Poll Results: Call It What It Is! Inattention and Fluctuating Cognition in a 97-Year-Old With Heart Failure
In this poll, Mr. M is a 97-year-old male with new onset heart failure admitted to a skilled nursing facility post hospitalization with fluctuating mental status course, inattention, disorganized thinking, and altered level of consciousness. The results of this poll can be seen below:
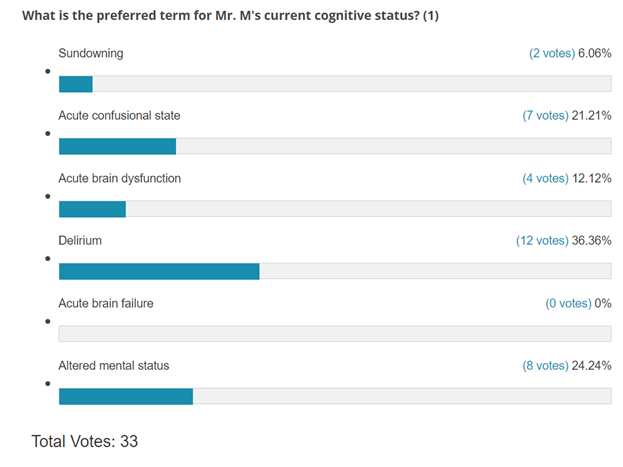
The first poll question addresses the optimal terminology when referring to patients with delirium. The heterogeneity noted is probably representative of real-life. Delirium is the optimal terminology in someone with cognitive features described in the vignette.
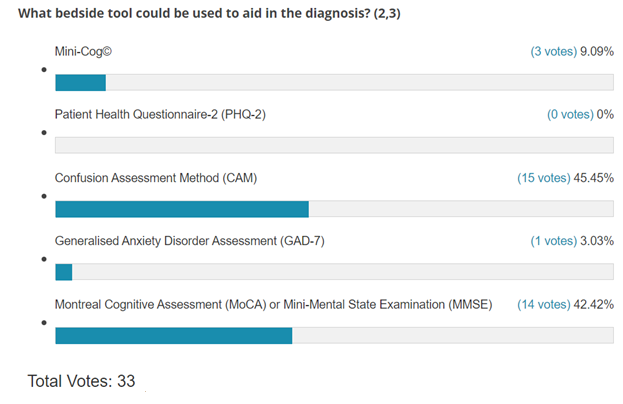
The second poll question addresses the optimal method of detection of delirium. The Mini-Cog© and the Montreal Cognitive Assessment (MoCA) or Mini-Mental State Examination (MMSE) are screening tools and tools respectively to assess for memory loss while the Confusion Assessment Method (CAM) is the optimal tool for detecting delirium.
The Mini-Cog© (administration time <5 minutes) is a screening tool for the assessment of memory loss consisting simply of three words that must be memorized, then recalled, after drawing of a clock with the hands at 10 minutes after 11 o'clock. The MOCA and MMSE are initial tests when cognitive dysfunction is suspected (administration time 15-20 minutes) used for the assessment of memory loss, mild cognitive impairment, and dementia.
The Patient Health Questionnaire-2 (PHQ-2) is a first step approach for screening of depression and consists of two questions that ask whether in the last 2 weeks, how often (not at all, several days, >half the days, nearly every day) has the patient been bothered by a. little interest or pleasure in doing things b. feeling down, depressed, or hopeless. The scores range from 0-6 and a score of ≥3 is suggestive of depression and further tests can be considered. The Geriatric Depression Scale (GDS) consists of 15 questions that have an increased sensitivity and specificity for depression in older adults. A score of >5 suggests depression.
The correct terminology for Mr. M's altered consciousness is DELIRIUM. Delirium derived from the Latin word delirare – 'to go out of the furrow' – deviate from a straight line, to be deranged. It is a severe neuropsychiatric syndrome characterized by acute onset of deficits in attention and cognition and is known to have multiple triggers with known variable duration (days-weeks-months [20%]). The confusing terminology (sundowning, etc.) has led to its substantial underdiagnosing at hospital discharge. Despite the description of delirium being known from Roman times, there has been little attention paid to it until the past 3-4 decades. Overall, research funding for delirium has been woefully inadequate with a large part attributed to the lack of consistent terminology. The statement of ten societies for the updated nomenclature of delirium states that the following terminologies should not be used: acute confusional state, acute brain dysfunction, acute brain failure. The report also states that altered mental status is not synonymous with delirium and should not be used.1-3
Clinical Follow Up
Mr. M was diagnosed with delirium based on CAM.4 CAM, initially developed by Dr. Sharon K. Inouye and team, is a bedside tool to aid in the diagnosis of delirium that focuses on four items (acute onset or fluctuating course, inattention [a hallmark], disorganized thinking, and altered levels of consciousness). The presence of delirium requires the first two and either disorganized thinking or altered levels of consciousness.
The etiology of Mr. M's delirium was dehydration due to poor oral intake, exacerbated by use of nectar-thick fluids, diuretic use for his heart failure. His furosemide was stopped, with a liberalization of his oral water intake to 1-1.5 liters and the institution of two intravenous normal saline boluses which resolved his delirium in 2 days. A subsequent MOCA completed 4 months after the initial presentation noted him to have a score of 24/30 suggesting mild cognitive impairment.
For additional information, read our piece Delirium: Take-Home Points For the Cardiovascular Clinician.
References
- Wilson JE, Mart MF, Cunningham C, et al. Delirium. Nat Rev Dis Primers 2020;6:90.
- Marcantonio ER. Delirium in hospitalized older adults. N Engl J Med 2017;377:1456-66.
- Slooter AJC, Otte WM, Devlin JW, et al. Updated nomenclature of delirium and acute encephalopathy: statement of ten societies. Intensive Care Med 2020;46:1020-22.
- Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med 1990;113:941-48.
Clinical Topics: Cardiovascular Care Team, Geriatric Cardiology, Statins, Sleep Apnea
Keywords: Aged, Furosemide, Saline Solution, Skilled Nursing Facilities, Consciousness, Patient Discharge, Follow-Up Studies, Dehydration, Mental Status and Dementia Tests, Delirium, Dementia, Diuretics, Geriatrics
< Back to Listings

