Impact of an Organized Treatment Pathway With Electrophysiology Emergency Room Consultation to Manage Atrial Fibrillation
Quick Takes
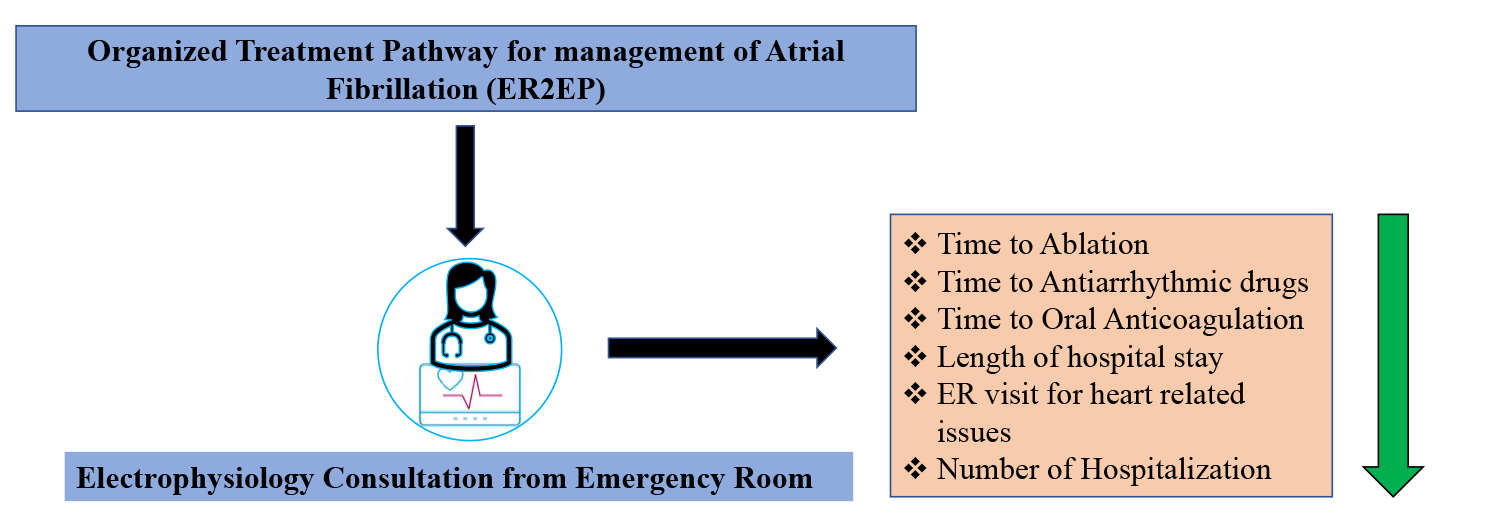
- Adapting an organized treatment pathway with electrophysiology consultation from the emergency room (ER) led to significantly lower times for definitive treatment of atrial fibrillation.
- At 12-month follow up, patients with an organized treatment approach had a lower rate of hospitalization, congestive heart failure and ER visits.
- Improving length of stay and subsequent hospitalizations could lead to significant economic relief to the patient and health care systems.
The increasing prevalence of atrial fibrillation (AF) worldwide is considered an epidemic leading to a significant economic burden on patients and the health care systems.1-3 Most patients with AF are often evaluated in emergency room (ER) with recurrent symptoms impairing their quality of life. As the treatment is usually at the discretion of the treating ER physician, there seems to be a significant variation in practice patterns. Prior study has reported variations in selecting rate versus rhythm control, initiation of oral anticoagulation (OAC) for stroke prevention, appropriate and timely use of antiarrhythmic drugs (AAD), and even cardiology versus electrophysiology (EP) consultations.4 In contemporary practice, early rhythm control with catheter ablation and AAD strategy was associated with reduction in mortality, stroke, and heart failure hospitalizations,5,6 with superiority of catheter ablation over AAD in terms of AF recurrence.7 In addition, OAC, considered the cornerstone of AF management for stroke prevention, is often underutilized, with delay in drug initiation (median time 5 days, IQR 1 - 43 days).8 Therefore, there remains an unmet need to standardize practice patterns starting from the ER, which can lead to improved treatment outcomes and, in turn, decrease the overall healthcare burden.
