Emerging Techniques For Cardiovascular Risk Assessment and Prevention
Quick Takes
- CAC scoring is an important tool recommended for risk stratification in patients with borderline to intermediate 10-year ASCVD risk.
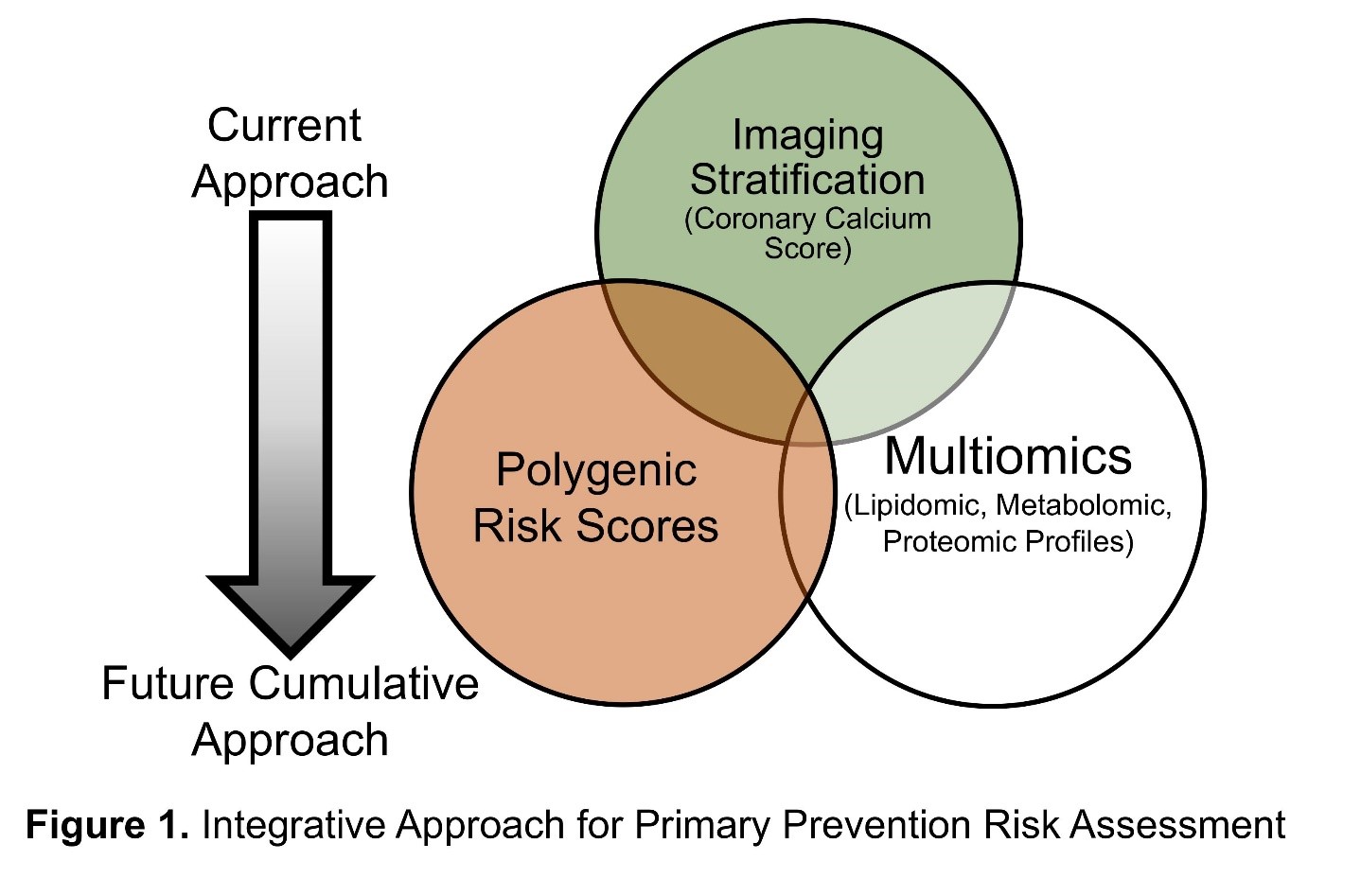
- Polygenic risk scoring and multi-omics are emerging technologies which will become increasingly available in the next few years and may improve risk stratification in combination with CAC or identify patients who might benefit from CAC scoring at an early age.
