Updated Approach to the Athlete With Chest Pain
Quick Takes
- The approach to the athlete with chest pain can differ significantly from the general population given the differing presentations and underlying etiologies as well as limitations of available testing modalities.
- Non-invasive imaging with coronary computed tomography angiography (CCTA) is now a Class IA recommendation in the workup for coronary artery disease (CAD) and is particularly favored in the younger population (age <65) where less obstructive CAD is suspected, such as the athletic population.
The etiology of chest pain in athletes often differs from the general population.1 Athletes typically have non-cardiac chest pain etiologies such as chest wall trauma, overuse injuries, gastroesophageal reflux disease, exercise induced bronchospasm or laryngeal obstruction. During the initial evaluation it remains essential to consider cardiac etiologies such as anomalous aortic origin of the coronary arteries (AAOCA), aortic dissection, myocardial bridging, or atherosclerotic coronary artery disease (CAD). Atherosclerotic disease remains the most common cause of sudden cardiac death (SCD) in athletes older than 35 years old.2 Furthermore, any athlete with a family member of unexplained death prior to the age of 50 should increase the suspicion for a genetic etiology of chest pain such as hypertrophic cardiomyopathy (HCM), arrhythmogenic right ventricular cardiomyopathy (ARVC), or connective tissue disorders.1
Ischemic chest pain in the athlete, much like the general population, is usually dull, squeezing or pressure-like, can last for several minutes, is worse with exertion, and relieves with rest. In addition, athletes with CAD can have warm up angina. If they continue exercising or stop and exercise soon after an initial warm up, the angina can resolve. The mechanism is thought to be secondary to arterial vasodilation and increased compliance.3 Non-ischemic chest pain, which is often sharp and occurs randomly, is usually more consistent with an inflammatory or non-cardiac etiology. It is essential to perform an accurate history and physical exam to determine the need for further cardiac testing.4,5