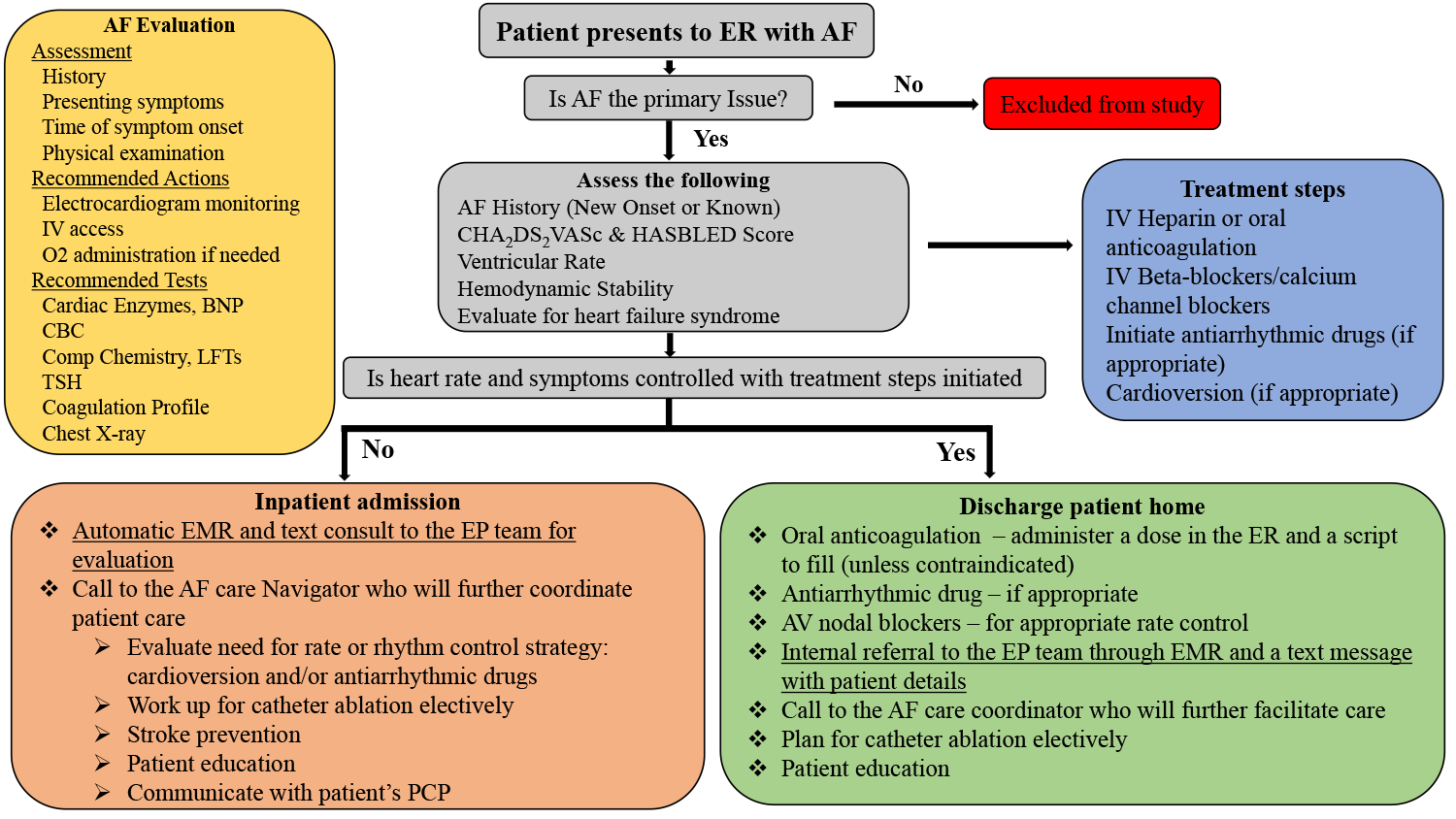
In this multicenter study, we hypothesized that initiating an appropriate, standardized referral protocol involving the EP service could significantly improve access to care and reduce AF-related complications and hospitalizations. The preliminary findings of the paper were presented as a late breaker clinical trial at Heart Rhythm Society Scientific Sessions, San Francisco, 2022 (Figure 1).9
Figure 1
ER=Emergency Room, AF=Atrial Fibrillation, ECG=Electrocardiogram, IV= Intravenous access, O2=Oxygen, CBC=Complete blood counts, LFTs=Liver function tests, TSH=thyroid stimulating hormone, PCP=Primary care physician
In our prospective, multi-center observational study, a total of 400 patients were included (200 in the organized treatment pathway or ER2EP group [Figure 1] vs. 200 in the control group) with a primary diagnosis of new-onset AF that presented to ER from 2019 to 2021. Overall in our study, 52% were men, and the mean age was 72±1 years. The two groups were well balanced with respect to major baseline demographics, except patients in the ER2EP arm were older, predominantly men, and had increased prevalence of persistent AF compared to the control arm. Of 400 patients included in the study, 42.5% of the patients (n=170) underwent AF ablation (45.5% [n=91] in ER2EP group vs. 39.5% [n=79] in the control group, p≤0.001). There was a significant reduction in time to first EP evaluation (median 1 day [range 1-24 days] vs. median 128 days [range 30-340 days] in the control group, p=0.001). All patients in the ER2EP group had EP evaluation versus 46% in the control group (p≤0.001). We demonstrated a significant reduction in time to OAC initiation (1.7±13 vs. 17±64 days, p=0.002), AAD initiation (2.7±12.1 vs. 25±7 days, p<0.001), and mean time to ablation (52.8±43.6 vs. 180.6±70 days, p<0.001) in the ER2EP group compared to control group, respectively. As such, this resulted in reduced length of stay (LOS) in the ER2EP group compared to the control group (2.3±2.5 vs. 5.8±6.3 days, p<0.001). Furthermore, the ER visit for heart-related issues and the number of hospitalizations was significantly lower in the ER2EP group than in the control group, with a signal toward non-statistical reduction in congestive heart failure and stroke (Table 1).
