An Analysis of ISCHEMIA and ISCHEMIA-CKD Outcomes by Chronic Kidney Disease Stage
Quick Takes
- In patients with stable coronary artery disease and chronic kidney disease, an initial conservative approach is non-inferior to an initial invasive approach.
- Invasive management for patients with stable coronary artery disease and less-advanced chronic kidney disease may improve quality of life.
- Higher stages of chronic kidney disease are associated with higher rates of cardiovascular events in patients with chronic coronary disease.
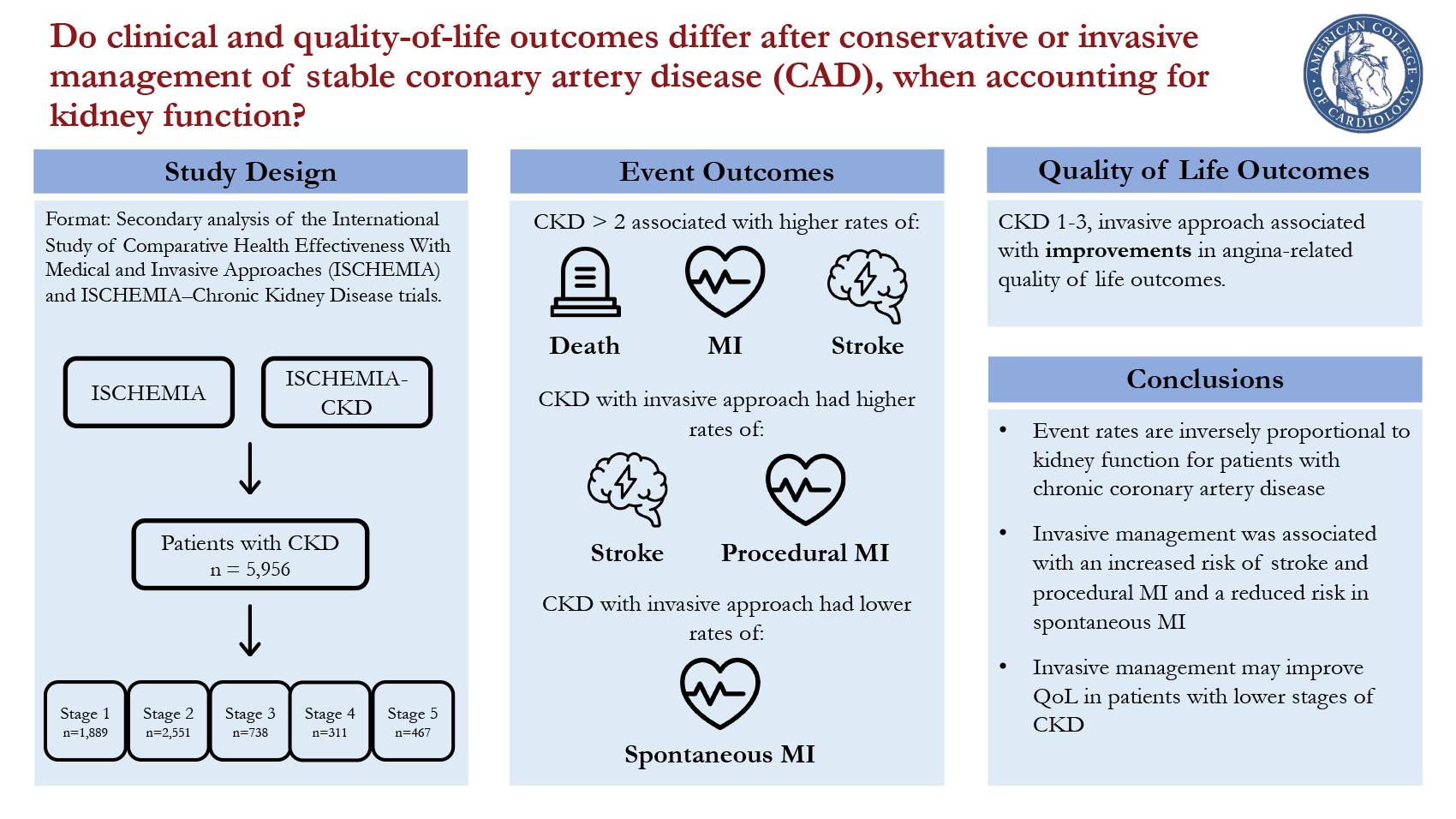
The 2022 paper, "Clinical and Quality-of-Life Outcomes Following Invasive versus Conservative Treatment of Patients With Chronic Coronary Disease Across the Spectrum of Kidney Function," assesses whether clinical and quality-of-life outcomes differ after conservative or invasive management of stable coronary artery disease (CAD), when accounting for kidney function.1 This study utilizes patient data from the International Study of Comparative Health Effectiveness With Medical and Invasive Approaches (ISCHEMIA) and ISCHEMIA-Chronic Kidney Disease (CKD) trials to determine whether the ISCHEMIA trial's findings can be recreated in patients with CKD.
Introduction
Since the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial in 2007,2 there has been a significant focus on how physicians should initially manage patients with known but stable CAD. This led to the ISCHEMIA trial, published in 2020.3
The COURAGE trial and the Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) trial both found that an initial conservative approach of guideline-directed medical therapy (GDMT) was non-inferior to an initial invasive approach of coronary angiography with revascularization if coronary anatomy was suitable, in addition to GDMT.2,4 However, these trials attempted to exclude patients with advanced CKD.