- Although multiple potential roles of polygenic risk scoring and multi-omics have been suggested, where these techniques might fit into the paradigm of ASCVD risk assessment and prevention by the end of this decade remains an open question for further research.
Commentary based on: Verma KP, Inouye M, Meikle PJ, Nicholls SJ, Carrington MJ, Marwick TH. New cardiovascular risk assessment techniques for primary prevention: JACC Review Topic of the Week. J Am Coll Cardiol 2022;80:373-87.1
Introduction
Public health policies such as elimination of trans fats, reduction in cigarette smoking, and pharmacological and technological advances have decreased atherosclerotic cardiovascular disease (ASCVD) mortality dramatically over the last 70 years. However, the prevalence of obesity, metabolic syndrome, and type 2 diabetes have increased during the past 20 years, and it is estimated there will be a 30% increase in prevalence of CVD by the year 2060.2 ASCVD risk scores using traditional risk factors are the foundation for ASCVD risk estimation and to guide preventive therapy (e.g., statin, antihypertensive, aspirin). However, they are imperfect and may underestimate risk in certain populations including younger patients with a family history of premature ASCVD, those of lower socioeconomic status, or those with chronic inflammatory disorders.
Imaging an individual's burden of subclinical atherosclerosis via coronary artery calcium (CAC) scoring significantly improves risk prediction beyond traditional risk factors, and emerging approaches such as polygenic risk scoring (PRS) and multi-omic strategies hold promise for further refining an individual's ASCVD risk prediction. Determining which patients have the highest utility from each of these tests can help facilitate more individualized risk assessment and thereby guide appropriate preventive management.
Imaging Stratification
CAC testing detects subclinical coronary artery disease (CAD), and a higher CAC burden is associated with a significantly higher risk for ASCVD. CAC scoring is currently recommended for use in asymptomatic individuals with borderline to intermediate (5-19.9%) 10-year ASCVD risk to improve ASCVD risk stratification. CAC is superior to traditional risk factors in predicting ASCVD outcomes and improves risk prediction beyond the pooled cohort equations (PCE).3,4 Accordingly, the 2018 American Heart Association (AHA)/American College of Cardiology (ACC) cholesterol guideline and 2019 ACC/AHA primary prevention guideline favor initiating statin therapy for patients with a CAC score of 1-99 and recommend initiation of statin therapy. Conversely, the absence of CAC (CAC=0) portends a very low 10-year event even among statin eligible patients who do not smoke.5,6
However, determining the ideal age to first perform CAC scoring and identifying young patients <40 years old with a high utility of CAC scoring is less certain given the generally low prevalence of CAC >0 in this age group. Selection of young patients with a high risk factor burden and/or the presence of risk enhancing factors can be considered, although many of these individuals will still have CAC=0.7 The identification of carotid plaque by ultrasonography is associated with incident CAC and somewhat increased CVD risk. However, it can be challenging to accurately measure carotid intimal thickness or identify small amounts of carotid plaque outside of a research lab as a skilled and experienced ultrasonographer is generally required.
Polygenic Risk Scores
Several genetic variants, typically single nucleotide polymorphisms, identified in genome-wide associated studies have been associated with increased lifetime risk of CAD. Genome-wide genotyping will become increasingly available and PRS based on these studies may be used to estimate risk.8 A multitude of scoring systems exist which have been shown to predict risk in large cohorts and a polygenic risk catalog has been established to enable direct comparison between scores.8
In the future, PRS may help to identify patients who will derive greater benefit from pharmacotherapy. PRS datasets have notably been validated for the prediction of symptomatic CAD but not for asymptomatic subclinical coronary atherosclerosis.9 Additionally, while genome-wide association study (GWAS) studies have identified mutations that predict both acute coronary syndrome (ACS) and CAC, certain loci are associated with one or the other.10 Therefore, PRS is still primarily used as a research tool and there are no US Food and Drug Administration (FDA) approved PRS scores for clinical use.