The latest chest pain guidelines (2021) moved away from describing chest pains as "typical" or "atypical," and emphasized the classification as "cardiac" or "non-cardiac" (Figure 1).6 The guidelines organize chest pain into acute or chronic and further stratify patients as low, intermediate, or high risk. The intermediate risk category is defined as patients who do not have evidence of acute myocardial injury by troponin but remain candidates for additional cardiac testing. The athlete population predominantly falls into the chronic low or intermediate risk population as they are more active and often more health conscious than the general population.7,8 By definition, they have a higher exercise threshold and low profile of co-morbidities in order to maintain a high level of performance.9
Figure 1
The workup for acute chest pain concerning for an acute coronary syndrome, aortic dissection, coronary dissection, cocaine abuse, myocarditis, pericarditis, or pulmonary embolism includes lab work, electrocardiogram (ECG), and transthoracic echocardiogram (TTE). In the intermediate to high pretest probability to groups, a stress test, CCTA, and/or cardiac catheterization may also be pursued.
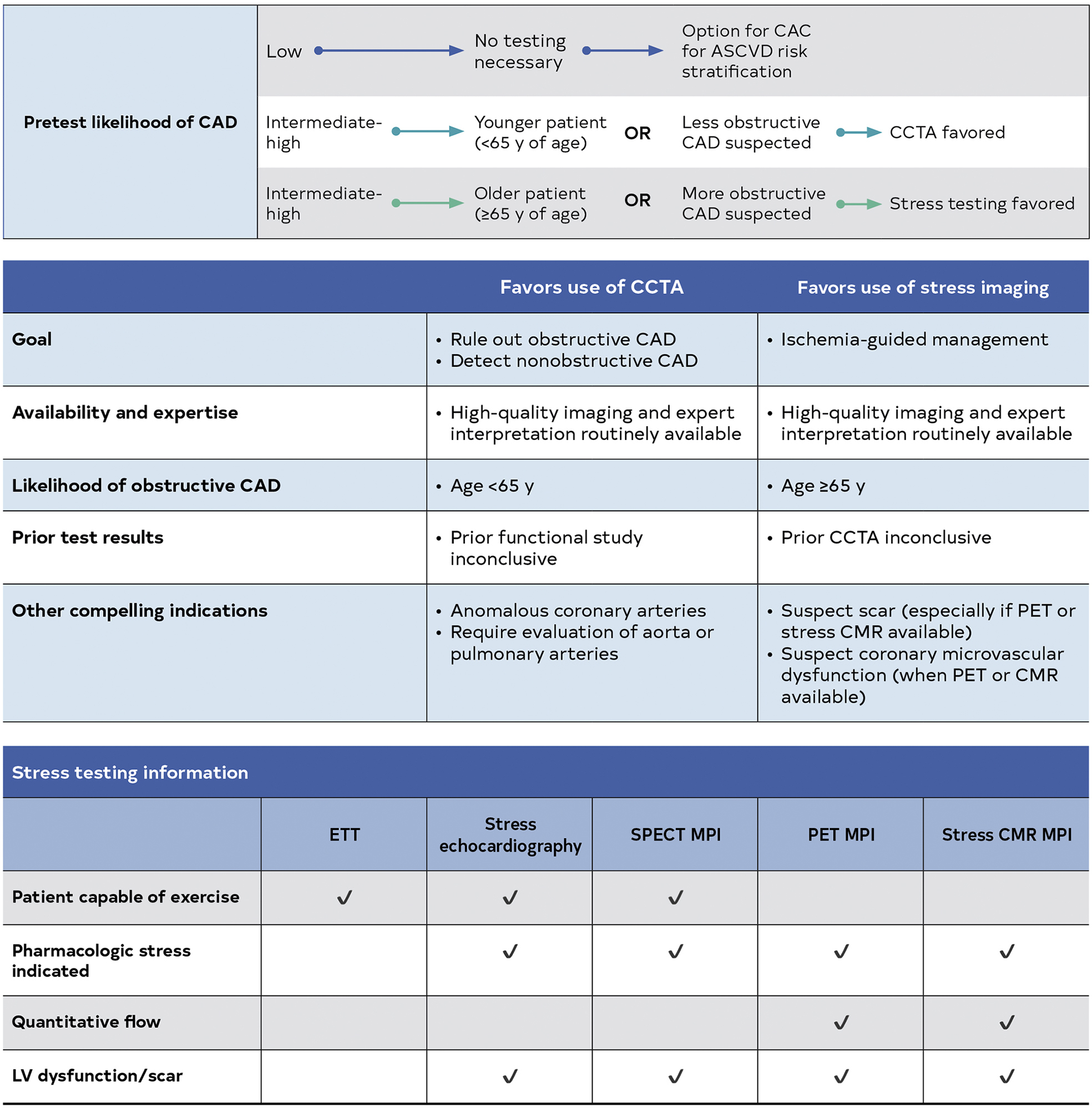
The recent guidelines distinguish coronary computed tomography angiography (CCTA) as the only Class 1A recommendation in the intermediate risk chest pain patient. As noted above, athletes typically fall into the low to intermediate risk population (<65 years old), thus the diagnostic workup should follow the same recommendations as the general population, which includes CCTA for the intermediate risk group (Figure 2).6 Furthermore, CCTA can provide superior prognostic value of the assessment of coronary atherosclerosis, as seen in PROMISE, Scot Heart, and the CONSERVE trial. CCTA provides an opportunity to exclude obstructive coronary disease and for the early identification of non-obstructive disease and initiation of preventive strategies including statins and intensification of risk factor modification.
Figure 2
ASCVD, atherosclerotic cardiovascular disease; CAD, coronary artery disease; CAC, coronary artery calcium; CCTA, coronary computed tomography angiography; CMR, cardiovascular magnetic resonance; ETT, exercise tolerance test; LV, left ventricular; MPI, myocardial perfusion imaging; PET, positron emission tomography and SPECT, single-photon emission computed tomography.
