Electronic Health Tools to Help Adolescent Patients With CHD Transition to an Adult Model of Care
Quick Takes
- Health care transition is a vital component of the treatment of adolescents and young adults with CHD.
- Electronic health tools offer easily updatable, portable, and translatable education to patients and families that can be shared with other providers. These tools also allow centers to track patient outcomes and promote delivery of education.
- This transition program may serve as a model for other institutions developing their own transition education programs.
Introduction
An increasing number of patients with congenital heart disease (CHD) are surviving to adulthood.1,2 Today, there are more adult than pediatric patients with CHD.3 There is consensus that transition education programs (TEPs) should be in place to empower adolescent patients to become successful and independent participants in the adult healthcare system.1,3 The timing and nature of transition education and transfer of care must be individualized based on the emotional and mental maturity and readiness of patients and their caregivers.1,3 Recent consensus statements emphasize the importance of transition education and highlight the risks which arise from a lack of formal TEPs, including gaps in cardiology care which can lead to public health costs to the medical infrastructure and negative impacts on the quality of life of patients, their families, physicians, and other healthcare providers.1,3,4 A formal TEP can mitigate some of these barriers and ensure successful transfer of care.1,3,4 There is some evidence that adoption of electronic tools can facilitate transition and support adolescents.5
Rationale for Transition Programs:
TEPs provide benefits including:
- Enabling adolescents to make informed decisions regarding care through knowledge gained
- Initiating practices that promote independence in seeking healthcare
- Offering opportunities to enroll in an adult insurance plan or Medicaid to ensure there is no interruption in coverage or care
- Reducing healthcare costs
- Becoming an established patient of an adult CHD physician to reduce gaps in follow-up
Transition Program
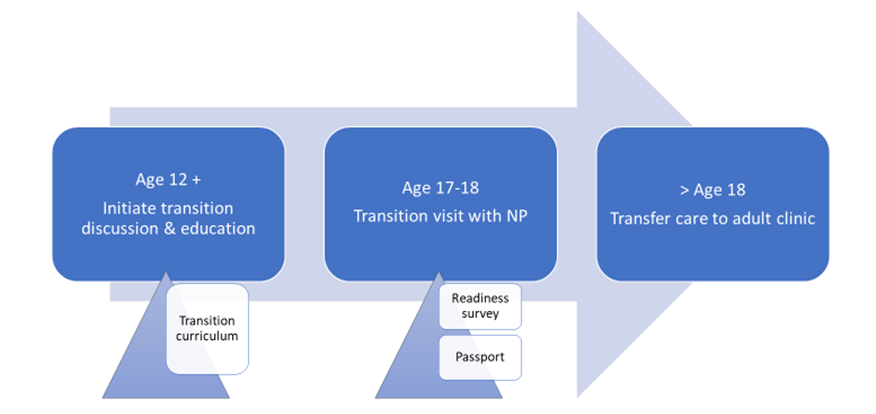
We highlight a TEP that promotes transfer of care from pediatric cardiology to adult cardiology using electronic health tools (Figure 1). This program includes a transition policy, tracking and monitoring, readiness assessment, patient education and transfer of care in keeping with recent practice based guidelines.4 Starting at about age 12 and culminating at time of transfer of care at >18 years of age, patients needing transition education are identified. An order is entered in the electronic medical record (EMR) which signals their enrolment status in the chart, prompting a coordinator and /or transition medical director to add the patient to a transition database/dashboard. Maintaining a transition database allows the center to track patients and document achievement of pre-determined goals and outcomes.
Figure 1: Outline of Transition Program
Electronic prompts in the EMR cue pediatric cardiologists and other members of the team to initiate transition education. A formal educational curriculum smart phrase can be used to lead discussions with patients and families on transition topics as outlined in the transition curriculum (Figure 2). This allows the clinician to document education provided during the encounter.
Figure 2: Transition Curriculum
At age 17 to 18, a face-to-face or virtual visit with an advanced practice provider or transition coordinator may be scheduled, during which readiness surveys are administered to assess patient knowledge gaps. The readiness survey may be sent to the patient electronically using EMR portal, and communication tools with the results tracked in the transition database.