Table 1
| Outcomes (Days) | ER2EP Group | Control group | P value |
| Time to EP evaluation (median) | 1 (range 1-24 days) | 128 (range 30-340 days) | 0.001 |
| Time to Ablation | 52.8 ± 43.6 | 180.6 ± 70 | < 0.001 |
| Time to Antiarrhythmic drugs | 2.7 ± 12.1 | 25 ± 7 | <0.001 |
| Time to Oral Anticoagulation | 1.7 ± 13 | 17 ± 64 | 0.002 |
| Length of Stay | 2.3 ± 2.5 | 5.8 ± 6.3 | <0.001 |
| ER visit for Heart-related issues | 9 (5%) | 20 (10%) | <0.001 |
| Number of Hospitalization | 1 ± 0.9 | 1.5 ± 1.7 | <0.001 |
| Congestive heart failure | 8 (4%) | 16 (8%) | 0.05 |
| Stroke | 10 (5.5%) | 15 (7.5%) | 0.53 |
We acknowledge that this is a prospective non-randomized study, therefore, there remains a risk of bias among the participating sites (high-volume, busy cardiac EP centers), which may have expedited the overall course of treatment in both groups. The differences in outcomes between the two groups may be even more significant in less organized facilities where the emphasis on care pathways is not stressed as much. In addition, the significantly higher number of persistent AF patients in the ER2EP group could potentially account for the aggressive treatment approach compared to the control group. A randomized multicenter trial is needed to further validate our study's findings.
In conclusion, the ER2EP study serves as a stepping stone and a strong advocate for adapting an organized treatment pathway and immediate EP consultation for the management of AF. Moreover, the findings of our study align with prior studies demonstrating significant delays in the treatment initiation for the management of AF in the control group, highlighting the need for a better treatment pathway and referral process. Also, in the current era, where LOS is used as a surrogate for resource utilization and overall efficiency of the health care system,10 reduction in LOS, hospital readmission, and ER visits might help reduce overall patient morbidity and mortality.
Figure 2
References
- Savelieva I, Camm J. Update on atrial fibrillation: part I. Clin Cardiol 2008;31:55-62.
- National Center for Health Statistics Mortality Data on CDC WONDER (CDC website). 2022. Available at: https://wonder.cdc.gov/mcd.html. Accessed 08/01/2022.
- Benjamin EJ, Muntner P, Alonso A, et al. Heart Disease and Stroke Statistics-2019 update: a report from the American Heart Association. Circulation 2019;139:e56-e528.
- Scheuermeyer FX, Innes G, Pourvali R, et al. Missed opportunities for appropriate anticoagulation among emergency department patients with uncomplicated atrial fibrillation or flutter. Ann Emerg Med 2013;62:557-65.e2.
- Kirchhof P, Camm AJ, Goette A, et al. Early rhythm-control therapy in patients with atrial fibrillation. N Engl J Med 2020;383:1305-16.
- Turagam MK, Garg J, Whang W, et al. Catheter ablation of atrial fibrillation in patients with heart failure: a meta-analysis of randomized controlled trials. Ann Intern Med 2019;170:41-50.
- Turagam MK, Musikantow D, Whang W, et al. Assessment of catheter ablation or antiarrhythmic drugs for first-line therapy of atrial fibrillation: a meta-analysis of randomized clinical trials. JAMA Cardiol 2021;6:697-705.
- Khurshid S, Weng LC, Hulme OL, Ellinor PT, Lubitz SA. Factors associated with anticoagulation delay following new-onset atrial fibrillation. Am J Cardiol 2017;120:1316-21.
- Lakkireddy D, Ahmed A , Garg J, et al. Clinical and economic impact of an organized treatment pathway on atrial fibrillation patient from the emergency room to electrophysiology service (ER2EP Study). Presented at Heart Rhythm Society Scientific Sessions, San Francisco, CA. 2022.
- Marfil-Garza BA, Belaunzarán-Zamudio PF, Gulias-Herrero A, et al. Risk factors associated with prolonged hospital length-of-stay: 18-year retrospective study of hospitalizations in a tertiary healthcare center in Mexico. PLoS One 2018;13:e0207203.
Clinical Topics: Anticoagulation Management, Arrhythmias and Clinical EP, Heart Failure and Cardiomyopathies, Anticoagulation Management and Atrial Fibrillation, Implantable Devices, EP Basic Science, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Acute Heart Failure
Keywords: Atrial Fibrillation, Anti-Arrhythmia Agents, Follow-Up Studies, Quality of Life, Prevalence, Length of Stay, Catheter Ablation, Anticoagulants, Stroke, Treatment Outcome, Heart Failure, Emergency Service, Hospital, Delivery of Health Care, Electrophysiology, Referral and Consultation, Prospective Studies, Control Groups, Health Services Accessibility, Observational Studies as Topic, Multicenter Studies as Topic, Patient Readmission, Morbidity, Critical Pathways
< Back to Listings