach for hypertension management and reducing LDL-cholesterol to a target range. It further supports considering non-statin therapies, including ezetimibe, proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors, icosapent ethyl, and antithrombotic therapies for primary and secondary prevention of CVD in patients with T2DM.
Imaging
Screening for CAD in asymptomatic T2DM patients remains debatable. While anatomical assessment (coronary computed tomography angiography [CCTA]) or functional imaging (stress test) can facilitate risk stratification and tailoring of preventive therapies for primary and secondary prevention of CVD in T2DM patients, routine use of ischemia testing in asymptomatic patients is strongly discouraged. Likewise, coronary artery calcium (CAC) score appears to provide the most actionable triggers for considering preventive therapies including antithrombotic drugs, lipid lowering therapies, and GL1-RAs for primary prevention. The 2022 AHA statement supports considering anatomical or functional imaging for CV risk stratification, shared decision-making, and allocation of preventive therapies which will optimize CV risk factors and affirm healthy lifestyle habits.
Conclusion
The 2022 AHA statement features compelling evidence from important CVOTs highlighting the role of newer cardiometabolic medications. It highlights implementing patient-centered diabetes management, including optimal lifestyle interventions, strong risk factor control, and tighter treatment targets to prevent adverse CV outcomes. It may be reasonable to obtain CAC in asymptomatic diabetic patients for refining risk, allocating, and titrating preventive therapies.
In patients with T2DM and additional risk factors for CVD, preventive medical therapies, including newer anti-hyperglycemic and non-statin lipid-lowering medications, should be initiated, but lifestyle and behavioral interventions should be concurrently emphasized. Cardiologists should be poised to determine eligible patients for novel treatment strategies and in a prime position to direct these therapies. The 2022 AHA statement recommends utilizing collaborative approaches to reduce therapeutic inertia and facilitate the adoption of these medications in cardiology practice. The choice of traditional and novel preventive medications to reduce CV events should be individualized based on the presence of risk factors for CVD. Shared decision-making, patient preference, cost effectiveness and medication adherence should all be considered in making these decisions.
Future Directions
Recent clinical trials have demonstrated encouraging responses and these novel preventive medications have been adopted by several guidelines, and the 2022 AHA statement is unequivocally endorsing them. Thus, it is crucial that cardiologists should regularly screen patients for diabetes, aggressively treat risk factors, and routinely prescribe evidence-based novel preventive therapies to reduce CV risk.
The new AHA statement will be a valuable resource to patients and clinicians to help them implement lifestyle interventions and preventive therapies. Updating and harmonizing guidelines among all major societies will eliminate confusion among clinicians managing T2DM and allow for more efficacious, patient-centered treatment. The 2022 AHA statement reflects a rapidly evolving body of research in a quickly changing field. With new therapies such as tirzepatide, lipoprotein (a) lowering therapies,8,9 and others currently undergoing evaluation in randomized controlled trials (RCTs), the field is rapidly evolving and will necessitate regular updating of such statements.
Multifaceted, collaborative approaches are essential to raise awareness and empower patients to prevent/manage CVD. This can be accomplished by focusing on social determinants of health, providing comprehensive and affordable care, and reducing premature mortality by risk stratification and optimizing pharmacologic regimens. Nevertheless, better insurance coverage for novel therapies and selective use of CV imaging modalities is needed to reap the benefits of these recent innovations, and hopefully this statement will facilitate these urgent changes.
Figure 1
References
- National Diabetes Statistics Report, 2020: Estimates of Diabetes and its Burden in the United States (cdc.gov). 2020. Available at: https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf. Accessed 01/25/2022.
- Joseph JJ, Deedwania P, Acharya T, et al. Comprehensive management of cardiovascular risk factors for adults with type 2 diabetes: a scientific statement from the American Heart Association. Circulation 2022;145:e722-e759.
- Fox CS, Golden SH, Anderson C, et al. Update on prevention of cardiovascular disease in adults with type 2 diabetes mellitus in light of recent evidence: a scientific statement from the American Heart Association and the American Diabetes Association. Diabetes Care 2015;38:1777-803.
- Guidance for Industry: Diabetes Mellitus - Evaluating Cardiovascular Risk in New Antidiabetic Therapies to Treat Type 2 Diabetes (fda.gov). 2008. Available at: https://www.fda.gov/media/71297/download. Accessed 01/25/2022.
- Giugliano D, Scappaticcio L, Longo M, et al. GLP-1 receptor agonists and cardiorenal outcomes in type 2 diabetes: an updated meta-analysis of eight CVOTs. Cardiovasc Diabetol 2021;20:189.
- McGuire DK, Shih WJ, Cosentino F, et al. Association of SGLT2 inhibitors with cardiovascular and kidney outcomes in patients with type 2 diabetes: a meta-analysis. JAMA Cardiol 2021;6:148-58.
- Agarwal R, Filippatos G, Pitt B, et al. Cardiovascular and kidney outcomes with finerenone in patients with type 2 diabetes and chronic kidney disease: the FIDELITY pooled analysis. Eur Heart J 2022;43:474-84.
- Frías JP, Davies MJ, Rosenstock J, et al. Tirzepatide versus semaglutide once weekly in patients with type 2 diabetes. N Engl J Med 2021;385:503-15.
- Tsimikas S, Karwatowska-Prokopczuk E, Gouni-Berthold I, et al. Lipoprotein(a) reduction in persons with cardiovascular disease. N Engl J Med 2020;382:244-55.
Clinical Topics: Cardiovascular Care Team, Dyslipidemia, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Prevention, Vascular Medicine, Atherosclerotic Disease (CAD/PAD), Advanced Lipid Testing, Lipid Metabolism, Nonstatins, Novel Agents, Statins, Acute Heart Failure, Interventions and Coronary Artery Disease, Interventions and Imaging, Interventions and Vascular Medicine, Computed Tomography, Nuclear Imaging, Hypertension
Keywords: Mineralocorticoid Receptor Antagonists, PCSK9 protein, human, Antihypertensive Agents, Calcium, Fibrinolytic Agents, Glucagon-Like Peptide-1 Receptor, Glycated Hemoglobin A, Proprotein Convertase 9, Renin-Angiotensin System, Cardiovascular Diseases, Diabetes Mellitus, Type 2, American Heart Association, Secondary Prevention, Blood Pressure, Computed Tomography Angiography, Coronary Artery Disease, Cost-Benefit Analysis, Decision Making, Shared, Exercise Test, Glycemic Control, Mortality, Premature, Patient Preference, Quality Improvement, Social Determinants of Health, United States Food and Drug Administration, Risk Factors, Hypoglycemic Agents, Hypertension, Heart Failure, Life Style, Risk Assessment, Risk Assessment, Cerebrovascular Disorders, Medication Adherence, Alcohol Drinking, Healthy Lifestyle, Insurance Coverage, Primary Prevention, Weight Loss, Patient-Centered Care, Risk Reduction Behavior, Lipoprotein(a), Prescriptions, Cholesterol, Subtilisins, Ezetimibe, Ischemia, Glucose, Lipids, Sodium
< Back to Listings