The COURAGE trial only enrolled 16 patients with an estimated glomerular filtration rate (eGFR) below 30 ml per minute per 1.73 m2 of body-surface area and the BARI 2D trial excluded patients with a serum creatinine greater than 2 mg/dL. The ISCHEMIA trial and its accompanying ISCHEMIA-CKD trial strengthened the past results of the COURAGE and BARI 2D trials, finding that an initial conservative approach had similar outcomes to an initial invasive approach in patients with stable CAD, even in patients with CKD.3,5
Methods
The point of this new post-hoc analysis, written by many of the same authors of ISCHEMIA and ISCHEMIA-CKD, was to evaluate clinical and quality-of-life outcomes across various stages of CKD following conservative and invasive treatment strategies.
In this analysis, ISCHEMIA and ISCHEMIA-CKD patients were categorized into different stages of CKD based on their calculated eGFR. Patients in these trials were randomized to either an initial invasive approach with coronary angiography and intervention if feasible plus GDMT or an initial conservative approach utilizing GDMT and only undergoing angiography and revascularization if GDMT failed. The primary outcomes were death or nonfatal myocardial infarction (MI) and the Seattle Angina Questionnaire (SAQ) score.
Results
There were 5,956 patients included in the study, with 32%, 43%, 12%, 5%, and 8% in CKD stages 1, 2, 3, 4, and 5, respectively. The authors found that patients with higher stages of CKD had higher rates of cardiovascular events, regardless of whether they underwent an invasive or conservative approach. A CKD stage higher than 2 was associated with higher rates of all-cause death MI, and stroke (stage 3: OR 1.54, 95% CI 1.24-1.91; stage 4: OR 2.86, 95% CI 2.22-3.68; stage 5: 4.14, 95% CI 3.32-5.15; p<0.001) with CKD stage 5 having a 10-fold higher risk of cardiovascular death than CKD stage 1. In patients with CKD assigned to the invasive approach, patients were less likely to have significantly obstructed CAD (p<0.001), and coronary revascularization was performed less often than patients without CKD (p<0.001). Additionally, in the conservative approach, patients with CKD had lower rates of meeting GDMT treatment goals.
Regardless of CKD stage, there were no differences between conservative and invasive approaches in primary clinical outcomes. However, the authors noted that the invasive approach had increased rates of stroke and procedural MI but lower rates of spontaneous MI. In the investigation of quality-of-life outcomes, based on self-reported angina scores, the authors found that the invasive approach was associated with improved self-reported angina scores, but only in patients with CKD stages 1 to 3. There was no difference in CKD stages 4 or 5.
Conclusions
Patients with more advanced CKD with stable CAD have higher rates of cardiovascular events. The only significant differences were an increased rate of stroke and procedural MI and a decreased rate of spontaneous MI in the invasive group, with similar effects in each CKD stage. The rates of death and death due to a cardiac cause were similar between the invasive and conservative approaches, which parallels the findings of the ISCHEMIA and ISCHEMIA-CKD trials.
Ultimately, the paper expands upon the ISCHEMIA and ISCHEMIA-CKD trials by analyzing CKD patients by the stage of their kidney disease. This study contributes to the growing discussion on the initial management of patients with stable CAD.
Limitations
This paper also includes a quality-of-life measurement surrogate in the angina questionnaire. The invasive approach was associated with improvements in self-reported angina in individuals with lower stages of CKD. There is a possible bias in this data collection. As the ORBITA trial revealed, patients can have a placebo effect when they believe they have undergone an invasive procedure, even if there was no stenting.6 While the patients in the ISCHEMIA and ISCHEMIA-CKD trials were not blinded to percutaneous coronary intervention (PCI) placement, it is possible that the invasive procedure could impact their self-reported scores.
Figure 1
References
- Bangalore S, Hochman JS, Stevens SR, et al. Clinical and quality-of-life outcomes following invasive vs conservative treatment of patients with chronic coronary disease across the spectrum of kidney function. JAMA Cardiol 2022;7:825-35.
- Boden WE, O'Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007;356:1503-16.
- Maron DJ, Hochman JS, Reynolds HR, et al. Initial invasive or conservative strategy for stable coronary disease. N Engl J Med 2020;382:1397-1407.
- Frye RL, August P, Brooks MM, et al. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med 2009;360:2503-15.
- Bangalore S, Maron DJ, Hochman JS. Management of coronary disease in patients with advanced kidney disease. N Engl J Med 2020;383:1091-92.
- Al-Lamee R, Thompson D, Dehbi HM, et al. Percutaneous coronary intervention in stable angina (ORBITA): a double-blind, randomised controlled trial. Lancet 2018;391:31-40.
Clinical Topics: Cardiovascular Care Team, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Stable Ischemic Heart Disease, Atherosclerotic Disease (CAD/PAD), Interventions and Coronary Artery Disease, Interventions and Imaging, Angiography, Nuclear Imaging, Chronic Angina, Dyslipidemia
Keywords: Coronary Artery Disease, Creatinine, Coronary Angiography, Glomerular Filtration Rate, Quality of Life, Conservative Treatment, Courage, Drug Evaluation, Renal Insufficiency, Chronic, Angioplasty, Physicians, Ischemia, Diabetes Mellitus, Percutaneous Coronary Intervention, Kidney, Angina, Stable, Goals, Placebo Effect, Self Report, Myocardial Infarction, Stroke
< Back to Listings