Optimize Cardiovascular Risk Factors For Prevention of Heart Failure
Quick Takes
- A recent analysis of Atherosclerosis Risk in Communities data shows that the number of poorly controlled risk factors and severity of disease state correlate with increased risk of developing heart failure. Patients with multiple uncontrolled risk factors were at highest risk for heart failure, whereas those with no cardiovascular risk factors had the lowest future incidence of heart failure.
- Cardiologists and primary care physicians should emphasize the importance of risk factor optimization to prevent heart failure, including the early use of SGLT2 inhibitors for patients with diabetes.
- Rather than focusing only on the risk of atherosclerotic disease, cardiologists and primary care doctors should also counsel patients on the risk of developing heart failure and arrhythmias such as atrial fibrillation when discussing cardiovascular risk factors and healthy behaviors.
Importance of Heart Failure Prevention
Heart failure (HF) is a major cause of morbidity, mortality, and healthcare expense, but HF prevention has been underappreciated in global cardiovascular risk assessment and intervention within preventive cardiology. About 6.2 million adults live with HF in the United States (US),1 leading to a cost of approximately $30.7 billion nationally.2 Given the extensive health and financial costs, there is an urgent need for improved prevention of HF.
Prevention of HF is best achieved through sustained, life-long cardiovascular health, as defined by adherence to the American Heart Association's Life's Simple 7,3 which is focused on the reduction of modifiable risk factors and optimization of health behaviors, specifically smoking, exercise, diet, body mass index, cholesterol, blood pressure, and glycemic control.
Coexistence of Multiple Risk Factors
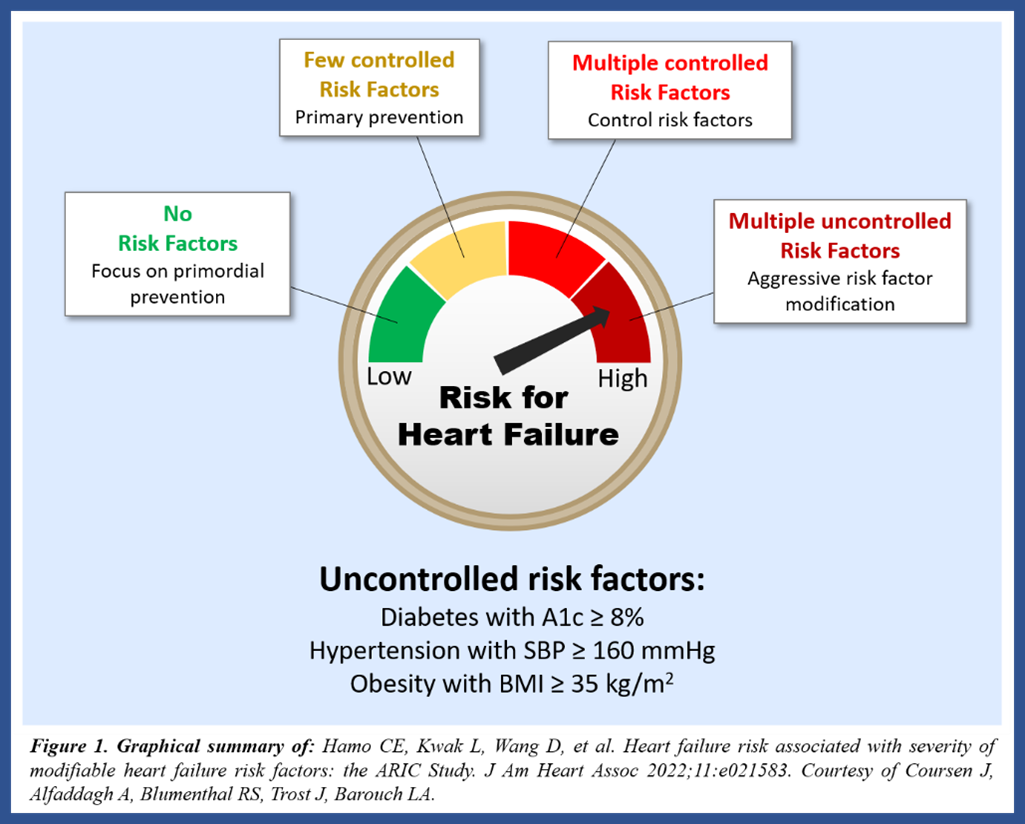
A recent analysis of the Atherosclerosis Risk in Communities (ARIC) cohort led by Drs. Carine Hamo and Chiadi Ndumele et al. showed that poorly controlled risk factors are associated with increased incidence of HF (Figure 1). In this observational study, an increase in the number and severity of modifiable risk factors (hypertension, obesity, and diabetes) was associated with an increased risk of developing HF. Patients with multiple uncontrolled risk factors were at the highest risk of developing HF.