As such, the use of PRS may eventually be complementary to CAC rather than redundant and this may eventually be more useful than using CAC alone as a population screening tool for identifying risk. Moreover, PRS might be used to identify younger individuals at higher risk for CAC who might benefit from earlier CAC screening.11 Limitations include the challenge of obtaining a standard PRS at commercial labs. Additionally, much of the data used to determine PRS is derived from Eurocentric populations.
Multiomics
Omics is biotechnology which analyzes large amounts of data representing a set of biological molecules including proteins, lipids, and metabolites, among others, and translates this data into the structure, function, and dynamics of an organism.12 Metabolic markers such as amino acids, fats, and proteins can be quantified using techniques such as nuclear magnetic resonance (NMR), mass-spectrometry or immunoassays. These can be summated to create a risk profile for diseases including atherosclerosis.13
NMR can be used to capture large measures of lipoproteins, metabolites, and proteins along with their size and composition in tandem to create an individual profile used to estimate risk. Lipidomic profiles have shown improvement over traditional risk factors in identifying patients at risk of CAD and can now be generated rapidly and accurately to analyze large cohorts.14,15 They can also be applied to generate metabolite or protein profiles.
Several metabolites have been identified which are associated with increased risk of incident CVD.16 Additionally, both coronary and carotid atherosclerosis have been associated with disturbances in particular inter-connected metabolic pathways, which have in turn been associated with incident cardiovascular events.17
Metabolomic profiles can be similarly used to assess CAD risk and study the effects of diet and pharmacological intervention on various metabolic pathways.18 Proteomic profiles might be used to capture the expanse of molecules implicated in atherosclerosis such as inflammatory and lipid-related proteins.19 This method of analyzing risk is limited by ability to scale and it is notable that the specific lipid and protein species associated with CVD vary between cohorts and may be altered by diet and pharmacological intervention.
Integrated Approach
Strengths and weaknesses exist for each method of estimating cardiovascular risk and their use in combination may eventually provide a better strategy for ASCVD risk assessment. CAC significantly improves risk prediction beyond traditional risk factors and is guideline recommended to improve CVD risk prediction for borderline to intermediate risk patients. Identifying which young patients under the age of 40 have a higher utility for CAC scoring is a topic of ongoing research. Where each method fits into stratifying CVD risk remains an open question. PRS and omics may be useful tools in the future to identify persons at increased risk for subclinical atherosclerosis who may benefit from CAC scoring at an early age to help determine the need for statin therapy and more aggressive lifestyle modification.
Figure 1
References
- Verma KP, Inouye M, Meikle PJ, Nicholls SJ, Carrington MJ, Marwick TH. New cardiovascular risk assessment techniques for primary prevention. J Am Coll Cardiol 2022;80:373-87.
- Mohebi R, Chen C, Ibrahim NE, et al. Cardiovascular disease projections in the United States based on the 2020 Census estimates. J Am Coll Cardiol 2022;80:565-78.
- Nasir K, Bittencourt MS, Blaha MJ, et al. Implications of coronary artery calcium testing among statin candidates according to American College of Cardiology/American Heart Association cholesterol management guidelines: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol 2015;66:1657-68.
- McClelland RL, Jorgensen NW, Budoff M, et al. 10-year coronary heart disease risk prediction using coronary artery calcium and traditional risk factors: derivation in the MESA (Multi-Ethnic Study of Atherosclerosis) with validation in the HNR (Heinz Nixdorf Recall) study and the DHS (Dallas Heart Study). J Am Coll Cardiol 2015;66:1643-53.
- Budoff MJ, Young R, Burke G, et al. Ten-year association of coronary artery calcium with atherosclerotic cardiovascular disease (ASCVD) events: the multi-ethnic study of atherosclerosis (MESA). Eur Heart J 2018;39:2401-08.
- Razavi AC, Kelly TN, Budoff MJ, et al. Atherosclerotic cardiovascular disease events among statin eligible individuals with and without long-term healthy arterial aging. Atherosclerosis 2021;326:56-62.
