Top Three Late Breaking Clinical Trials in Sports Cardiology and Hypertrophic Cardiomyopathy from ACC.23
Quick Takes
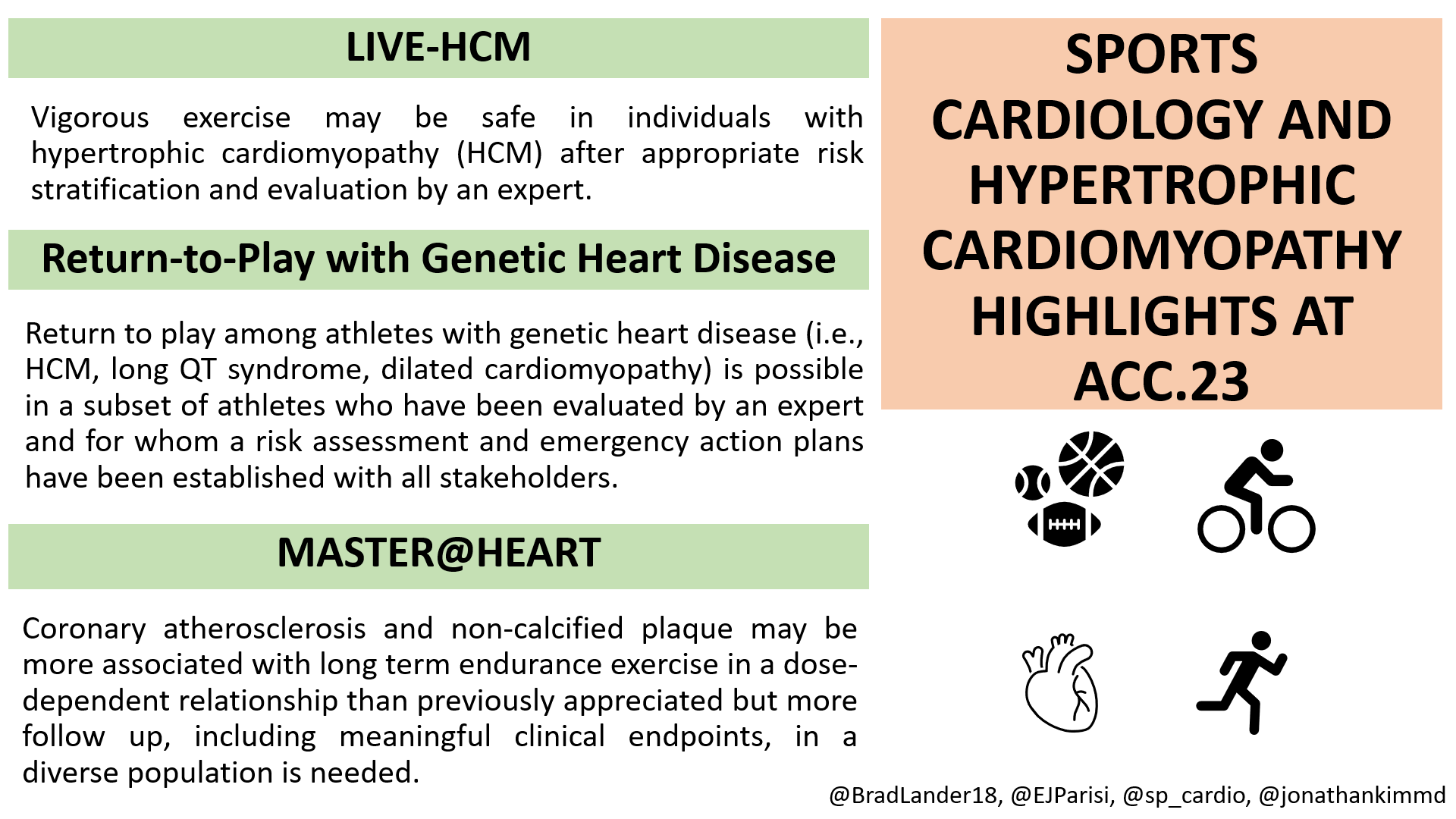
- Vigorous exercise may be safe in individuals with hypertrophic cardiomyopathy (HCM) who are evaluated and appropriately risk stratified by an expert.