CCTA has proven cost effective compared to myocardial perfusion imaging (MPI) based on the CT-STAT trial.10 In the athlete with acute or chronic chest pain, if arterial etiology is likely, the early use of CCTA is reasonable. Fractional flow reserve – computed tomography (FFR-CT) can help distinguish obstructive disease, but this must be interpreted with caution as high intensity athletes can develop ischemia at higher baseline FFR values.11,12 Further research is needed to determine FFR thresholds in athletes.8
As a response to the hemodynamic stress of regular exercise, athletes may develop adaptations on the ECG. Such physiologic changes can contribute to false positive stress ECG testing.13-16 Thus stress testing with imaging or CCTA is often necessary.17-19
Anomalous aortic origin of the coronary arteries (AAOCA) are rare, occurring in 0.1-.0.7% of the general population.20,21 In the young athlete with chest pain it must be considered as a risk factor for SCD. AAOCA is often challenging to diagnose.22 In an experienced lab, TTE may be able to define the take-off of the coronary arteries, but in many cases a CCTA is needed to define the exact course.23 Cardiac magnetic resonance imaging (MRI) can also be used to define the arterial origin. Identifying high-risk features associated with AAOCA is challenging and best reserved for the most experienced institutions. The most concerning AAOCA is when the path of the left coronary comes off the right sinus of Valsalva and runs an interarterial course between the aorta and the pulmonary artery as this can lead to sudden cardiac arrest.21 An anomalous right coronary is more common and is most concerning when it has an interarterial course and is intramural with a slit like origin, which can be defined on CCTA. In such patients, further stress testing with imaging or FFR-CT can help exclude ischemia in the absence of symptoms.20-22
Conclusion
The 2021 chest pain guidelines are an excellent tool to define how to approach our chest pain patients. The multitude of etiologies of chest pain in athletes make the clinical and diagnostic assessment of chest pain challenging. The earlier adoption of CCTA in athletes at intermediate risk with acute or chronic chest pain is appropriate and consistent with the recent updated guidelines.
References
- Baggish AL, Battle RW, Beckerman JG, et al. Sports cardiology: core curriculum for providing cardiovascular care to competitive athletes and highly active people. J Am Coll Cardiol 2017;70:1902-18.
- Moran B, Bryan S, Farrar T, et al. Diagnostic evaluation of nontraumatic chest pain in athletes. Curr Sports Med Rep 2017;16:84-94.
- Williams RP, Manou-Stathopoulou V, Redwood SR, Marber MS. 'Warm-up Angina': harnessing the benefits of exercise and myocardial ischaemia. Heart 2014;100:106-14.
- McKinney J, Moulson N, Morrison BN, et al. Do athletes play by different rules? Obstructive coronary artery disease in asymptomatic competitive Masters athletes: a case series. Eur Heart J Case Rep 2020;4:1-5.
- Sik EC, Batt ME, Heslop LM. Atypical chest pain in athletes. Curr Sports Med Rep 2009;8:52-8.
- Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol 2021;78:2218-61.
- Borjesson M, Dellborg M, Niebauer J, et al. Recommendations for participation in leisure time or competitive sports in athletes-patients with coronary artery disease: a position statement from the Sports Cardiology Section of the European Association of Preventive Cardiology (EAPC). Eur Heart J 2019;40:13-18.
- Pelliccia A, Sharma S, Gati S, et al. 2020 ESC guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur Heart J 2021;42:17-96.
- Wells GD, Norris SR. Assessment of physiological capacities of elite athletes & respiratory limitations to exercise performance. Paediatr Respir Rev 2009;10:91-8.
- Goldstein JA, Chinnaiyan KM, Abidov A, et al. The CT-STAT (Coronary Computed Tomographic Angiography for Systematic Triage of Acute Chest Pain Patients to Treatment) trial. J Am Coll Cardiol 2011;58:1414-22.
- Issa OM, Inglessis-Azuaje I, Baggish AL. Coronary Fractional Flow Reserve in Endurance Athletes: The "Grey Zone" Between Supply and Demand. http://www.acc.org. Feb 20, 2019. Accessed 05/15/2022. https://www.acc.org/latest-in-cardiology/articles/2019/02/20/08/11/coronary-fractional-flow-reserve-in-endurance-athletes
- Kim JH, Malhotra R, Chiampas G, et al. Cardiac arrest during long-distance running races. N Engl J Med 2012;366:130-40.
- Knuuti J, Ballo H, Juarez-Orozco LE, et al. The performance of non-invasive tests to rule-in and rule-out significant coronary artery stenosis in patients with stable angina: a meta-analysis focused on post-test disease probability. Eur Heart J 2018;39:3322-30.