Figure 1
The risk factors most highly correlated with HF incidence were poorly controlled diabetes (Hgb A1c ≥8%), uncontrolled hypertension (SBP ≥160), and advanced obesity (BMI ≥35).4 These risk factors frequently co-exist simultaneously in patients. For example, metabolic syndrome, which includes many of the same risk factors, is present in approximately one-third of the US population, and the prevalence continues to rise.5 The optimization of multiple risk factors is necessary to reduce the incidence of HF for many high-risk patients.
Given the risk of poorly controlled diabetes in the development of HF,6 there should be a low threshold for initiation of cardioprotective diabetic medications. Specifically, cardiologists should consider early use of SGLT2 inhibitors for patients with diabetes at risk for HF, especially given the cardioprotective benefits demonstrated in the EMPA-REG OUTCOME trial.7,8
Importance of Primordial Prevention
Dr. Hamo et al. found that the absence of cardiovascular risk factors was associated with the lowest incidence of HF,4 suggesting the value of primordial prevention (the prevention of cardiovascular risk factors). This highlights the role of risk exposure in cardiovascular health. Increased exposure to cardiovascular risk factors leads to increased HF incidence, even years prior to HF diagnosis or hospitalization.9 Conversely, delaying or averting the onset of risk factors such as diabetes through lifestyle interventions is linked to prevention of HF.10 Risk factor prevention reduces cardiovascular disease burden, including HF.
Risk Factor Optimization
Another interesting conclusion from the Hamo et al. ARIC analysis was the benefit of mitigating risk factors. Patients with mildly uncontrolled risk factors had lower incidence of HF compared to those with severely uncontrolled risk factors.4 Thus, even partial optimization of a risk factor, such as improvement of HgbA1c, is valuable in HF prevention, even if the risk factor is not completely abolished.
Similarly, other studies have demonstrated significant benefit of initiating health behaviors; for example, the initiation of physical activity is associated with decreased risk of HF, even if exercise is started later in life.11 Cardiologists and primary care doctors should take the approach that "some (improvement) is better than none" when counseling patients.
Heart Failure in Cardiovascular Disease Risk Calculation
Unfortunately, current cardiovascular risk calculators do not include any estimate of risk for HF or arrhythmias such as atrial fibrillation (AF). The exclusion of HF and AF in current HF calculators leads to a systematic underestimation of cardiovascular disease risk. Quantitative risk assessments via pooled cohort equations (PCE) are key tools used in clinical practice today for effective prevention of atherosclerotic cardiovascular disease (ASCVD). However, there are significant limitations in the accuracy of these assessments, especially for patients of certain racial/ethnic groups, patients with chronic inflammatory diseases, and patients of lower socioeconomic status.12
A risk calculator that includes global cardiovascular risk, including HF and AF, would be valuable to clinicians to estimate cardiovascular disease development more accurately and fully. As a hypothetical example, a 55-year-old obese patient with type 2 diabetes mellitus and a 10% risk of ASCVD may have an additional 25% risk of HF13 and 20% risk of AF,14 but these non-ASCVD risks are unaccounted for by use of the PCE alone. A cumulative estimate of global cardiovascular risk would better reflect the true burden of cardiovascular disease and would likely be more motivational for at-risk patients. Given this data from the ARIC analysis and related studies, clinicians should counsel patients on the additional risk of developing HF when discussing cardiovascular risk factors and health behaviors.
Conclusions
HF incidence is closely tied to the severity and extent of poorly controlled modifiable cardiovascular risk factors. Cardiologists and primary care physicians should emphasize the importance of risk factor optimization, including the early use of SGLT2 inhibitors for patients with diabetes, to reduce risk of HF. Although current cardiovascular risk calculators systemically underestimate the overall risk of cardiovascular disease by not including the risk of HF and arrhythmias, cardiologists should discuss the risk of HF while counseling patients. There is an important need for more research on risk reduction, health behavior optimization, and quantitative risk assessment of HF.