- Return to play among athletes with genetic heart disease (HCM, long QT syndrome, dilated cardiomyopathy) is possible in a subset of athletes who have been evaluated by an expert and for whom a risk assessment and emergency action plan have been established with all stakeholders.
- The prevalence of coronary atherosclerosis and non-calcified plaque in long term endurance athletes may be higher than previously appreciated but more follow up, including meaningful clinical endpoints, in a diverse population is needed.
The 2023 American College of Cardiology Scientific Session Together With the World Congress of Cardiology (ACC.23) was particularly notable for those within the sports cardiology community as many key trials were presented that help inform the care of active patients and athletes with cardiovascular disease (CVD). We highlight the top three trials here.
LIVE-HCM
Dr. Rachel Lampert presented the results of the Lifestyle and Exercise in hypertrophic cardiomyopathy (HCM) (LIVE-HCM) study as a late breaking clinical trial. This study was done in collaboration with Drs. Michael Ackerman and Sharlene Day. The study examined whether vigorous exercise was associated with an increased risk of life-threatening ventricular arrhythmias and/or death among individuals with HCM. Among the 1,660 enrollees from 42 sites in five countries, 1,534 participants had overt HCM while 126 were genotype positive but phenotype negative. The vast majority of the cohort (78%) were ˃25 years of age, whereas 13% were 18-25 years old and 9% of enrollees were <18 years of age. The cohort was 90% White. Of the 1,600 participants, 675 (42%) were women. Exercise was categorized using the Minnesota Leisure Time Questionnaire. Vigorous exercise was defined as at least one activity with metabolic equivalents (METS) ≥6 for ≥60 hours per year (42% of the cohort), moderate intensity was defined as all activities ≥4 METs but <6 METs for 60 hours per year (43%), and those who did not meet criteria for moderate or vigorous were deemed sedentary (16%). Follow up consisted of surveys every 6 months for 3 years and the endpoints (which were adjudicated by the events committee blinded to exercise classification) were: death, resuscitated cardiac arrest, syncope (definitely or likely arrhythmic or undetermined), or appropriate shock from an implantable cardioverter-defibrillator (ICD), reviewed by two electrophysiologists. There was no significant difference in events between vigorous and non-vigorous exercisers (15.9 vs. 15.3 events per 1,000 person-years, respectively) nor were there significant differences in secondary/post-hoc analyses between vigorous/moderate/sedentary individuals. Importantly, all events occurred in those with phenotypic HCM and none in those who were genotype positive but phenotype negative. Whereas prior consensus documents have recommended against vigorous exercise in patients with HCM, this study provides a safety signal for vigorous exercise. Follow-up data on this cohort as well as a more detailed understanding of the exact phenotypes of these patients are needed to make a more generalizable recommendation. Specifically, the risk of physical activity of 6 METs (i.e., light jogging) may be different than the risk of competitive college or professional athletics. Furthermore, this cohort was predominantly >25 years of age and White whereas other studies have shown that college-aged and Black athletes have higher risks of death.
Take-Home Message: Athletes with HCM who are considering vigorous activity should be evaluated by cardiologists with significant experience in the evaluation, risk stratification and treatment of HCM, sports cardiology and shared decision making.
Return-to-Play with Genetic Heart Disease
A second late breaking clinical trial, Return-to-Play for Elite Level Athletes with Sudden Cardiac Death Predisposing Heart Conditions was presented by Katherine Martinez. This was a retrospective study of patients seen at four expert sports cardiology/HCM centers (led by Drs. Matthew Martinez, Aaron Baggish, Michael Ackerman, and Dermot Phelan) that reported outcomes of a return-to-play (RTP) protocol for elite professional and college athletes with genetic heart diseases (GHD). The study included 76 athletes (36% professional and 64% Division I college), of which 28% were women. The most common diagnoses were HCM (53%), long QT syndrome (26%) and dilated cardiomyopathy (7%). Of these athletes, 30% had an ICD and 55% had a pathogenic genetic variant. Within this cohort, 72% were initially disqualified but after comprehensive evaluation and risk stratification, 96% chose to RTP and 4% (three athletes) chose not to RTP. Four athletes remained disqualified by their teams despite having a medical clearance to RTP. In total, there were four non-fatal breakthrough cardiac events among three athletes.