- Patel J, Pallazola VA, Dudum R, et al. Assessment of coronary artery calcium scoring to guide statin therapy allocation according to risk-enhancing factors: the Multi-Ethnic Study of Atherosclerosis. JAMA Cardiol 2021;6:1161-70.
- Inouye M, Abraham G, Nelson CP, et al. Genomic risk prediction of coronary artery disease in 480,000 adults: implications for primary prevention. J Am Coll Cardiol 2018;72:1883-93.
- Deloukas P, Kanoni S, Willenborg C, et al. Large-scale association analysis identifies new risk loci for coronary artery disease. Nat Genet 2013;45:25-33.
- O'Donnell CJ, Kavousi M, Smith AV, et al. Genome-wide ssociation study for coronary artery calcification with follow-up in myocardial infarction. Circulation 2011;124:2855-64.
- Severance LM, Carter H, Contijoch FJ, McVeigh ER. Targeted coronary artery calcium screening in high-risk younger individuals using consumer genetic screening results. JACC Cardiovasc Imaging 2021;14:1398-1406.
- Doran S, Arif M, Lam S, et al. Multi-omics approaches for revealing the complexity of cardiovascular disease. Brief Bioinform 2021;22:bbab061.
- Huynh K, Barlow CK, Jayawardana KS, et al. High-throughput plasma lipidomics: detailed mapping of the Associations with Cardiometabolic Risk Factors. Cell Chem Biol 2019;26:71-84.e4.
- Mundra PA, Barlow CK, Nestel PJ, Bet al. Large-scale plasma lipidomic profiling identifies lipids that predict cardiovascular events in secondary prevention. JCI Insight 2018;3:e121326.
- Alshehry ZH, Mundra PA, Barlow CK, et al. Plasma lipidomic profiles improve on traditional risk factors for the prediction of cardiovascular events in type 2 diabetes mellitus. Circulation 2016;134:1637-50.
- Cavus E, Karakas M, Ojeda FM, et al. Association of circulating metabolites with risk of coronary heart disease in a European population. JAMA Cardiol 2019;4:1270-79.
- Tzoulaki I, Castagné R, Boulangé CL, et al. Serum metabolic signatures of coronary and carotid atherosclerosis and subsequent cardiovascular disease. Eur Heart J 2019;40:2883-96.
- Würtz P, Raiko JR, Magnussen CG, et al. High-throughput quantification of circulating metabolites improves prediction of subclinical atherosclerosis. Eur Heart J 2012;33:2307-16.
- Hoogeveen RM, Pereira JPB, Nurmohamed NS, et al. Improved cardiovascular risk prediction using targeted plasma proteomics in primary prevention. Eur Heart J 2020;41:3998-4007.
Clinical Topics: Acute Coronary Syndromes, Arrhythmias and Clinical EP, Cardiovascular Care Team, Diabetes and Cardiometabolic Disease, Dyslipidemia, Noninvasive Imaging, Prevention, Vascular Medicine, Atherosclerotic Disease (CAD/PAD), Lipid Metabolism, Nonstatins, Novel Agents, Statins, Echocardiography/Ultrasound, Diet, Smoking
Keywords: Coronary Artery Disease, Genome-Wide Association Study, Hydroxymethylglutaryl-CoA Reductase Inhibitors, Cardiovascular Diseases, Calcium, Antihypertensive Agents, Prevalence, Acute Coronary Syndrome, American Heart Association, Cigarette Smoking, Diabetes Mellitus, Type 2, Genotype, Lipidomics, Metabolic Syndrome, Polymorphism, Single Nucleotide, Proteomics, United States Food and Drug Administration, Risk Factors, Heart Disease Risk Factors, Atherosclerosis, Risk Assessment, Primary Prevention, Cholesterol, Magnetic Resonance Spectroscopy, Carotid Artery Diseases, Metabolic Networks and Pathways, Mass Spectrometry, Health Policy, Ultrasonography, Biotechnology, Immunoassay, Lipoproteins, Amino Acids, Life Style, Aspirin, Obesity, Lipids, Diet
< Back to Listings