References
- Virani SS, Alonso A, Benjamin EJ, et al. Heart disease and stroke statistics—2020 update: a report from the American Heart Association. Circulation 2020;141:e139-596.
- Benjamin EJ, Muntner P, Alonso A, et al. Heart disease and stroke statistics—2019 update: a report from the American Heart Association. Circulation 2019;139:e56–528.
- Uijl A, Koudstaal S, Vaartjes I, et al. Risk for heart failure: the opportunity for prevention with the American Heart Association's Life's Simple 7. JACC Heart Fail 2019;7:637–47.
- Hamo CE, Kwak L, Wang D, et al. Heart failure risk associated with severity of modifiable heart failure risk factors: the ARIC Study. J Am Heart Assoc 2022;11:e021583.
- Moore JX, Chaudhary N, Akinyemiju T. Metabolic syndrome prevalence by race/ethnicity and sex in the United States, National Health and Nutrition Examination Survey, 1988-2012. Prev Chronic Dis 2017;14:E24.
- Echouffo-Tcheugui JB, Ogunmoroti O, Golden SH, et al. Glycemic markers and heart failure subtypes: the Multi-Ethnic Study of Atherosclerosis (MESA). J Card Fail 2022;Jan 31:[Epub ahead of print].
- Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 2015;373:2117-28.
- Pham SV, Chilton RJ. EMPA-REG OUTCOME: the cardiologist's point of view. Am J Cardiol 2017;120:S53-S58.
- Cohen LP, Vittinghoff E, Pletcher MJ, et al. Association of midlife cardiovascular risk factors with the risk of heart failure subtypes later in life. J Card Fail 2021;27:435-44.
- Echouffo-Tcheugui JB, Zhang S, Florido R, et al. Duration of diabetes and incident heart failure: the ARIC (Atherosclerosis Risk In Communities) Study. JACC Heart Fail 2021;9:594-603.
- Florido R, Kwak L, Lazo M, et al. Six-year changes in physical activity and the risk of incident heart failure: ARIC study. Circulation 2018;137:2142-51.
- Lloyd-Jones DM, Braun LT, Ndumele CE, et al. Use of risk assessment tools to guide decision-making in the primary prevention of atherosclerotic cardiovascular disease: a special report from the American Heart Association and American College of Cardiology. J Am Coll Cardiol 2019;73:3153-67.
- Schwartz B, Pierce C, Vasan RS, et al. Lifetime risk of heart failure and trends in incidence rates among individuals with type 2 diabetes between 1995 and 2018. J Am Heart Assoc 2021;10:e021230.
- Staerk L, Wang B, Preis SR, et al. Lifetime risk of atrial fibrillation according to optimal, borderline, or elevated levels of risk factors: cohort study based on longitudinal data from the Framingham Heart Study. BMJ 2018;361:k1453.
Clinical Topics: Arrhythmias and Clinical EP, Cardiovascular Care Team, Diabetes and Cardiometabolic Disease, Dyslipidemia, Heart Failure and Cardiomyopathies, Prevention, Atrial Fibrillation/Supraventricular Arrhythmias, Lipid Metabolism, Nonstatins, Acute Heart Failure, Diet, Exercise, Hypertension, Smoking
Keywords: Sodium-Glucose Transporter 2 Inhibitors, Glycated Hemoglobin A, Cardiovascular Diseases, Aminophylline, Body Mass Index, Diabetes Mellitus, Type 2, American Heart Association, Prevalence, Atrial Fibrillation, Blood Pressure, Glycemic Control, Ethnic Groups, Metabolic Syndrome, Physicians, Primary Care, Risk Factors, Heart Disease Risk Factors, Heart Failure, Hospitalization, Risk Assessment, Hypertension, Atherosclerosis, Primary Prevention, Social Class, Exercise, Health Behavior, Risk Reduction Behavior, Primary Health Care, Cholesterol, Cardiology, Counseling, Delivery of Health Care, Life Style, Obesity, Smoking, Diet
< Back to Listings