Take-Home Message: This study demonstrated that elite athletes with GHD can RTP in a safe manner when the following contingencies are met: (1) adherence to prescribed treatments, (2) access to a personal automated external defibrillator (AED), (3) annual follow-up visits and risk evaluation by an expert cardiologist and (4) consistent communication with all stakeholders. Future prospective studies are underway (https://orccastudy.org/) to follow this cohort of athletes and others with similar GHDs. These data will continue to advance our understanding of the safety of sport with GHD.
MASTER@HEART
The MASTER@HEART study,1 a multi-centered, prospective, observational cohort led by Dr. Ruben De Bosscher, was designed to answer the central inquiry of whether a dose-response relationship exists between the duration of endurance exercise load and the absolute prevalence of calcified, non-calcified, and mixed coronary plaques. Prior studies focusing on coronary artery calcium (CAC) in athletes have highlighted a paradox. Specifically, when compared to sedentary controls, athletes were more likely to have a higher CAC burden and higher likelihood of more stable, calcified plaques, but reduced all-cause mortality and lower incidence of CVD. Somewhat contrary to these studies, the MASTER@HEART study found that White, middle-aged men who were lifelong endurance athletes had a higher burden of coronary plaque including non-calcified and mixed plaques, as well as proximal plaques with significant luminal stenosis, when compared to healthy controls. It should be noted that the study population and control population were overall healthier than their respective cohorts in prior studies. Those with classic cardiovascular risk factors were excluded, and all three groups (non-, late-onset-, and lifelong athletes) had higher aerobic capacity, compared to previous study populations. The critical limitation to this study lies in its generalizability given 100% of the participants were White men.
Take-Home Message: Although the MASTER@HEART study has nicely demonstrated that even those participating in lifelong endurance exercise are not immune to ischemic heart disease, future research is necessary to better explore these patterns across races and sex. Additionally, longitudinal cardiovascular outcome data as well as progression of plaque burden and characteristics over time are currently lacking and would provide valuable information if included in future studies. Importantly, given the absence of outcome data, we would not discourage high-level endurance exercise solely based on the results of this study.
Figure 1
References
- De Bosscher R, Dausin C, Claus P, et al. Lifelong endurance exercise and its relation with coronary atherosclerosis. Eur Heart J 2023;Mar 6:[ePub ahead of print].
Clinical Topics: Arrhythmias and Clinical EP, Cardiovascular Care Team, Congenital Heart Disease and Pediatric Cardiology, Heart Failure and Cardiomyopathies, Sports and Exercise Cardiology, Implantable Devices, Genetic Arrhythmic Conditions, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Congenital Heart Disease, CHD and Pediatrics and Arrhythmias, CHD and Pediatrics and Prevention, CHD and Pediatrics and Quality Improvement, Sports and Exercise and Congenital Heart Disease and Pediatric Cardiology
Keywords: ACC Annual Scientific Session, ACC23, Follow-Up Studies, Consensus, Cardiomyopathy, Hypertrophic, Syncope, Arrhythmias, Cardiac, Surveys and Questionnaires, Life Style, Phenotype, Genotype, Defibrillators, Implantable, Prospective Studies, Retrospective Studies, Return to Sport, Athletes, Death, Sudden, Cardiac, Heart Diseases, Long QT Syndrome, Patient Reported Outcome Measures, Prevalence, Incidence, Cardiovascular Diseases, Risk Factors, Plaque, Atherosclerotic, Myocardial Ischemia
< Back to Listings