- Knuuti J, Wijns W, Saraste A, et al. 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J 2020;41:407-77.
- van de Sande DA, Breuer MA, Kemps HM. Utility of exercise electrocardiography in pre-participation screening in asymptomatic athletes: a systematic review. Sports Med 2016;46:1155-64.
- van de Sande DA, Hoogeveen A, Hoogsteen J, Kemps HM. The diagnostic accuracy of exercise electrocardiography in asymptomatic recreational and competitive athletes. Scand J Med Sci Sports 2016;26:214-20.
- Drezner JA, Sharma S, Baggish A, et al. International criteria for electrocardiographic interpretation in athletes: consensus statement. Br J Sports Med 2017;51:704-31.
- Petek BJ, Drezner JA, Prutkin JM, Owens DS, Tran T, Harmon KG. Electrocardiogram interpretation in college athletes: local institution versus sports cardiology center interpretation. J Electrocardiol 2020;62:49-56.
- Weiss M, Rao P, Johnson D, et al. Physician adherence to 'Seattle' and 'International' ECG criteria in adolescent athletes: an analysis of compliance by specialty, experience, and practice environment. J Electrocardiol 2020;60:98-101.
- Finocchiaro G, Behr ER, Tanzarella G, et al. Anomalous coronary artery origin and sudden cardiac death: clinical and pathological insights from a National Pathology Registry. JACC Clin Electrophysiol 2019;5:516-22.
- Borns J, Gräni C, Kadner A, Gloeckler M, Pfammatter JP. Symptomatic coronary anomalies and ischemia in teenagers - rare but real. Front Cardiovasc Med 2020;7:559794.
- Gräni C, Kaufmann PA, Windecker S, Buechel RR. Diagnosis and management of anomalous coronary arteries with a malignant course. Interv Cardiol 2019;14:83-88.
- Baggish AL, Battle RW, Beaver TA, et al. Recommendations on the use of multimodality cardiovascular imaging in young adult competitive athletes: a report from the American Society of Echocardiography in collaboration with the Society of Cardiovascular Computed Tomography and the Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr 2020;33:523-49.
Clinical Topics: Acute Coronary Syndromes, Arrhythmias and Clinical EP, Cardiovascular Care Team, Diabetes and Cardiometabolic Disease, Dyslipidemia, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Pericardial Disease, Prevention, Sports and Exercise Cardiology, Vascular Medicine, Atherosclerotic Disease (CAD/PAD), Genetic Arrhythmic Conditions, SCD/Ventricular Arrhythmias, Nonstatins, Novel Agents, Statins, Interventions and ACS, Interventions and Coronary Artery Disease, Interventions and Imaging, Interventions and Structural Heart Disease, Interventions and Vascular Medicine, Computed Tomography, Magnetic Resonance Imaging, Nuclear Imaging, Exercise, Sports and Exercise and Congenital Heart Disease and Pediatric Cardiology, Sports and Exercise and ECG and Stress Testing, Sports and Exercise and Imaging
Keywords: Coronary Artery Disease, Fractional Flow Reserve, Myocardial, Computed Tomography Angiography, Hydroxymethylglutaryl-CoA Reductase Inhibitors, Acute Coronary Syndrome, Myocardial Perfusion Imaging, Exercise Test, Arrhythmogenic Right Ventricular Dysplasia, Asthma, Exercise-Induced, Cocaine-Related Disorders, Cost-Benefit Analysis, Myocardial Bridging, Myocardial Bridging, Myocarditis, Physical Exertion, Pulmonary Artery, Sinus of Valsalva, Thoracic Wall, Vasodilation, Chest Pain, Electrocardiography, Cardiac Catheterization, Risk Factors, Cardiomyopathy, Hypertrophic, Gastroesophageal Reflux, Magnetic Resonance Imaging, Death, Sudden, Cardiac, Pulmonary Embolism, Aneurysm, Dissecting, Connective Tissue, Cumulative Trauma Disorders, Exercise, Physical Examination, Pericarditis, Morbidity, Ischemia, Troponin, Athletes, Sports, Sports Medicine
< Back to Listings