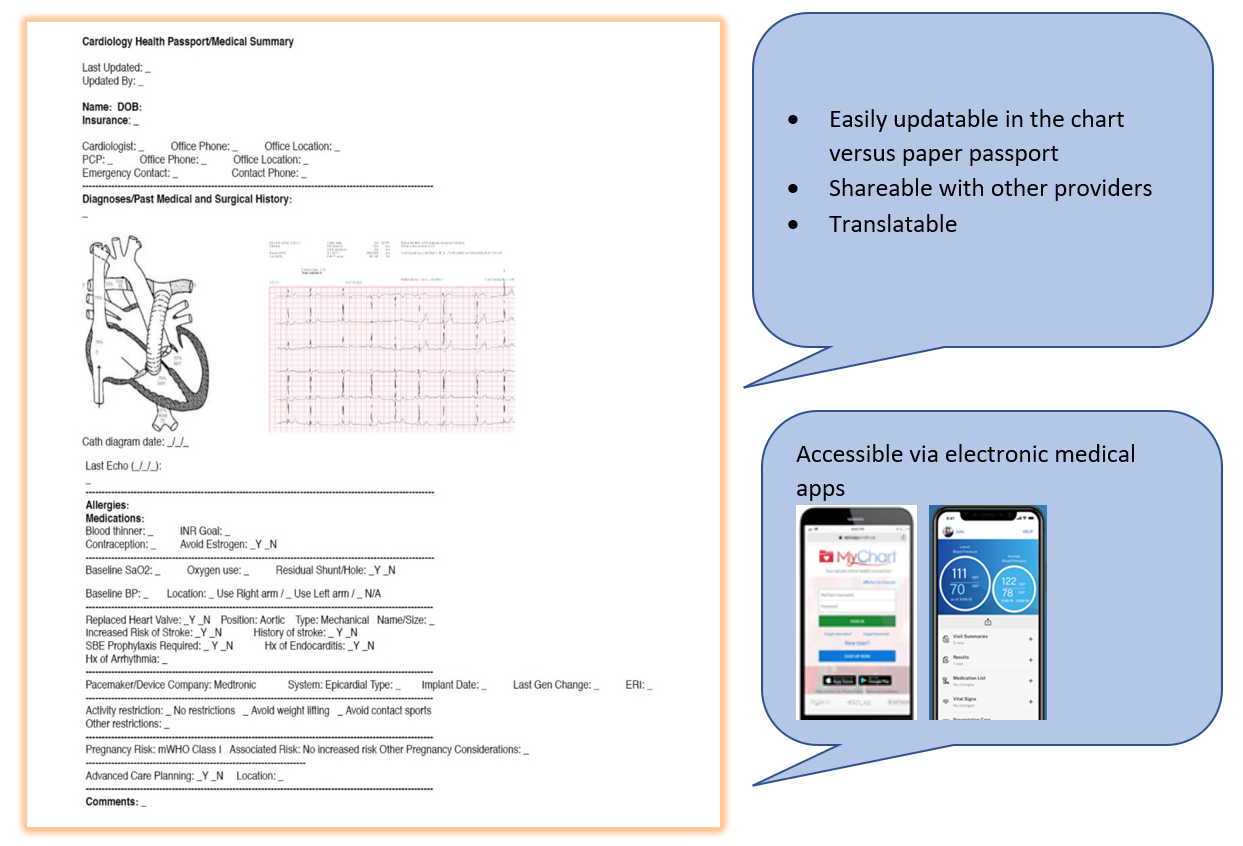
The authors advocate for use of a "virtual health passport" (Figure 3), created in the patient's EMR that can be accessed by the patient using the medical system's healthcare applications (i.e., Epic, MyChart, iCentra, MyHealth). The virtual passport can also be downloaded and stored digitally on a mobile device, allowing portability and ease of accessibility. Patients are thereby able to show it to other providers that may not be in their current system (i.e., emergency room provider). The health passport can be easily updated and "smart links" within the passport allow instantaneous updating of medications and diagnoses.
Figure 3: Virtual Health Passport
Conclusion
A robust and well-supported transition program is vital for any CHD program. A successful program can decrease knowledge gaps, reduce patients lost to follow-up, and educate and empower adolescents and young adults to become independent and successfully navigate the healthcare system. Incorporating technology and electronic health tools can facilitate the creation of a transition program and educate patients.
References
- Moons P, Bratt EL, De Backer J, et al. Transition to adulthood and transfer to adult care of adolescents with congenital heart disease: a global consensus statement of the ESC Association of Cardiovascular Nursing and Allied Professions (ACNAP), the ESC Working Group on Adult Congenital Heart Disease (WG ACHD), the Association for European Paediatric and Congenital Cardiology (AEPC), the Pan-African Society of Cardiology (PASCAR), the Asia-Pacific Pediatric Cardiac Society (APPCS), the Inter-American Society of Cardiology (IASC), the Cardiac Society of Australia and New Zealand (CSANZ), the International Society for Adult Congenital Heart Disease (ISACHD), the World Heart Federation (WHF), the European Congenital Heart Disease Organisation (ECHDO), and the Global Alliance for Rheumatic and Congenital Hearts (Global ARCH). Eur Heart J 2021;42:4213-23.
- de Hosson M, De Backer J, De Wolf D, et al. Development of a transition program for adolescents with congenital heart disease. Eur J Pediatr 2020;179:339–48.
- John AS, Jackson JL, Moons P, et al. Advances in managing transition to adulthood for adolescents with congenital heart disease: a practical approach to transition program design: a scientific statement from the American Heart Association. J Am Heart Assoc 2022;11:e025278.
- White PH, Cooley WC, Transitions Clinical Report Authoring Group, American Academy of Pediatrics, American Academy of Family Physicians, American College of Physicians. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics 2018;143:e20183610.
- Low JK, Manias E. Use of technology-based tools to support adolescents and young adults with chronic disease: systematic review and meta-analysis. JMIR Mhealth Uhealth 2019;7:e12042.
Clinical Topics: Congenital Heart Disease and Pediatric Cardiology, Congenital Heart Disease, CHD and Pediatrics and Quality Improvement
Keywords: Adolescent, Young Adult, Child, Quality of Life, Electronic Health Records, Caregivers, Follow-Up Studies, Medicaid, Physician Executives, Public Health, Delivery of Health Care, Heart Defects, Congenital, Communication, Health Care Costs, Emergency Service, Hospital, Electronics, Technology, Pediatrics
< Back to Listings